Teaming Up to Co-Develop a Referrals App
The team decided to explore a referrals app as a possible solution to their problems. During January and February 2018, staffers met to discuss their options. Over the next few months, as they began looking for a tech solution, luck intervened: Carium, a tech start-up in early development, approached them.
The former COO of the Petaluma Health Center knew the CEO of Carium, so the startup had heard about Petaluma’s work with various startups and with our Technology Hub. Carium had been looking for someone in the safety net to partner with, so the timing was ideal.
In May, after a careful evaluation, Petaluma selected Carium as its partner to develop an app-based solution for specialty referrals. Its executive chairman, Michael Hatfield, 56, was well-known in Sonoma County tech circles for his pioneering research on telecommunications network data. In 2018 he had decided to apply the same skills to the health care system, helping build a tool to collect and analyze the voluminous health data recorded by mobile tools like Fitbit, iPhones and the Apple watch. The health center was a natural fit, he told the Santa Rosa Press Democrat, because the organization was already a leader in using health metrics to better serve its patients.
“We’re very fortunate to have such a high-quality facility like the Petaluma Health Center,” Hatfield told the newspaper. “The thing that I’ve been excited about with this collaboration is we’re doing it all right here in Petaluma, but it’s going to have impact outside of Petaluma.”
Introductory meetings were held in June and the kick-off planned for July 2018. The center planned to work with Carium from August through November on developing and co-designing the referral tools. The Phase 1 launch was planned for November, leaving the team free to evaluate the project in December.

How It Works
For the specialty referral project, Carium developers worked to make the patient app and referral process as seamless as possible.
When the Carium team talked with Petaluma, they learned about two issues with specialty referrals that were eating up a lot of staff time: “Folks who would call on a daily basis to find out about their status; and second, people who never called and in fact needed some nudging to make an appointment,” John McLaughlin of Carium’s customer success division..
