Key Challenges
Long cycle time, lack of access to data at the point of care, paper-to-electronic transcription errors
Q: What was the problem your organization was grappling with?
A: The “cycle time” begins at the time of arrival and ends when the patient leaves the office. At NEVHC, a patient should expect to spend an average of 89 minutes at their office visit based on data calculated in the third quarter of 2014. For adults, the average cycle time was even longer at 111 minutes. Our cycle time goal has been established at less than 60 minutes.
In addition to a long cycle time, data from screening tools was not always available to the provider at the time of the visit. Therefore, a patient with a positive depression screen might be missed during the visit and would then have to be recalled. And lastly, errors occurred when transcribing data from a paper screening into an electronic template, and scanning PDF documents does not allow extraction of results.
Q: How did you learn it was a problem? And why was it important to address?
A: Results from the Pulse One-Minute Survey (POMS) conducted at our Sun Valley Health Center indicated that patients were not satisfied with the cycle time at NEVHC. They clearly expressed dissatisfaction with the total amount of time it takes to see a provider and complete their visit. We also know from our annual Patient-Centered Medical Home (PCMH) Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey from 2012 and 2013 that approximately 40 percent our patients said they see their provider within 15 minutes of their appointment time. Based on these surveys, NEVHC determined that we could greatly improve the patient experience if we could reduce the “waiting” time. This could be done by improving efficiency, and adding “value” to the wait time for the patient, provider, and care team.
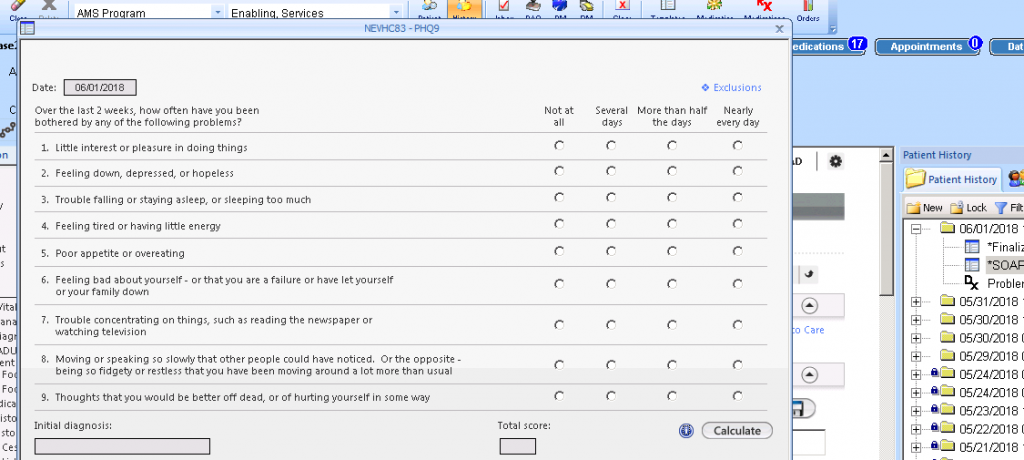
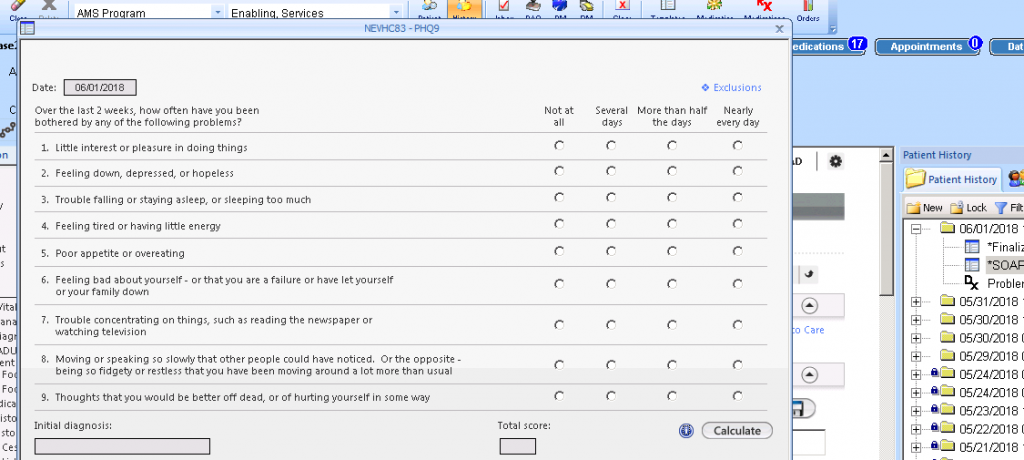
NEVHC also discovered that there were transcription errors when staff transcribed data from a paper screening into the electronic health record (EHR). A chart audit found that accuracy in transcribing patient responses from the paper PHQ9 (depression screen) was at 52.2 percent. Of the 23 chart audits, staff did NOT transcribe four PHQ9’s at all prior to the visit, a transcription error was made on two charts, and question No. 10 was left off the transcription of five charts. We also discovered that sometimes patients skipped a question and the scoring would be inaccurate.
