Relationship-Centered Networks

Attendees mingle at CCI’s summit “From Collaboration to Co-Liberation: Reimagining Partnerships for Healing.” (Credit: Patanisha Alia Williams and team)
The way that we are connected and behave toward one another has never been more important.
What are relationship-centered networks? They’re a process by which organizations and community members come together to achieve shared health goals. “Relationship-centered” refers to building long lasting, strong bonds in partnership, coalitions, and collaboration across CCI’s “networks” which include community health centers, community-based organizations, government agencies, multisector partnerships, and individual community members.
We understand that health care services alone will not achieve health equity and justice. As much as 80 percent of what influences health — such as zip codes — operates outside the four walls of the clinic. And studies have found improved health outcomes when health systems partner with community-based organizations to provide social services.
CCI is making a commitment to support the safety net by nurturing relational connections across the health ecosystem so that we can address the root causes of health disparities. We’re supporting organizations in a variety of ways — helping them hire more care coordinators and community health workers, provide integrated care, train staff in trauma-informed care, and more — so that they can better work with communities towards a brighter tomorrow.
We at CCI believe:
- Building relationships is vital to building community power.
- We advance health equity and justice through developing relationships based on trust, dignity, and respect instead of transactions.
- A longer-term view is necessary to understand relationships between partners, including why they may have failed in the past and how we move forward better together in the future.
- Healthy relationships and strong bonds are built on an understanding of power, intention, and deep listening to what community needs and wants.
Here’s what we learned in 2023:
Becoming a healing organization

Sherry meets regularly with therapist Alvin Fong at the Chinatown Service Center in downtown Los Angeles. (Credit: Harrison Hill, CHCF)
Sherry hadn’t seen a doctor in years when she first stepped foot into Chinatown Service Center. The pandemic, a change of residence, and her six-day-a-week job as a housekeeper made it too difficult. But there was also something else: The 32-year-old was spiraling into depression. During the visit, the mention of a Pap smear led to Sherry bursting into tears. Her primary care doctor had recently received training on assessing primary care patients for possible behavioral health needs, and Sherry’s screening score alarmed clinicians. But instead of simply giving Sherry a referral for behavioral health services, the health care providers did something better: They stepped right outside the exam room to find the center’s integrated service coordinator.
“Suddenly I had this person telling me I could get an appointment with a therapist very quickly and she was going to help me do it,” Sherry later told us. “Frankly, I had felt bad — at times suicidal, even — for a long time. I didn’t have anyone at all I could talk to about this. But that first day I thought, okay, there’s some hope. There’s someone out there who might be able to actually help me.”
The position was made possible by a CCI program that helped community health centers expand and improve behavioral health outcomes with a specific focus on advancing health equity and aligning behavioral health and social needs resources. The program has helped more patients access vital behavioral health services; in fact, Chinatown Service Center realized a 50 percent increase in annual referrals from the medical department to the behavioral health department, and primary care doctors now successfully complete a depression screening during 90 percent of visits (up from 74 percent).
This success story also contains a promising practice for CCI: To heal your community, you must heal yourself first. Relationship-centered networks require internal-facing work — creating stronger bonds within your organizations with your own colleagues. It’s about creating new roles with smooth “warm handoffs” between departments, fostering more communication, and creating all-staff trainings that get folks on the same page.
It’s a key lesson that’s been reinforced by another CCI program that is advancing pediatric care delivery models that are trauma- and resilience- informed so that young children and their caregivers have the support they need to be well and thrive. Take an inside look at UCSF Benioff Children’s Hospital Oakland where clinicians screen and treat people for “adverse childhood experiences,” or ACEs, as well as the upstream factors impacting health outcomes like domestic violence, food insecurity, and housing instability.
Through similar work, LifeLong Medical Care recognized that it was critical to create a caring environment for its staff through space for staff reflection and a support group for clinicians of color. Highland Hospital began prioritizing staff wellness. Robert Savio, MD, the former chief of pediatrics at Highland, said CCI’s learning collaborative helped strengthen rapport and trust among his coworkers:
“It has helped us rebuild in the backdrop of a global pandemic, where I think our clinic bond was maybe disintegrating a little bit because of masks, because of routine time, because of not looking at each other in the eye. Having intense emotional tearful discussions – this has brought us back as a team.”
Growing those collegial relationships within their organizations is what has allowed health centers to show up as better partners to both patients and community-based organizations. The Children’s Health Clinic reminded us that the people who are closest to the problem are also likely closest to the solutions. As one California clinic employee told our program evaluator, “Everybody a patient sees in a clinic has the potential to affect their appointment, whether that’s the front desk folks, the actual provider, the nurses. Everybody has a role to play. You don’t have to be a therapist to be therapeutic.”
And echoing our work in behavioral health, CCI discovered that integrating a dedicated person to help ensure both staff and patients have the support they need at all phases of ACEs screening — Community Medical Centers tapped a bilingual case manager and Bay Area Community Health Center recruited a pediatric care coordinator — not only smooths the screening administration, but that clinic role can also identify and provide connections to community resources and services. Tracey Hessel, MD, the associate medical director at Marin Community Clinic, told us:
“This program has really transformed the way I look at my work, partly because I feel so much more embedded in a team, a team that’s really looking at not just the whole child, but sometimes the whole family. That feels really hopeful to me, and it feels like so much more than when we were focused on illness. And we’ve got to do that too, but I think this broadening of the scope of what we do is much more powerful.”
Reimagining partnerships
When it comes to multisector partnerships, a lot of energy is focused on developing technical and tactical skills for a diverse set of organizations serving the community — boosting the “multisector” part of the equation. But what about the “partnerships” piece? In 2023, CCI began demonstrating that relationship work is a critical part of systems change and community health transformation.

