When Transportation is a Barrier to Health Care
Many Americans lack access to reliable transportation, and research has shown that this can be a significant barrier to health care, particularly for low-income patients. According to one study, every year, an estimated 3.6 million Americans miss getting medical care because of lack of transportation. Missed appointments can lead to more severe and expensive medical conditions. According to one study, “… transportation barriers may mean the difference between worse clinical outcomes that could trigger more emergency department visits and timely care that can lead to improved outcomes.”
West Counties Health Clinic is located in western Sonoma County, a rural area of far flung and isolated communities. Over 80 percent of WCHC patients live at or below the federal poverty line and many are homeless. WCHC also serves a number of people displaced by the 2017 Tubbs Fire, one of the most destructive fire in California history. Many WCHC patients must travel long distances for medical care. Some patients don’t have access to a vehicle or a friend or family member who can reliably drive them. At the same time, bus service can be spotty and often involves long waits and travel times, which can be grueling for fragile patients. For very poor patients, gasoline and bus fare costs may also be prohibitive. Transportation is one of the top three social determinants of health (SDOH) affecting the WCHC patient population.

At WCHC, appointment no shows and late cancellations are a fact of life, according to Kathleen Figoni, the clinic’s innovation project manager. “Our clinic staff are constantly juggling schedules,” she says. “The lack of reliable transportation has a huge impact on our patients. Some are really sick: just walking into the clinic is hard, and riding the bus can be traumatizing.”