With that in mind, he said, the developers created the following set of messages, which the patient sees on the mobile application (app) as the appointment progresses:
1. A message that Petaluma is working on a referral, ending with “Expect an update within 7 business days.”
This way, the referral team sets expectations on timing while the staff clear the appointment with the specialist and the patient’s insurance company.
2. If there is a problem, the patient will be alerted immediately. But if all goes well, the patient will get a new note: Ready to Schedule.
Underneath that, the message would read: “Great news! Your referral with Dr. _____________ is approved. Call the office at 123-555-6789 to schedule your appointment.” The patient can then click on the number and be sent directly to the specialist’s office. “Patients need to schedule the appointment themselves, but we try to make it as easy as possible,” said McLaughlin. The patient then clicks a calendar to input the date and time of the appointment, and the clinic sees the appointment is scheduled.
3. If the patient doesn’t make an appointment, the app will continue to send reminders every three days or so. If there is no response after a week, the patient may get a nudge from the clinic.
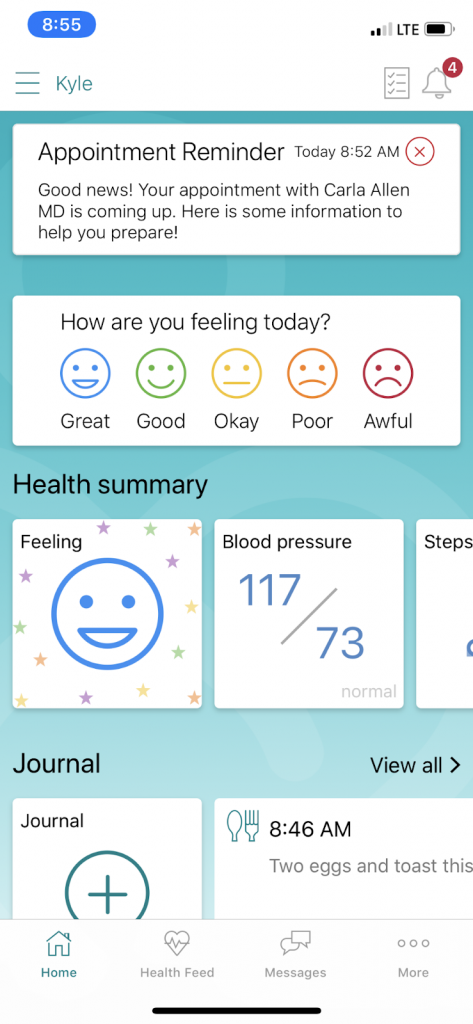
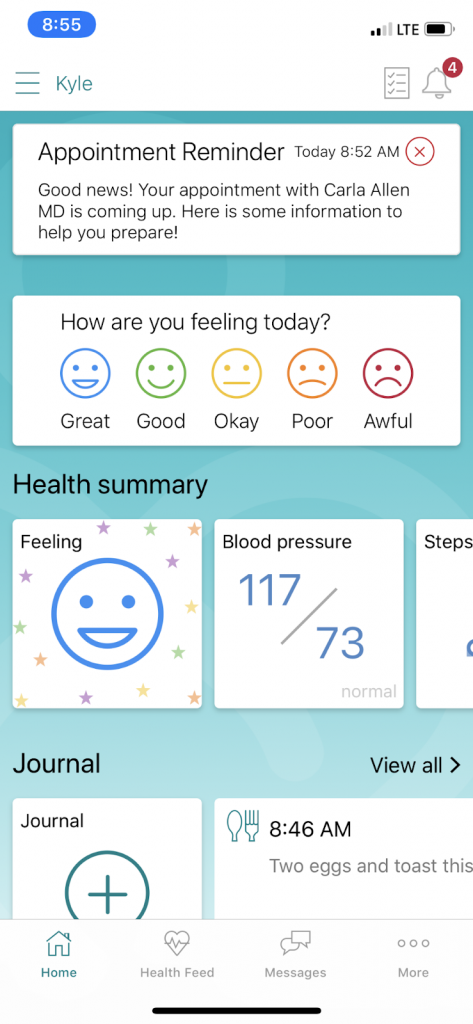
4. As the appointment approaches, the patient is given a reminder about it and some information to make the visit as efficient as possible.
5. On the morning of the appointment, the patients get this reminder: “It’s almost time with your appointment with Dr. X. Tap here for address and phone number.”
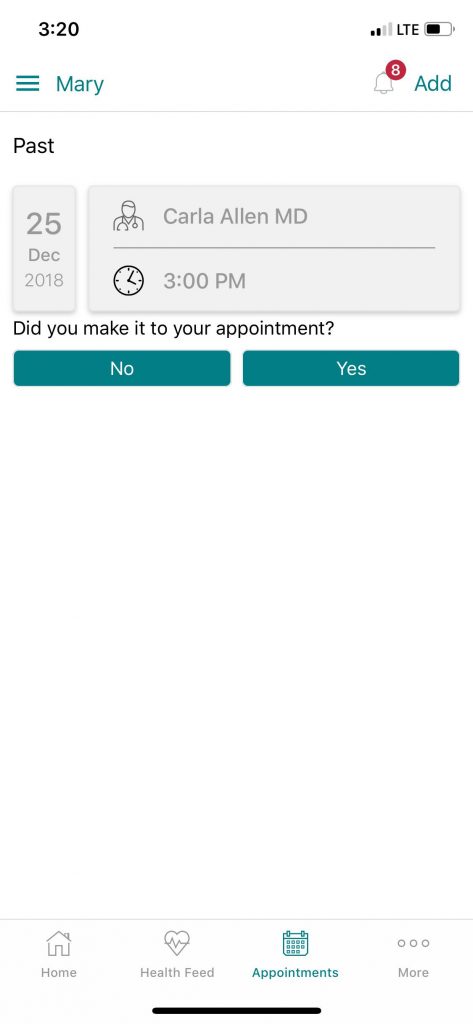
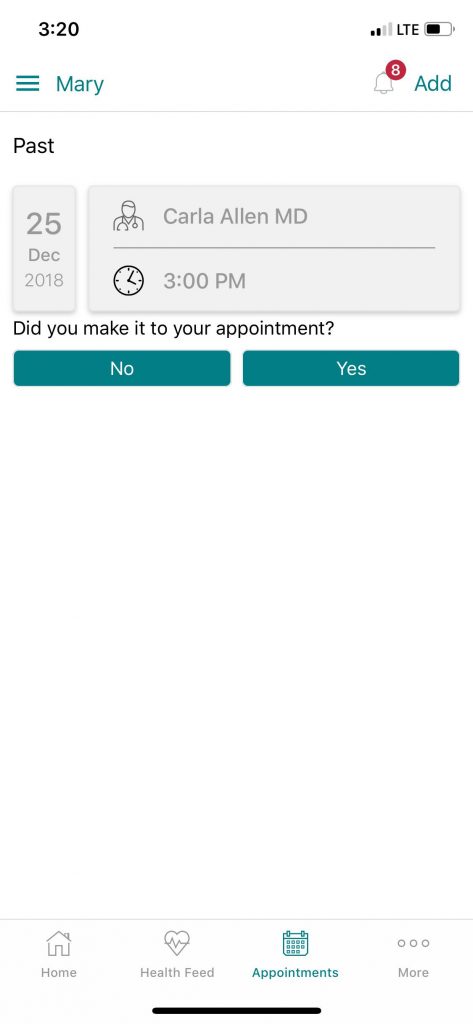
6. After the scheduled appointment has passed, the patient receives a message about the appointment asking simply, “Hi there! It looks like your appointment with Dr. X was today. Were you able to make it to the appointment?” and a “yes” or “no” button to click.
7. If “yes,” the referral process is finished – for the patient. On the provider side of the app, the staff has a list of messages associated with the patient such as “specialist assigned,” “insurance approved,” “appointment scheduled,” and “appointment completed.” But there is still one task left for the office team: “Get provider notes from the appointment.” When this is finished, the referral is complete.