Zhonnet Harper of Alameda Health System hugs Lisa-Marie Riley of the County of Marin Health and Human Services. (Credit: Patanisha Alia Williams and team)
As we wrapped up our program on strengthening partnerships that prevent domestic violence — reflecting on the lessons learned of this learning collaborative, then hosting a summit to bring those key findings to the community — we discovered this: It’s not just the work that is important. It’s how you do it.

Mindfulness coach and public health leader Jenée Johnson leads the group in a stretching and breathing exercise. (Credit: Patanisha Alia Williams and team)
At the partnership summit, community leaders talked about the importance of transforming the way clinics and non-profits approach their work. They urged partners to listen, to give community members a seat at the table, and to build relationships. “Suffering is universal,” said Jenée Johnson, a program innovation leader at the San Francisco Department of Public Health. “But we need to remember that pain and sun lead to growth and connection.”
In fact, too much emphasis on the work itself rather than the way it is carried out can be destructive, cautioned Johnson. A laser focus on productivity, Johnson said, “can show up as workaholism and a lack of empathy…So the work is to transform your organization first. Because you can’t give what you don’t have.” She recommends creating formal and informal “healing spaces” to foster social connection and psychological safety — and involving clients and patients in problem-solving.

Participants use sticky notes in an activity about the way we “mask” ourselves in our work lives. (Credit: Patanisha Alia Williams and team)
Timiza Wash, chief program equity officer of equity and transformational change at WEAVE, advised attendees to abandon “the super-hero complex” and lead by listening to youth, adult allies, and community members. “Connect with people who don’t know they can be changemakers,” she concluded.
To build successful, healing partnerships, our program participants proved that it’s key to invest time upfront to develop a deep understanding of each other and shared values, beyond organizational roles. Participants urged their partners to add value, not extract value. We learned that embracing vulnerability, transparency, and honest communication is a daily practice. And while it’s important to take creative risks and try new ways of working together, we must also give each other the opportunity to navigate setbacks and challenges.
As Emma Fay, a program coordinator at the Community Action Partnership of San Luis Obispo County, told CCI’s summit attendees: “Collaboration moves at the speed of trust.”