Missed appointments are also a drain on clinic resources. “You can walk into the clinic office and hear nurses on the phone with patients, trying to help them figure out transportation,” says Figoni. “They do a wonderful job, but it’s time consuming, and not the best use of their time.” According to one national estimate, missed medical appointments result in a staggering $150 billion in lost clinic revenue and staff time every year.
Hitch Health
The issue of how to improve patient access to reliable transportation was on Kathleen Figoni’s mind when she and other WCHC colleagues attended a Safety Net Innovation Network meeting in 2017 and heard a pitch by representatives of Hitch Health. Hitch Health, which was developed by the Hennepin County Medical Center in Minneapolis, is software that links clinic electronic health records to the rideshare service, Lyft.
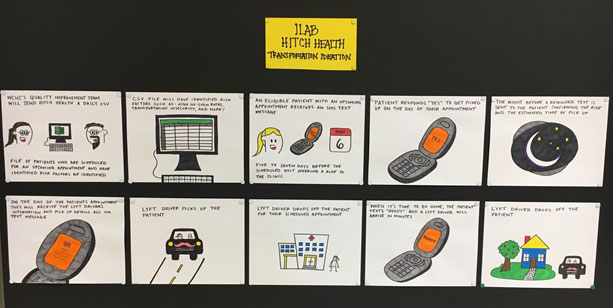
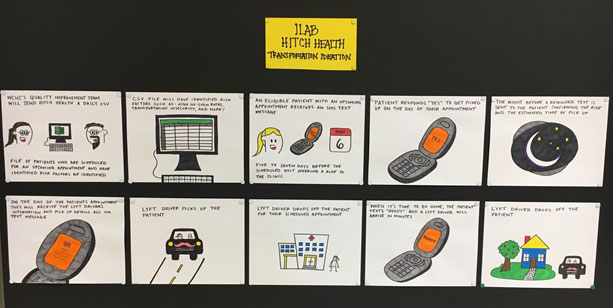
Hitch Health works like this:
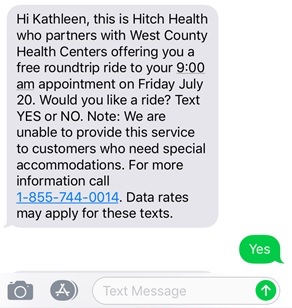
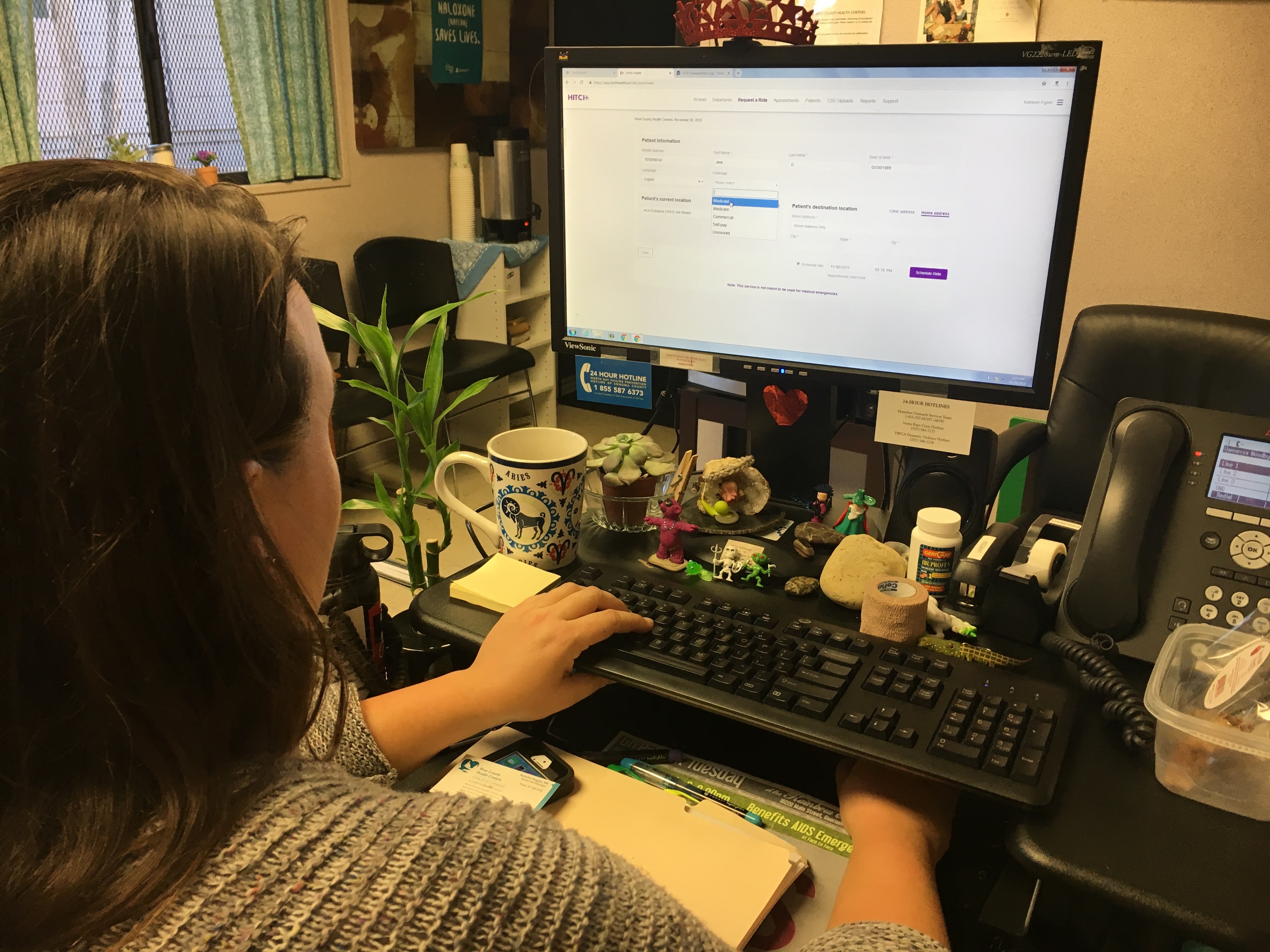
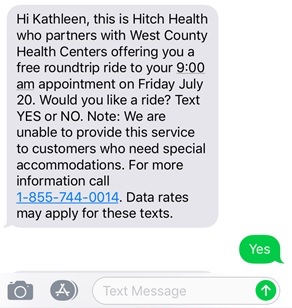
When a patient makes an appointment, they receive an SMS text message offering a ride to the clinic on the date of their appointment. (Patients do not need to have a smartphone to receive the messages, nor do the they need access to the Lyft app.) If the patient accepts the ride, they receive reminders, and are picked up and taken to their appointment at the scheduled time. The system also provides clinic staff with updates on when the patient will arrive. When the appointment is over, the patient texts again, and a driver comes to take them home. This process is automated and does not involve active management by frontline health center staff.