Testing
Developing digital questionnaire templates and interfacing data into NextGen electronic health record
Q: Describe the solution you tested. How did you come to decide to try this solution?
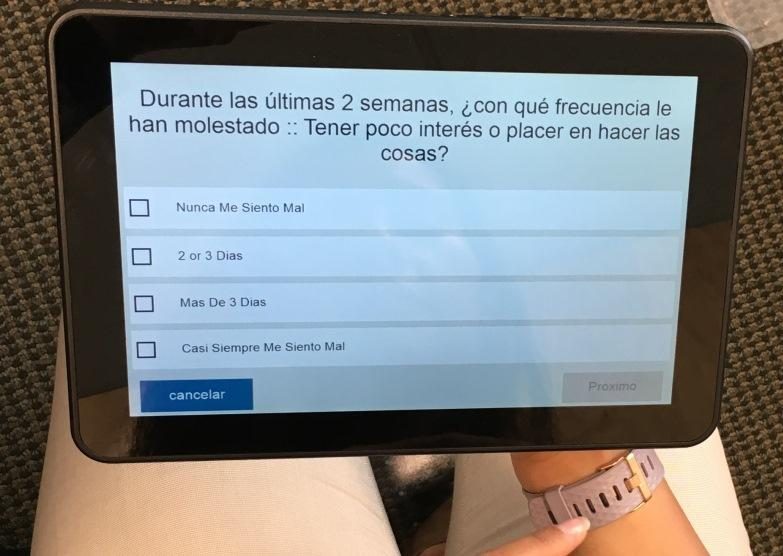
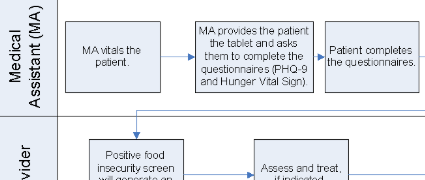
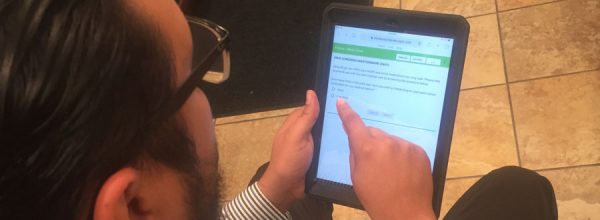
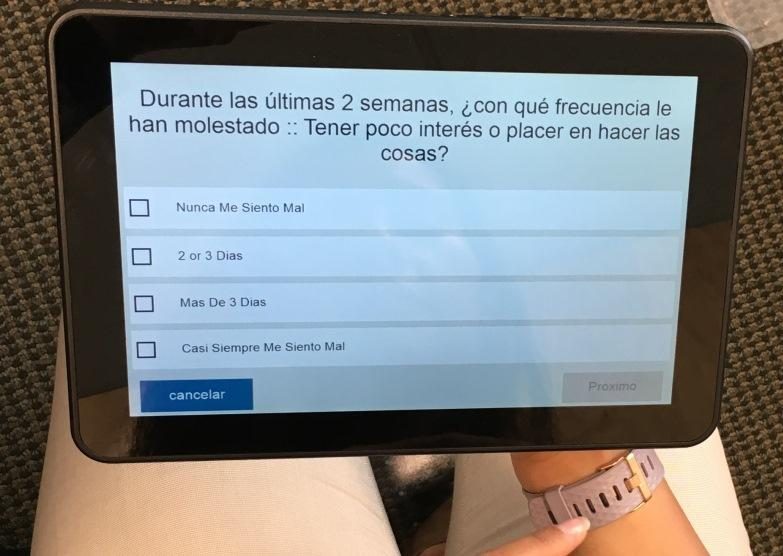
A: NEVHC tested Tickit in 2015 and 2016 to collect patient-entered data to improve the efficiency of the visit and to reduce cycle time. NEVHC started with one questionnaire with the ultimate goal of gathering data from multiple questionnaires prior to the visit with a provider. Tickit initially designed and re-created the PHQ9 to screen for depression utilizing user-friendly graphics and design to better serve vulnerable populations and patients with low literacy. The goal was to enable patients to answer the survey questions on their own to save time, eliminate the process of transcribing patient responses, and reduce potential data entry errors, therefore adding value to the time the patient spends with the provider and care team members. NEVHC implemented Tickit for the adult population at our second largest health center, Pacoima Health Center. Tickit was well received by patients and the care team, but after significant effort, we did not succeed in interfacing the data into NextGen, our electronic health record.