8. At any time in the process, patients can punch the other buttons to record health data such as blood sugar readings, mood, or steps taken each day. They can then share that data with their health care provider or specialist if desired; however, this was not part of the patient referral study.
A New Kind of Working Relationship
Working together closely, the two groups developed a plan in which patients with new referrals would sign up for Carium and receive notifications and status updates through the app. Patients would also be able to key in details about the referral, including the appointment date, or whatever barriers (if any) were preventing them from seeing the specialist.
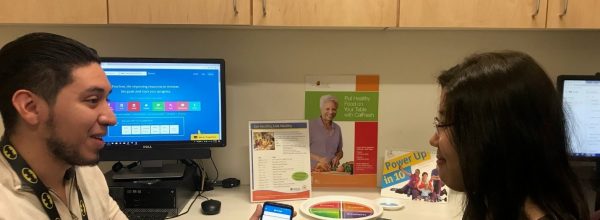
The first Carium employees to visit the health center were those from product development, along with the startup’s medical director. Then Carium proposed a novel working relationship: working side by side with staff at Petaluma to enroll patients in the project. After some discussion, Carium’s product managers and developers joined Petaluma in signing people up. While they were at it, they solicited feedback from both the patients and clinic staff to better guide the next phases of the project.
However, Carium wasn’t just working on a specialty referral tool. Patients could use the same user interface to track their blood sugar, measure how many steps they took each day, keep a health journal and a mood dairy, and manage other health conditions. In fact, Carium used same tool interface in a simultaneous project with Petaluma involving diabetes and self-care.
“We want to be a one-stop shop – a single source where people can track and manage their health and wellness journey,” said McLaughlin. “Of course, for Petaluma, we shadowed the referral team and tailored a solution specific to their work flow. It was a really great experience to get to work with a local place, spending time on site and meeting everybody in the pilot.”
An Indiana native, McLaughlin loves California’s weather, food and natural beauty and feels right at home with Petaluma farming celebrations, such as the town’s annual Butter and Eggs Day Parade. “I pass by the Petaluma Health Center just about every day; it’s such a cornerstone of the community,” says McLaughlin. “I feel lucky to have a chance to work with it.”

Sergio Herrera, Petaluma’s data and electronics health records specialist, found the team approach gratifying. He was impressed by Carium’s commitment and collaborative nature.