Fireside Chat panel on building relationships, left to right: author and therapist Colette Reid-Horn, Timiza Wash of WEAVE, Emma Fay of Community Action Partnership of San Luis Obispo County, and Lisa-Marie Riley of County of Marin Health and Human Services. (Credit: Patanisha Alia Williams and team)
That’s why we’re excited about CCI’s latest endeavor as an implementation partner on a California-wide initiative that’s working to advance population health management capabilities in order to eliminate health disparities and improve the health of people and communities. We’ll be taking what we’ve learned about relationship-centered networks into a new collaboration with 32 community health centers, Regional Associations of California, California Primary Care Association, Department of Health Care Services, and Kaiser Permanente. Through this initiative to transform care for Medi-Cal beneficiaries, CCI will be able drive our strategy forward by continuing to build upon foundations we’ve already laid with community health centers. Over the years, CCI has made a name for meeting organizations where they’re at and helping them figure out what they need. We’ll continue to encourage and foster a knowledge sharing culture, so that no one has to go it alone — or reinvent the wheel.
Making connections by thinking outside the box

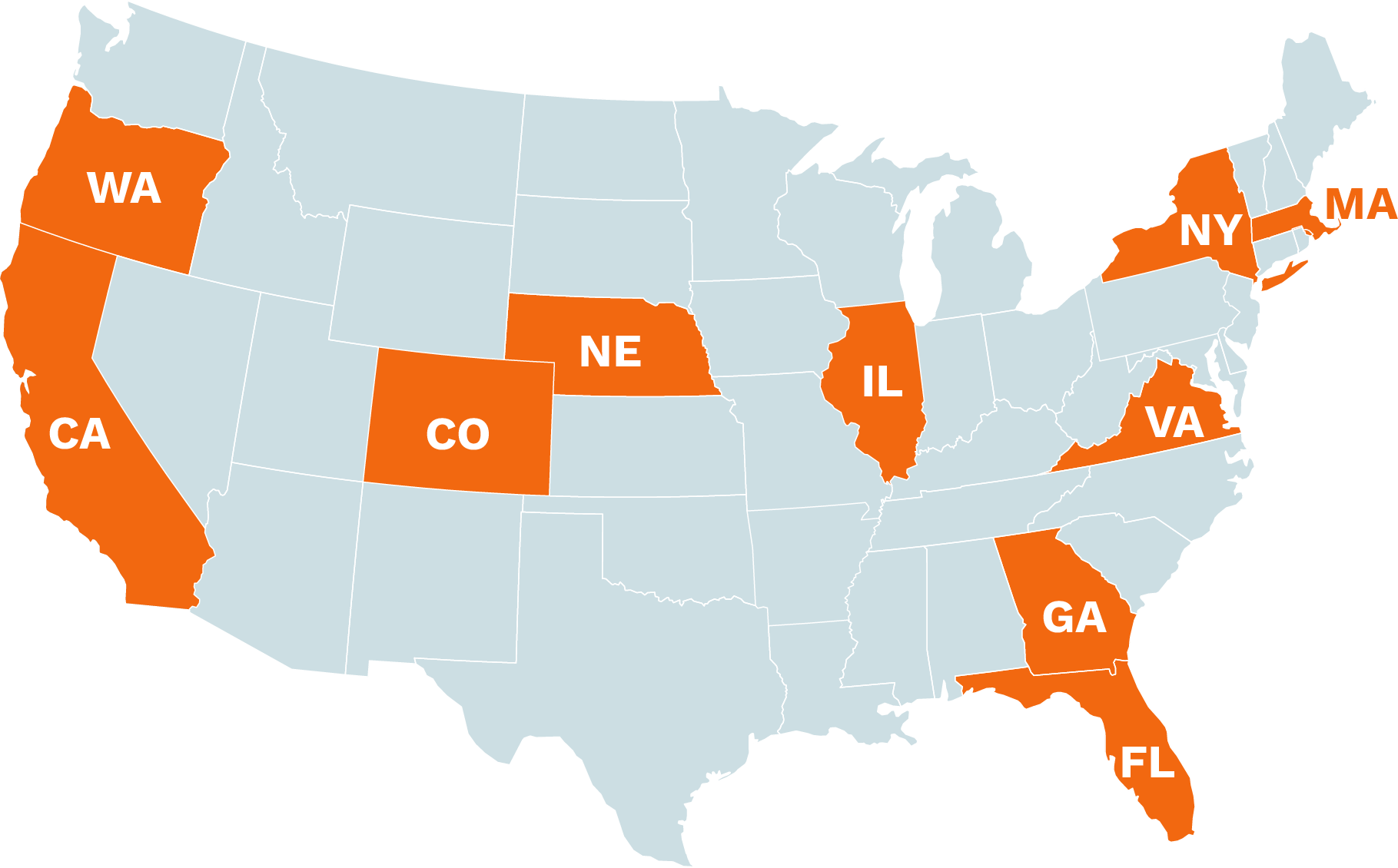
Over the summer, CCI and our partners helped resurrect the spirit of our previous innovation summits at “The Crossroads” in Chicago. With our co-hosts AllianceChicago and ILN, we asked safety net leaders — hailing from Illinois, California, Florida, and more — how we might turn onto the road less traveled: How might we take the best of these recent pandemic experiments and innovations and apply them to our most current challenges? How might we use creative destruction to let go of elements that are not needed? Most importantly, how might we birth new ideas and approaches to improve all our health? To inspire attendees, we took them on field trips to see the inner workings of cutting-edge organizations facing similar challenges — but outside of health care. The idea is that if you can break out of your usual workflow and toss out convention, it’ll kickstart your creative thinking and insight gathering. A fresh perspective is often what it takes to find the right answers to the problems you’ve been contemplating.