To Figoni and her colleagues at WCHC, Hitch Health sounded like a wonderful way to tackle transportation barriers facing their patients. With seed money from iLab, they teamed up with Hitch Health and began implementing the system in early 2018.
Getting to the Clinic On Time
To get started, WCHC created a project team made up of clinic administrators. The team held monthly meetings, beginning in January 2018. They enlisted the help of the WCHC’s Patient and Family Council, the clinic’s patient advisory group, and its input proved invaluable. A member of the patient group found the initial text messages confusing, for example, and recommended clearer language. Some other adjustments based on input from the Patient and Family Council:
- Text language was modified to take into account low literacy among some in the patient population (messages are currently in English; a Spanish version is in development).
- Hitch Health’s text messaging system was based on Central Time, so had to be converted to Pacific Time.
- If a driver is reassigned, patients are now alerted via text message.
- If a patient needs to cancel a ride, they can now do so by adding the message “No Ride” to the text message thread at any time.
 Seth Emont from iLab consulted with WCHC early in the process to help the Project Team develop qualitative questions to help them evaluate how the new system was working. iLab seed money was used primarily for patient rides.
Seth Emont from iLab consulted with WCHC early in the process to help the Project Team develop qualitative questions to help them evaluate how the new system was working. iLab seed money was used primarily for patient rides.
The Project Team also worked closely with Hitch Health representatives throughout the implementation process and continues to consult with them via weekly calls today. Since Hitch Health software was developed to meet the needs of urban patients (WCHC was the first rural clinic to try it) a number of adjustments had to be made. It also took some time to work out technical issues that came up as WCHC and Hitch Health coordinated their two different systems.
The testing phase took from January to July — far longer than WCHC anticipated, but it was valuable time because it gave the Project Team a chance to work out kinks in the system before they rolled it out for patients. They tested and refined messaging language, worked with Hitch Health representatives to create additional messages, and developed a script and trained WCHC’s call center staff so they could handle any problems that came up.
In July 2018, WCHC launched a one week test pilot at the Gravenstein Community Health Center near Sebastopol. The initial pilot included only patients from certain zip codes who were scheduled for primary care visits. That trial led to further refinements and more testing that varied from the text message content, to changing the how many patients were sent messages at time, to working with health center front office scripts for questions or requests about the program.