“I didn’t know what to expect when I started working with a tech start-up in the health center, but Carium has been open to learning about our work and how they can best meet the needs of our population,” said Herrera. “They have treated our patients with utmost respect and professionalism. Every time I find a glitch in the system they react as quickly as possible to resolve the issue. It’s exciting to think about how this could impact more patients in the future.”
Some Bumps on the Road
Since Carium is still in early development and the team only began its first pilot in November, it has limited data to share. Since the current solution is only available to patients who use iOS, a mobile operating system created and developed by Apple, the pilot has been much smaller than it would have been otherwise. Out of 2,000 referrals, the team was only able to include 20 — or 1 percent — in the study.
In addition, the tech solution is not integrated into the Petaluma’s electronic health record (EHR), requiring the referral data to be entered by hand. For that reason, it required more Petaluma staff time to coordinate and enroll patients than initially expected. “It was a significant investment of our staff time just to get people into the pilot,” reports Jessicca Moore, a nurse practitioner and Petaluma’s associate clinical director.
Results
The Petaluma Health Center launch team’s goal was to learn whether or not an app-based solution could improve patient and staff satisfaction and increase the number of completed referrals.
In the preliminary evaluation, staff reaction to the Carium app was mixed, primarily because there was no EHR integration, requiring the staff to enter data by hand. On the other hand, Moore said, early qualitative data suggested that patients who use the app to track their referrals to specialists are much happier with the process.
“Feedback from patient users was largely positive,” said Moore. They appreciate the notifications, she said, “and they can easily input their appointment information and communicate that back to the Petaluma team via Carium.”
Some patients used the tool for overall health management. “Carium has really helped reduce my stress around managing my health,” said one patient. “I have much more visibility into my specialist appointments, past, present, and future. I’m also using the application to track my blood pressure readings and create a list of my medications, which is really helpful as I prepare for my upcoming surgery.”
| Referral Status |
Quantity |
| Ready to Schedule |
13 |
| Appointment scheduled |
2 |
| Appointment missed |
1 |
| Awaiting appointment notes |
2 |
| Closed |
5 |
| Total |
23 |
Source: Carium
After Phase Two of the project was completed, Carium recapped the tech startup’s main goals and provided metrics:
Goals
- To provide more visibility to the referral team on referral states
- To help patients on their health journey, specifically giving them extra support and info to encourage completion of their referral
Metrics
As seen above, the project assisted 20 patients who together had 23 referrals. Ten patients used the tool actively, with seven making it to the specialist appointment. The other three landed in “appointment missed” or “appointment schedule” status, so the referral team could track their progress.
The other 13 referrals stayed in the “Ready to Schedule” state on the app, even though they received the name and phone number of the specialist. Two patients of the remaining three were confirmed to have seen a specialist.
With nine of the 20 patients confirmed to have scheduled an appointment, the rate of successful specialty referrals was about 50 percent — the same as it was before the pilot project. However, McLaughlin noted, giving more visibility to the referrals while saving on office time fulfilled the first goal: Carium was able to help Petaluma track the referrals automatically “without requiring any intervention from the referrals team.” The team hopes to use the planned patient focus group to figure out how to boost the referral metrics.
Meanwhile, the specialty referral project is partially on hold while the Petaluma re-evaluates the project. “We’re working with Carium to see whether we could get what we want to get out of the tool and whether Carium has the resources to help,” says Moore.
One key goal is that the app be integrated into the EHR, which would substantially reduce the amount of staff time needed to manage it. Carium is working with a third-party developer with expertise in electronic health record integration on this goal.
“Carium thinks they may be able to integrate it with our health record, but we’ve been working with [the EHR] much longer and we know how long and difficult such a process can be,” Moore said. If the partnership continues, Petaluma hopes to (among other things) pull data on referrals directly from the EHR, evaluate a larger patient sample, do focus groups to evaluate user experience, and expand the app to include Spanish.
Lessons Learned
- When working with an early phase start-up, allocate more staff time than you think you’ll need for development and pilot.
- Don’t let lack of EHR integration stall progress. If it’s a worthwhile solution in early phase pilots, you’ll have more leverage to support future integration.