CCI’s Weslei Gabrillo and Jessica Ortiz in Chicago with AllianceChicago and ILN. (Credit: CCI)
At a first-of-its-kind convening this past fall, CCI and our collaborators brought together Medi-Cal managed care plans, health care providers, and community-based organizations from across California to swap insights, share innovations, and develop ideas for boosting uptake of Medi-Cal’s ambitious new enhanced care management (ECM) benefit, launched as part of CalAIM. At this hands-on learning event, attendees celebrated successes, troubleshooted roadblocks, and shared stories to spark new ideas around this major effort to coordinate and pay for non-traditional health care services like food and housing. Moreover, CCI introduced human-centered design approaches to help attendees learn more about what CalAIM implementers are experiencing today and to reimagine what is possible going forward.

CCI hosts a first-of-its-kind CalAIM gathering of Medi-Cal managed care plans, health care providers, and community-based organizations from across California (Credit: CCI).
One of our tools was “journey mapping” — a fun, insightful activity that helped attendees identify and strategize around key touchpoints in the community-based referral process. Belén Arangure, the ECM program manager at Northeast Valley Health Corporation, said, “It wasn’t until I began collaborating with other ECM providers outside of my organization that things began to really click.” Kristy Garan-Martinez, senior director of ECM at Inland Empire Health Plan, told us, “I feel like I can phone a friend when I’m in need of sharing thoughts and to discuss how to operationalize guidance from the state and how to overcome barriers.”
Throughout its 2023 convenings, our addiction treatment program has worked to braid together work on partnerships, equity, and medications for addiction treatment (MAT) care. We’ve introduced our program participants to “systems thinking,” way of making sense of the thorny, seemingly intractable challenges by looking at them in terms of relationships, as well as polarity mapping exercises (mapping of common tensions), which have deepened partnerships between clinics and community-based organizations by helping them figure out why partners can end up becoming accidental adversaries over a particularly vexing issue (and how to fix it).

CCI’s Kristene Cristobal and UCSF’s Dominque McDowell engage in an indigenous tobacco tie ceremony. (Credit: CCI)
Another approach our participants have learned from an indigenous participant is “yarning,” an Aboriginal Australian approach to giving and receiving knowledge that centers narrative and emphasizes deep listening without judgment, mutual respect, and sharing your own story.
And in the last few weeks of this year, CCI and our co-host Community Clinic Association of Los Angeles County invited street medicine teams across Los Angeles to a “design dash” — a super-fast introduction to design thinking methods and mindsets — that explored how we might keep street medicine patients connected to care. Belly laughter could be heard rippling throughout the event — a clear indicator that this new way of working was successfully bringing people together and sparking joy. One attendee told us, “We completed more here in one day than an entire year of collaborating remotely.”