Unable to use the data in a PDF format, NEVHC abandoned the pilot and implemented another solution using OTech in 2017 and 2018. NEVHC was able to pilot the PHQ9 for one month to determine if the data from the PHQ9 would interface into the NextGen template. The one month trial was implemented for Adult Medicine.
Q: What structure did you put in place for the pilot? What eligibility criteria did you choose for the pilot, and why? What was the result?
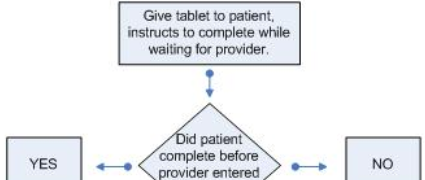
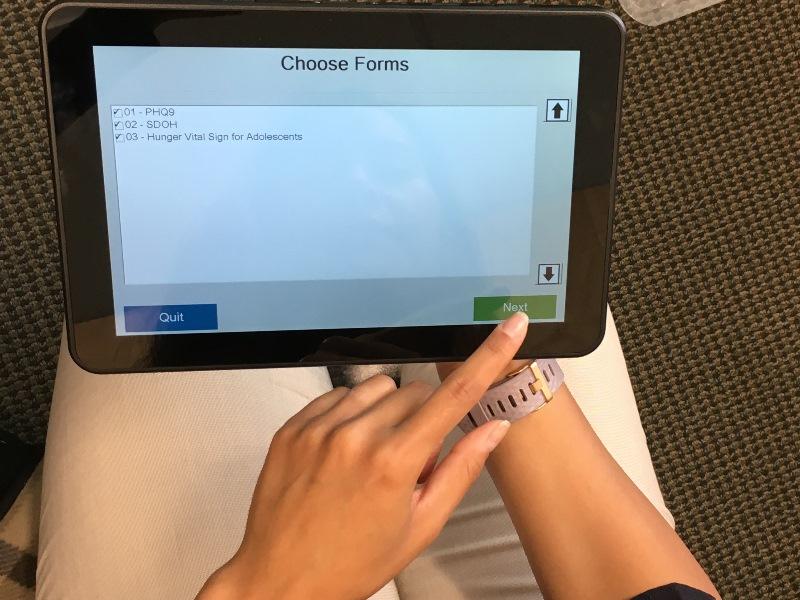
A: Following our initial one-month pilot at the Pacoima Health Center Adult Medicine Department, NEVHC spread OTech and the PHQ9 to Women’s Health and the Pediatrics Department. However, NEVHC experienced Wi-Fi and functionality issues with the tablets and chargers during the first year of implementation. Although staff and patients found that the tablet were easy to use, the technical issues had a negative impact on implementation, resulting in reduced staff buy-in. However, OTech has now swapped out the existing tablets for a higher-quality model and the previous Wi-Fi issues have for the most part been resolved.
