Key Challenges
Logistics and access to updated information at the point-of-care
Q: What was the problem your organization was grappling with?
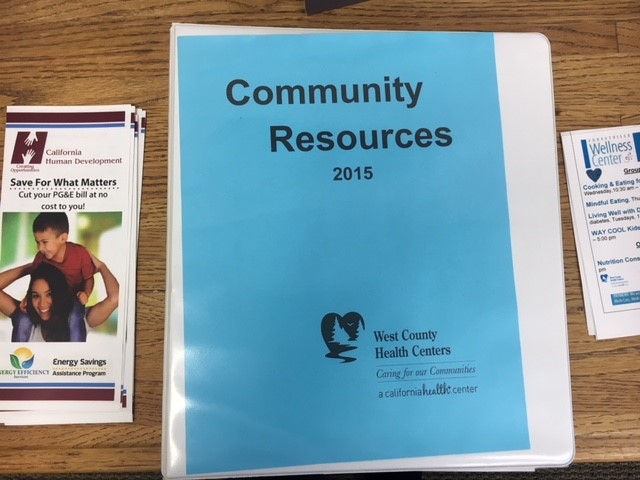
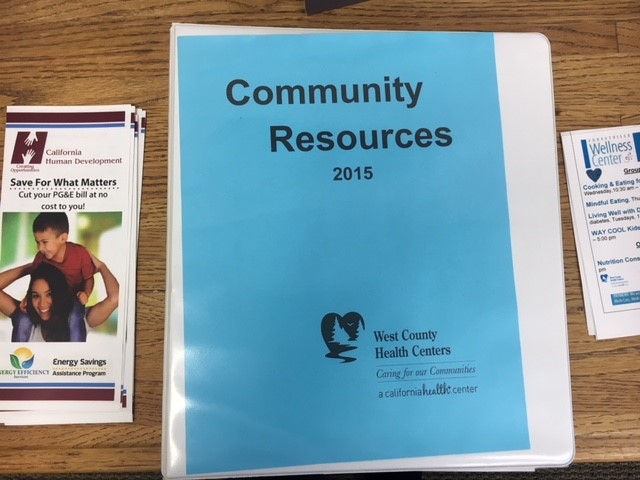
A: WCHC recognizes that every patient of ours is unique and deserves the best service to meet their unique needs – beyond just health care – so we developed a paper-based “Community Resource Binder” that housed social service resources throughout the county. These binders lived in all our exam rooms and on the desks of many staff members. Keeping the resource information within the binders up-to-date and stocking the many three-ring binders was not easy and limited the usefulness to staff and patients. In addition to the logistics of keeping these resources updated, WCHC rarely knew if patients went to the social service that were recommended.
Q: How did you learn it was a problem, and why was it important to address?
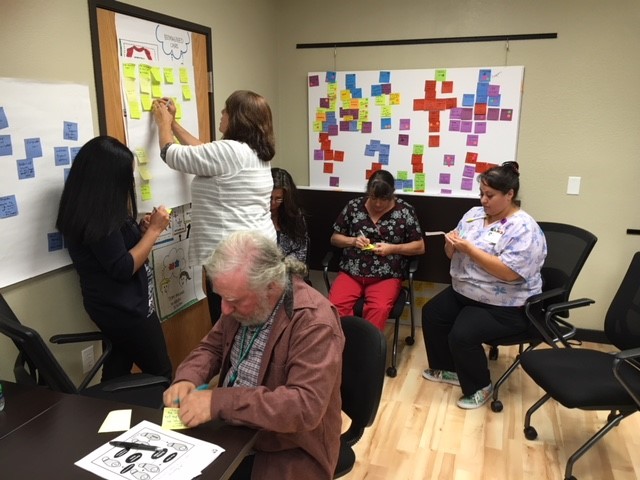
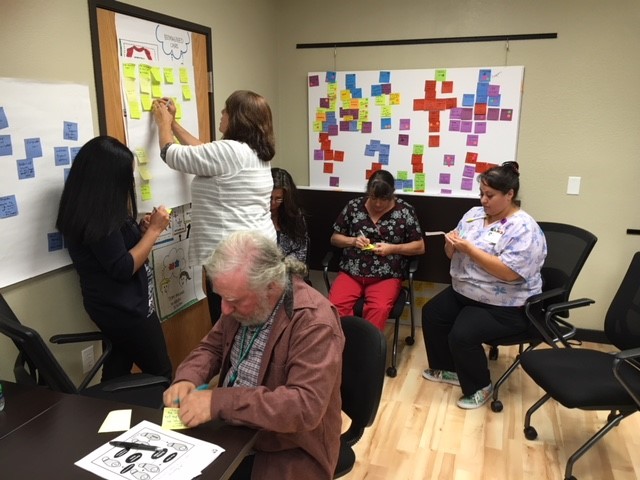
A: To better understand the problem, WCHC used human-centered design methods and techniques to research the many different aspects and dimensions of the challenge. Observational research allowed us to see things differently and it gave us great insights into what our staff and patients were experiencing daily. Importantly, this process allowed us to engaged the end-users and create internal buy-in early on. We were able to validate our hypothesis – staff across the agency had trouble locating the resource binders, countless services were out of date and staff were not able to know if their patients got connected with the resource they gave them.