Wendi Vierra of Neighborhood Healthcare takes our program participants on a tour of its integrated behavioral health program. (Credit: CCI)
Digital Transformation
Digital transformation is the integration of technology into all facets of health care.
This was given a boost during the COVID-19 pandemic, which upended the health ecosystem, expediting the use of digital tools in patient visits, clinical decision support, administrative systems, and more.
Today, CCI is guiding the safety net through this monumental technological shift. Providers working with us have used telehealth to shrink the digital divide and care for patients in remote rural areas. They’ve reduced patient travel and wait times. Many have reported improving their efficiency without higher net costs, while offering comparable or even improved quality of care. And others are thrilled with the ability to offer urgently needed online counseling sessions to people struggling with addiction, depression, and other conditions.
Moreover, we worked to capture and broadcast these stories in print, podcasts, and video, especially since we’ve found storytelling is a great way to speed adoption and adaptation. Our mini-documentary about the Community Clinic of Maui (Malama I Ke Ola Health Center), where CCI’s support helped add a nurse to its street medicine team that uses telehealth to connect unhoused patients with physicians back at the clinic, beamed around the globe in 2023. The video took home statuettes and plaques for six international media and film prizes, including two Telly Awards. (We were grief-stricken about this year’s horrific wildfire in the town of Lahaina, which the clinic serves.)
We at CCI believe:
-
-
- Accessing health care shouldn’t be so much work!
- Community members must have a place at the table.
- Safety net providers are in a unique position to demonstrate the role of digital tools to address the deep inequities in health and well-being.
- Staff satisfaction and retention will improve with successful adoption of digital tools, resulting in better services for patients.
Here’s what we learned in 2023:
Increasing availability and accessibility
This year we learned that digital tools are allowing the safety net to deliver more value to community members — specifically helping historically underinvested and marginalized populations more quickly and easily get the care they need.

CCI’s Elkin Salinas, Maria Garcia, Isabella Chavez, and Jessica Ortiz discuss desktop medicine with Jasper Lin of Neighborhood Healthcare. (Credit: CCI)
Looking for inspiration for how to improve and grow virtual visits? Check out our Virtual Visit Journey Map, where you will find helpful resources for each step along the patient journey. As our health system continues to adapt to virtual care, our team has worked with CCI program participants to compile resources for this unique tool that helps you better engage your patients.
In 2023, one of those CCI programs was a testing ground and support for California organizations to rapidly design, test, scale, and share new strategies to improve equity in access to telehealth. We learned that when it comes to factors that influence telehealth equity, many opportunities fall on the provider side of the equation. We need workflows that screen patients for digital barriers and incorporate all the virtual options they can choose from for visits appropriate for telehealth. Closing the gap requires rolling out technology platforms that are actually easy for patients to use, and we need to provide support to both patients and providers who face language or technology challenges.
As a complement to that virtual care work, we also grew a national community aimed at expanding access to video visits, particularly for people who have experienced economic disparities, housing and food insecurity, institutional discrimination, or violence. Though video visits are not the solution to achieving health equity, they do have the potential to break down barriers to care and enhance health care delivery. You can read all about it in our Accessible Video Visits Guidebook, a digital learning tool designed to introduce users to practical changes, how-to’s, and checklists to increase video visits. There we’ll introduce you to telehealth experts — all from the safety net, many of whom have piloted solutions powered by previous CCI programs — and tools from the field to identify provider-and patient-centered innovations.
Our work in revamping digital workflows also appeared when CCI partnered on a California multimillion-dollar “test to treat” program that supported and guided providers in how to speed delivery of lifesaving COVID-19 medicines. With the major investment from the government to expand access to treatment for COVID-19, we at CCI wanted to make sure the investment also served to support digital transformation that strengthened primary care overall. Today, participants are leveraging new workflows to facilitate access to care for other conditions and diseases.
For instance, Nobility Health ensured that 100 percent of its staff were trained in the new electronic health record system, then migrated all its historical processes and documentation into the new system. They worked to strengthen digital workflows, creating a process to ensure clinical staff would contact patients within 24 hours of a positive COVID-19 test. That increased the number of qualified patients who received therapeutics within 48 hours of a positive COVID-19 test to 70 percent (up from 40 percent). By the end of the program, Nobility used this model to incorporate screenings for Hepatitis C and sexually transmitted infections screenings including HIV and syphilis.