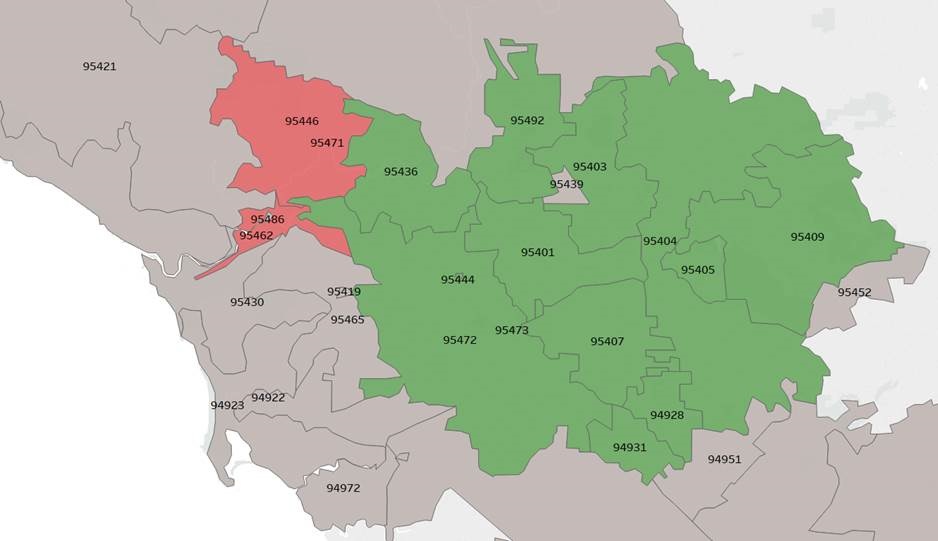
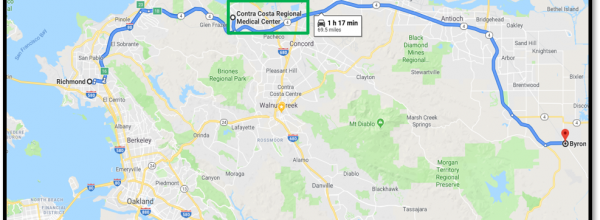
Patient response at the Gravenstein clinic was good, and the system seemed to be working well, so the project team decided to try implementing Hitch Health at the Russian River Health Center in Guerneville as well. This clinic is located in the most rural part of WCHC’s service area; it’s also where transportation insecurity is greatest. But it also turns out to be an area with very little Lyft coverage. Drivers are concentrated in Santa Rosa, which is 40 minutes from Guerneville. When the clinic tried implementing the ride system, Lyft drivers repeatedly cancelled scheduled pick-ups. “We learned quickly that the rural geography created significant barriers to Lyft access both in pickup and drop-off,” according to Kathleen Figoni. After a month of trying, WCHC decided to halt the pilot at the Russian River location.
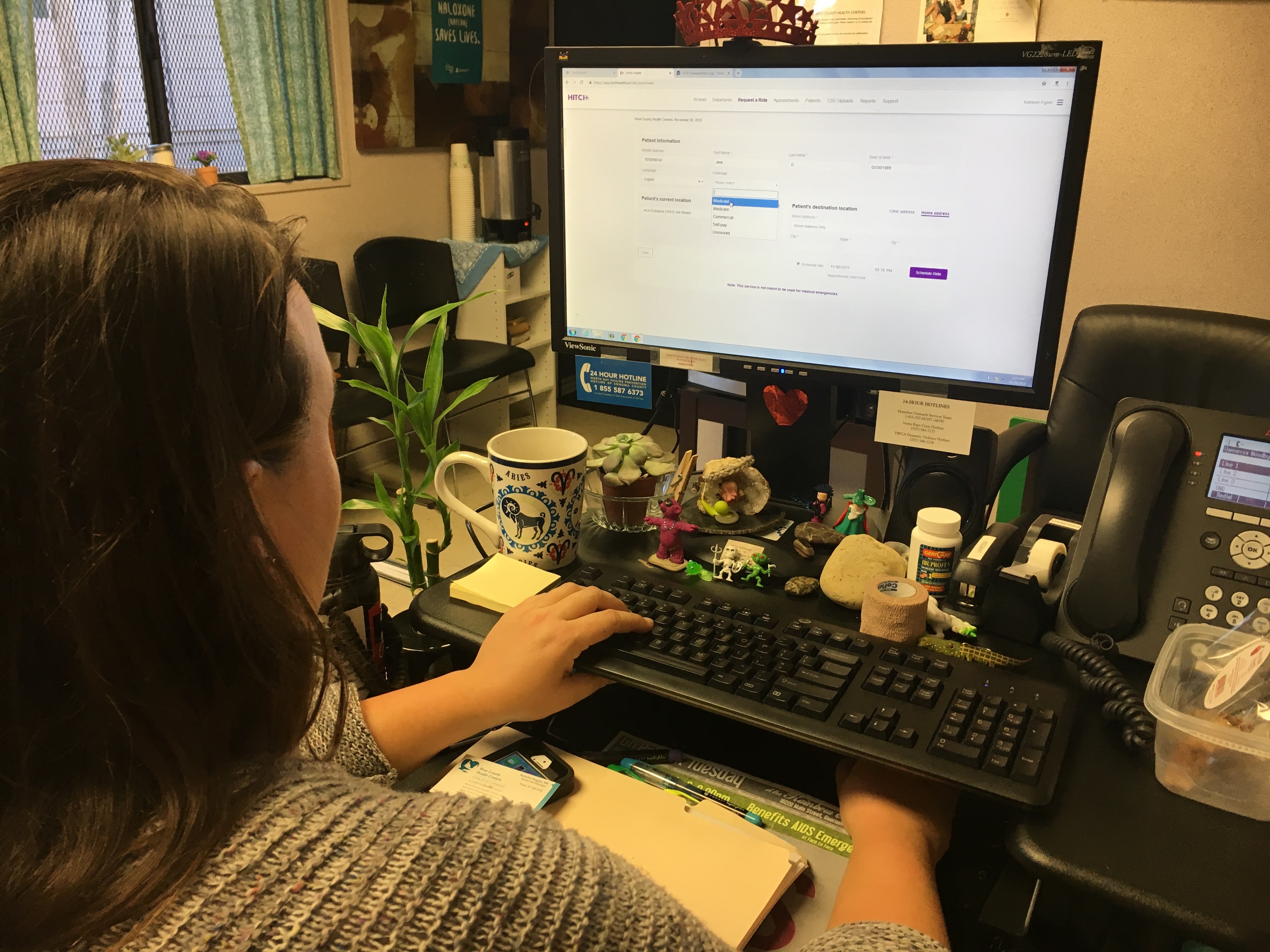
Meanwhile, when Hitch Health was piloted with WCHC’s Healthcare for the Homeless patients, it worked well. Healthcare for the Homeless outreach workers used an “On Demand” feature on the Hitch Health dashboard, which arranged for patients to be picked up immediately (instead of scheduling rides in advance). “Scheduling a ride or visit in advance with the homeless population is challenging,” says Figoni. “Requesting a ride when the patient was right there was far more efficient.”