Testing
Transitioning from paper binder to Purple Binder
Q: Describe the solution you tested. How did you come to decide to try this solution?
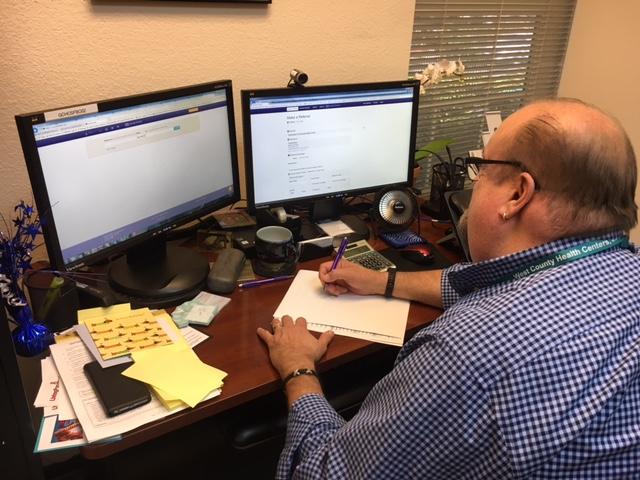
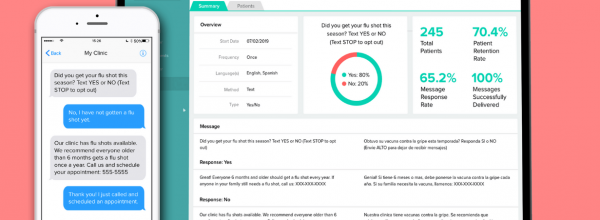
A: We decided to pilot Purple Binder because it is web-based platform that has accurate, hyper-local social service information that is easy to connect our patients. In addition, Purple Binder offers information such as: eligibility requirements, intake process, applications, and wait list – this feature makes it easy for our staff at a glance to know if this resource would be a good fit for our patient. Lastly, Purple Binder offers real-time support via live chat help finding just the right resource for our patient.
Q: What structure did you put in place for the pilot (e.g. how many end users, for what use cases)? What eligibility criteria did you choose for the pilot, and why?
A: WCHC focused the pilot on the two separate functions within Purple Binder, the “digital resource directory” and “referral gateway”. We started piloting the resource directory with approximately 30 staff end users in September of 2016. Because this digital resource was such an asset to our organization and because many other clinical support staff used our outdated community resource binder everyday it just made sense for us to expand our piloting users to 60 end users in December of 2016. Our evaluator created a 3-D network map of soft referral data between September 2016 and March 2017 among our health care partners in the Sonoma County Collaborative also demoing Purple Binder. In regards to the referral gateway we chose to keep this piloting group small – with that said, we have 4 Access Coordinators, 1 Transition Case Manager and 2 Staff Members at a referring social service organization (Food For Thought) participating in this pilot.