Nobility partners with numerous local organizations to bring more testing services into the community. (Credit: Nobility)
Reducing Administrative Burden
One of the major sources of burnout in the health care workforce is the staggering pile-up of administrative tasks — scheduling, charting, reporting, patient communication, and more. Digital tools have demonstrated major efficiency boosts and reduced burden on staff in many health care organizations. That said, many organizations in the safety net are only starting to explore the potential of digital tools to reduce the administrative and cognitive burden — freeing up staff to spend more time with patients online and in person.
This has been a major focus of a CCI program that helps safety net health systems to vet pilot, evaluate, and spread innovative digital health solutions. Altura Centers for Health sought to make the referral management process as self-sustaining as possible, so it introduced automated solutions.
COVID-19 testing and vaccines sent a large influx of people to Contra Costa Health Services’ patient portal. And because we’re all only human, it also triggered a huge number of password resets. Contra Costa’s small staff couldn’t support the volume of reset queries, and when it outsourced that support to a third-party, every one of those phone calls cost $20. So it launched an AI digital assistance program. Contra Costa saw how it could deflect as many as 80 percent of the password reset calls by offering to send text messages directing folks to where they could reset it themselves, rather than waiting on hold to talk to somebody that would essentially do the same thing.
This came with a number of benefits for the patient as well. Matt White, director of innovation at Contra Costa, said, “We could now offer self-service, offer service outside of hours of that call center. We allowed people to be empowered and to help to participate in their health, to learn about tools that maybe they hadn’t known were available before.”
CCI’s innovation community in Colorado is making similar strides. Along with an in-person translator, Gunnison Valley Health found online interpretation for Latino patients who speak Cora, an indigenous language from Mexico. Patient testimonials for included this note: “I want to thank the hospital for all the support, the translators are excellent, beautiful people with human warmth.”

Multilingual patient navigator Cinthia Saenz helps Spanish- and Cora-speaking patients with everything from appointments to billing. (Credit: Gunnison Valley Health)
Northwest Colorado Health, which covers a vast area the size of Delaware, Rhode Island, and New Jersey combined, began helping all eligible patients fill out financial aid forms — and integrated the application process into the center’s systems so that it can continue regardless of employee turnover. And WellPower and Jefferson Center recently completed a promising pilot with an AI documentation assistant that turns behavioral health conversations into clinical insights — one that might later free up providers to focus less on notetaking and more on delivering high-quality patient care.
At the same time, we’ve learning from what’s not working. Pueblo Community Health Center found creative ways to better serve its deaf and hard of hearing patients. To create real-time closed captions at reception stations, staff experimented with tablets loaded with speech-to-text software; but with transcription inaccuracies, data security worries, and battery life issues, it turns out patients are more responsive to simple, low-tech white boards and markers. As one receptionist team member told us, “If I had known it was this easy, I would have asked for these a long time ago!” Among those grateful for the change was a patient who once spent three days in terror after she misheard a doctor say she needed to go to a “hospice” instead of a “hospitalist.”
These are just some of the highlights of our year — jump to our “Keep Exploring” section to dig into all our storytelling from 2023!





![Colette Reid Horn_Amplify-Healing-Connections-event [1]](https://www.careinnovations.org/wp-content/uploads/Colette-Reid-Horn_Amplify-Healing-Connections-event-1-2-300x225.jpg)






![Street medicine teams_CCI collaboration [1]](https://www.careinnovations.org/wp-content/uploads/Street-medicine-teams_CCI-collaboration-1-2-225x300.jpeg)