WCHC is continuing to pilot Hitch Health at its Gravenstein Community Health Clinic, expanding the service to all visit types (i.e. not just primary care visits) and to patients in additional zip codes. WCHC is also testing a new Hitch Health feature that will allow homeless patients to schedule rides for specialty appointments two weeks in advance.
Results
WCHC is currently evaluating the Hitch Health initiative to see if and how much it has reduced patient no shows and late cancellations and to assess the patient experience. They are continuing to collect and analyze data to establish proof of concept and will have results in the next few months.
Some preliminary findings:
- Out of 2,096 patients with upcoming appointments who qualified for a Lyft ride (based on type of appointment and zip code) 56 (3 percent) accepted the ride invitation. Out of that number, 35 patients (62 percent) used the ride service to get to the clinic.
- Ride acceptance rates are increasing as the pilot progresses and more patients are familiar with the process and have had good experience. Allowing for this natural ‘ramping’ up process was a good lesson learned.
- Satisfaction with the service was high: When patients were asked how likely they were to recommend the ride service to someone else, on a scale of 0 to 10 with 10 being very likely, the average score was 9.9.
- 82 percent of patients found the service very easy to use.
- In interviews with WCHC staff, many patients who were asked what they would have done if the Hitch Health Service was not available said they would have cancelled their appointments; others said they would have taken a bus or taxi, gotten a ride with family or friends, or reschedules their appointment.