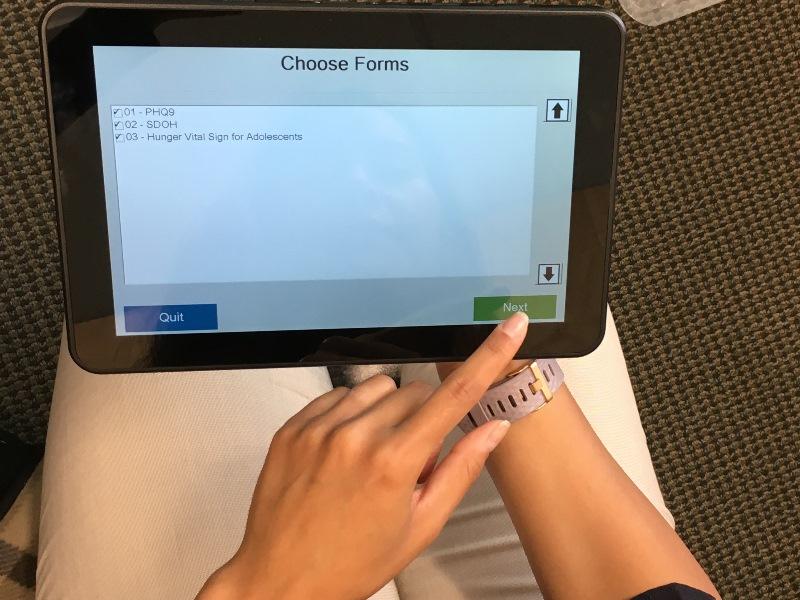
In February 2018, NEVHC was ready to implement our second screening assessment using the Hunger Vital Sign and PRAPARE tools. Work first needed to be completed on the NextGen template, enabling us to pull social determinants of health (SDOH) / Uniform Data Sytem (UDS) data from other NextGen templates. Implementation of the Hunger Vital Sign began at the Pacoima Health Center with the 12- to 17-year-old population since they were already using OTech for the PHQ9. Our patient navigators and behavioral health care coordinators also began using OTech for the PRAPARE pilot in April 2018. As we spread the PRAPARE tool to other health centers we did experience Wi-Fi issues, but most have now been resolved. In May 2018, NEVHC spread OTech to our Valencia Health Center with both questionnaires. A total of 36 staff members are currently using Otech for up to three questionnaires.
Q: How does OTech work today?
A: NEVHC just began the second year of implementation utilizing 40 tablets. Functionality of the tablets has improved significantly, and we are no longer experiencing the technical challenges identified in the first year. We have spread the PHQ9 pilot to all disciplines at the Pacoima Health Center and have added the Hunger Vital Sign for 12- to 17-year-olds as a second screening tool. We have also expanded to a second health center for all disciplines. In addition, NEVHC has implemented the PREPARE tool using OTech at three health centers.
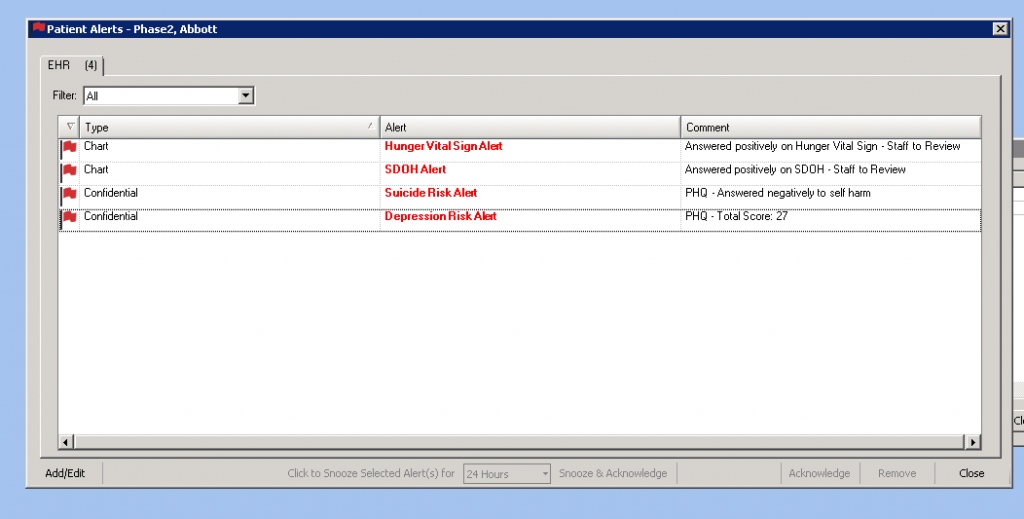
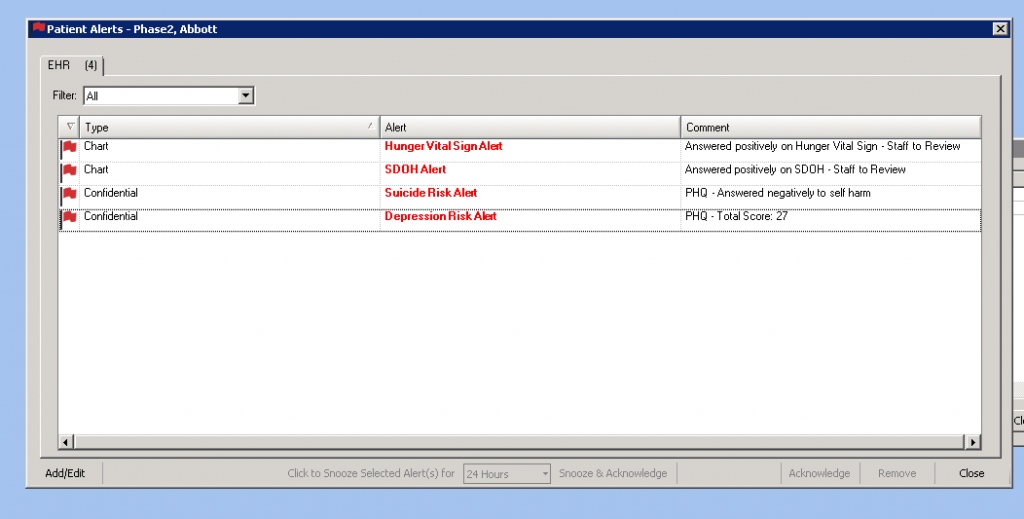
Care team members are now comfortable with the tablets and the majority of patients are using it with ease. The interface continues to work well providing alerts in the electronic health record when the PHQ9 score is 10 or greater, or the patient screens positive to the suicide ideation question, or the patient screens positive to the food insecurity questions or other social determinants of health.
Cycle time for visits has improved significantly due a variety of operational interventions, although not necessarily due to the implementation of Otech. The average cycle time improved from 89 minutes in 2014 to 68 minutes in the first quarter of 2018. Audits also indicate that the accuracy of the data is at 100 percent, and the interface is immediate so the information is available prior to the visit. We have also created alerts in NextGen so positive screens are not missed by the provider.
Lessons & Next Steps
Real-time data extraction, timely action, and expansion to substance abuse, asthma, and tuberculosis screening