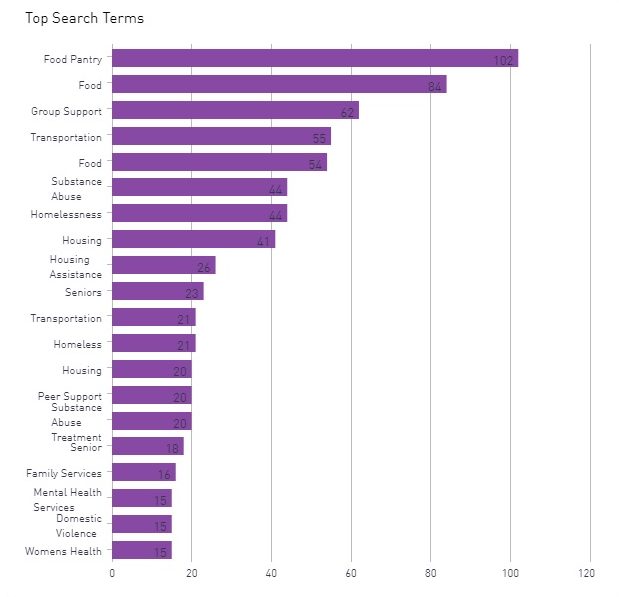
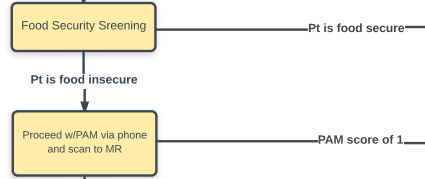
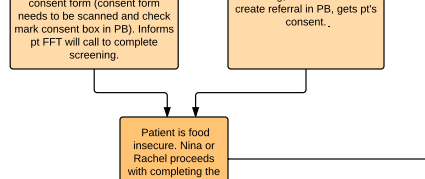
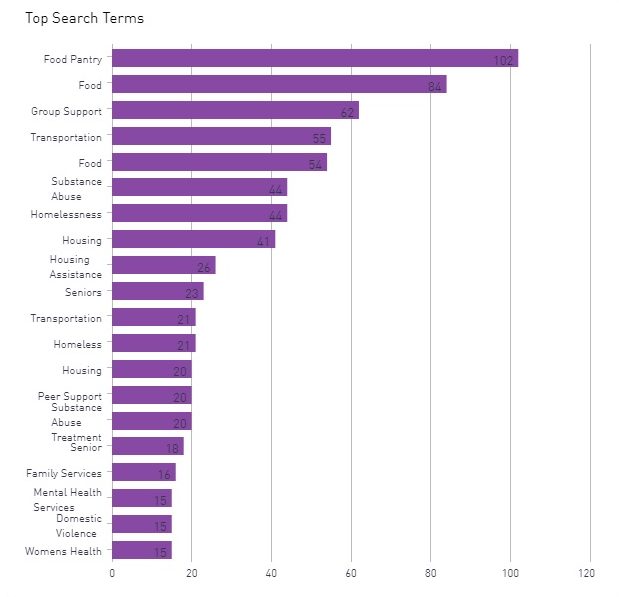
WCHC has made a commitment to address the social determinants of health (SDOH) in our community by collecting SDOH data on all our patients – food insecurity is one of the most pressing issues our patients face (see top search terms below), so WCHC decided to tackle this area of opportunity with a partnering social service organization called Food For Thought. We were interested in looking at the impact of successful referrals to address patient’s food insecurity. This pilot was split into two cohorts for evaluation: (1) high system utilization patients with risk of heart disease or stroke and (2) Hospital Transition Care. In both cohorts, patients were screened for food insecurity as well as patient activation (PAM), depression (PHQ9), broad social determinants of health barrier, (PREPARE SDOH tool) in addition to trending claims hospital and ER utilization at baseline and at 6 and 12 months post initiation of the Food For Thought portion of the pilot.
Lessons & Next Steps
Collaboration, funding, and new features
Q: What are some of the key insights and learnings from your experience testing Purple Binder?
A: Connecting patients to appropriate community based resources is a regional solution and required us to think differently about how we approached piloting and test a solution. Our most interesting challenge was participating in a pilot that required regional partnerships both in the implementation of the solution and also in the contracting and vendor management. The most difficult part was developing a network of organizations to participate in the testing phase. It took a long time to develop that network and reach an agreement on terms of the contract and participation expectations.
In one sense, the work that was required to move this project forward took much more effort to gain consensus, and the testing cycle was more complex and slower than we are used to managing. Contracting and vendor negotiation was more complicated and took considerable effort early in the pilot.
Funding remains the most important factor for sustainability. Collaboration across a county collaborative and exposing other potential partners to this solution has been essential in the pilot phases. Due to the groundwork of engaging the Redwood Community Health Coalition and consensus building early on, we were able to garner broad interest and support in the community. We have strong interest from several county-wide initiatives who are interested in participation and to assist with sustainable funding.
Q: What is next for your team? Are you planning to expand the solution to other providers, staff, and patient populations?
A: While we have fully implemented Purple Binder across the organization, we are still assessing and understanding the value of using a digitized resource and navigation platform for specific use cases. For example, we are currently uploading resources to support patients who have been affected by the North Bay wildfires.
In addition, we are still in the process of vetting the referral gateway with the SDOH intake specific form mentioned previously. Once we reach our goal of 40 patients receiving food for at least 6 months in the Food For Thought pilot, we will have more information about its value to the patient and potential impact on health system utilization. However, in the meantime we would like to partner with more social service agencies to test the minimal “make a referral” process. We have demoing this at the county and social service level and are still waiting to hear back if other social service agencies would like to join. We are also reviewing other solutions in the space to identify a roadmap of new features for Purple Binder to work on for us as they transition to Healthify.