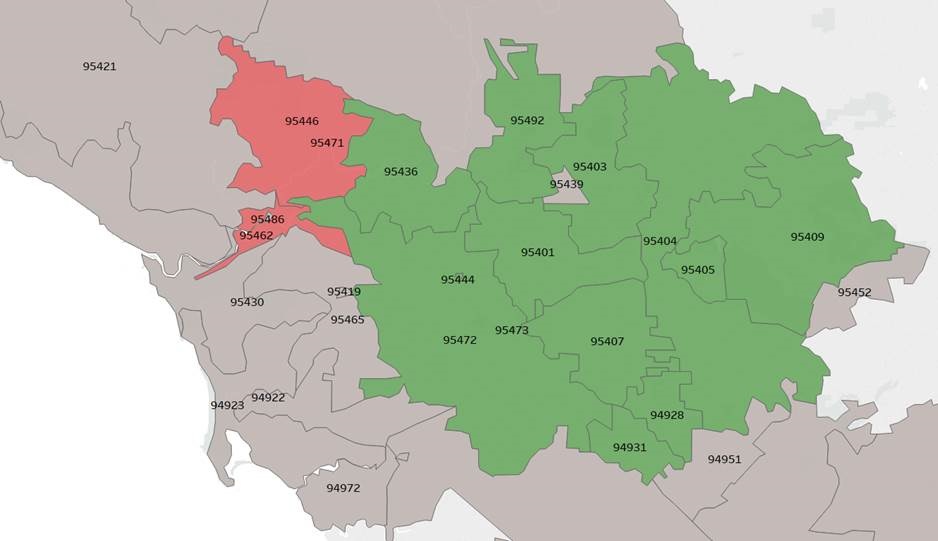
Green zip codes indicate successful roundtrip rides to and from clinic. Red zip codes indicate unsuccessful pick up and drop offs. Grey zip codes indicate zip codes in which WCHC has not offered rides.
One patient reported, “It’s awesome! My condition has resulted in loss of driving privileges, so Hitch makes it possible to get to appointments. Thank you!”
And another patient said, “If this service was not available I would have tried to get a ride with friends, I have part ownership of a car but can no longer drive myself due to my anxiety. Using this service was very easy and I like to get to my appointment early and that happened with this service! I would definitely use this again. The cars were immaculate, and taxis often smell and well, the bus can be downright traumatic, so as long as I can use this service I will.”
Clearly, a year into the project, Hitch Health is already helping WCHC eliminate transportation barriers to health care for some of its patients. Kathleen Figoni, who conducted extensive patient surveys about the program, says the biggest challenge is how to expand it. “Our patients love this service, and don’t want it to go away,” she says. “They are really hoping that this pilot remains sustainable and that we can do more. We’d like to expand it to all our clinics.”
For clinic staff, too, Hitch Health has shown benefits. “Using this technology has been useful for eliminating the staff role in managing transportation,” Figoni observes. “It has helped us put these arrangements directly into the hands of patients, so our nurses are freed up to do what they do best.”
Expanding the program to other areas and clinics won’t be easy. In many areas of western Sonoma, there aren’t enough Lyft drivers available to ensure reliable rides for patients. Figoni plans to meet with Lyft representatives to find out if there is a way to expand the service. She also plans to talk to a local taxi company that the clinic often works with to see if there are ways to expand that partnership.
But Figoni is hopeful that these obstacles can be overcome. “I can see how much value there is in this and it warms my heart; we’re making a significant impact,” she says. “It outweighs the hiccups that we’ve experienced along the way.”
Long-term viability and financial sustainability will be assessed based on measured reduction in no-show or late cancellation for scheduled office visits, partnership with health plans or other payors who have existing non-emergent transportation responsibility, and assessment of clinical impact on patients with transportation insecurity.




 Seth Emont from iLab consulted with WCHC early in the process to help the Project Team develop qualitative questions to help them evaluate how the new system was working. iLab seed money was used primarily for patient rides.
Seth Emont from iLab consulted with WCHC early in the process to help the Project Team develop qualitative questions to help them evaluate how the new system was working. iLab seed money was used primarily for patient rides.