Q: What are some of the key insights and learnings from your experience implementing OTech?
A: Our key-takeaways:
- Interfacing the data into the electronic health records is essential. Alerts ensure that providers see and can act on the data during the visit.
- Working Wi-Fi and equipment is critical to the success of the program.
- Interfacing PHQ9 data directly from OTech saved only an average of 39.2 seconds per patient.
- The accuracy of transcription improved significantly and is now at 100 percent.
- Additional screening tools need to be implemented to enable us to see the full value of this intervention.
Q: What is next for your team? Are you planning to expand the solution to other providers and patient populations?
A: NEVHC is now focusing on expanding the number of questionnaires to increase the value of OTech at existing sites. Our future goal is to add most/all of the screening questionnaires to the OTech platform. This is expected to continue to decrease cycle time, improve accuracy by reducing transcription errors, and to store discreet data in the EHR eliminating the need to scan documents and allow for data extraction. We are currently working on the Screening, Brief Intervention, and Referral to Treatment (SBIRT) questionnaires which include our pre-screening questions, the Audit and Drug Abuse Screen Test (DAST 10). OTech is currently working on developing the questionnaires, and we are working with consultants to create the templates in NextGen. Following the SBIRT tools, we expect to add the registration form, Asthma Control Test (ACT) questions, Tuberculosis Risk Assessment, Staying Healthy Assessments and many others.
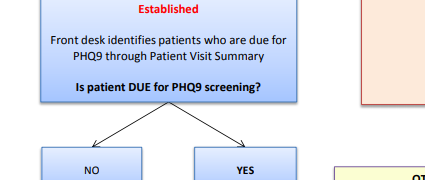
Future goals will be to create an interface from our Clinical Decision Support Tool to identify which survey the patient is due for and only make those tools available to the patient. Currently, the back office staff determine which tools need to be completed and make those available on the tablet.
We are also exploring where these tools should be initiated and expect to test different approaches. Ideally the tablets will be given to the patient at front registration, so the patient can begin the process of completion as early in the waiting time cycle as possible. This again will improve efficiency, accuracy, and improve “value-added” time to the visit. In addition, we would like to add these screening questions to the patient portal, so data could then be collected prior to the patient coming in for their appointment.