![]() Central to effective and equitable implementation of telemedicine care is engaging a diverse patient population.
Central to effective and equitable implementation of telemedicine care is engaging a diverse patient population.
Some of the most pressing areas of consideration to ensure telemedicine does not worsen existing health disparities include:
- Understanding patients’ digital access and skills,
- Connecting patients with technical support,
- Integrating interpreters into remote/virtual visits for those with limited English proficiency, and
- Engaging patients’ caregivers and additional support services and teams.
Finally, it is critical that the interpersonal components of care, built upon a foundation of trust between patients and providers, are at the forefront of all patients’ virtual care experiences.
→ Want a more searchable and tagged version of this toolkit? Check out the Virtual Care Learning Hub!
Screening Patients’ Digital Access and Skills
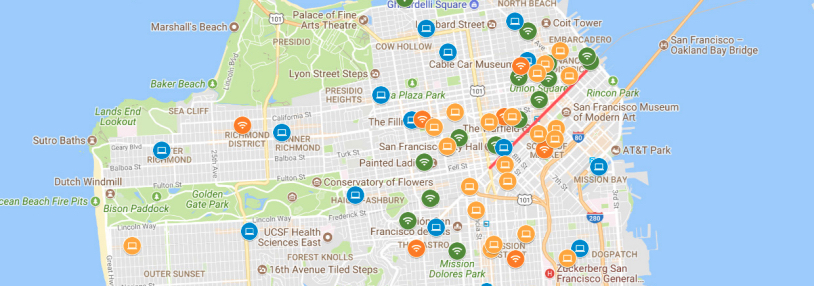
While smartphone ownership in the US continues to climb, the digital divide in the US persists for many. Groups with the lowest rates of home Internet use and smartphone ownership include low-income Americans, older adults, and those living in rural areas. In addition, more than a quarter of low-income individuals use their smartphone as their only online access point, without home internet, presenting challenges for sufficient data/bandwidth to connect to video visits. Finally, barriers related to digital literacy — the skills to be able to use email, apps, and other online tools — are common for many patients even if they have access to a device. Health care systems can screen patients’ digital access and skills, allowing for improved alignment between workflows and patient needs. Screening could also include patient preferences for communication (in-person, phone, text, email, etc.), to ensure support for digital modalities while simultaneously supporting patient preferences for their care.
- San Francisco Health Network: Zoom Video Visit Patient Sign-Up and Onboarding Script — This resource provides a script for contacting and signing up patients for Zoom video visits, including questions about patients’ preferred modality (“Would you be interested in doing a video visit instead of a telephone visit for your appointment?”) as well as device capabilities (“Do you have a device with a camera?”), internet access (“Do you have wifi or an unlimited data plan?”), and digital skills (“Do you need help setting up for zoom?”). It also includes a script for onboarding video visit patients to Zoom once they have a video visit set up, including language specific to different types of patient devices. This tool was created by the San Francisco Health Network — a public network of clinics, hospitals, and programs within the Department of Public Health in San Francisco, California that connects San Franciscans to quality health care regardless of immigration status or lack of insurance — as part of their work through CCI’s Connected Care Accelerator.
- Los Angeles County Department of Health Services: Video Visit Screening & Script — This script is used to inform and screen patients for Zoom video visits. It includes a brief overview of why patients might be interested in signing up for a video visit (e.g. “There is no travel time or transportation cost.” “You’ll be able to show your provider anything you would like to instead of trying to describe it over the phone.”) as well as screening questions to assess Internet and device access. It makes clear that the screening questions to assess patients’ readiness for video visits are asked of every patient and provides sample responses to use when patients are, or are not, ready for a video visit. This tool was created by the Los Angeles County Department of Health Services – an integrated public health system that provides health services to residents of Los Angeles County, California and is the second-largest municipal health system in the nation – as part of their work through CCI’s Connected Care Accelerator.
- San Francisco Digital Equity Initiative: SF Digital Equity Playbook — This PDF includes concrete guidance on assessing digital access and skills. This playbook includes sample intake forms which could be used to screen patients’ digital needs on page 16.
- UCSF Center for Vulnerable Populations: Sample Questions to Screen Patient Digital Needs — This PDF includes questions health care systems can adapt and use to assess patients’ digital needs, including internet use, device access, broadband and data plan access, and confidence using technology.
Technical Support for Patients, Especially Those with Limited Digital Literacy
Broadband and Device Access. There are multiple avenues to support patients’ ability to access and use telemedicine services such as video visits. Multiple existing programs exist to help patients sign up for low-cost devices, data plans, and broadband.
- National Digital Inclusion Alliance: COVID-19 Resources — This webpage has a list of COVID-19 resources, including low-cost broadband programs.
- Federal Communications Commission (FCC): Lifeline Program for Low-Income Consumers — This webpage has an overview of the FCC’s Lifeline Program, which supports smartphone ownership for low-income Americans.
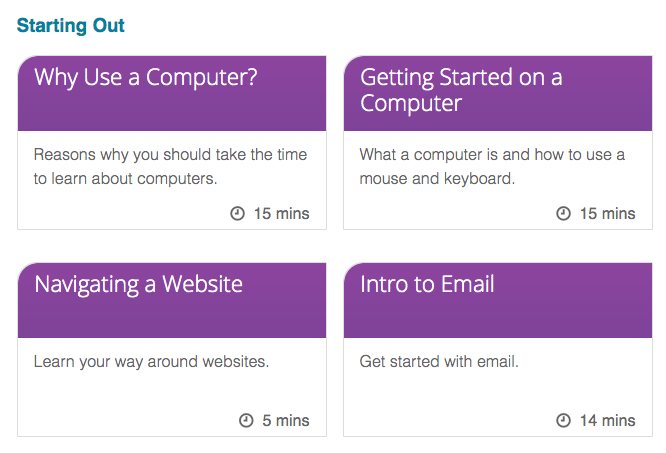
Digital Skills Training. In addition, many groups can provide support for patients who need basic training to use a smartphone or computer, such as learning to download apps or conduct online searches. While resources vary within regions and cities, the public library system is often an important place to start for basic skills training, both nationally as well as through your local public library branches to determine offerings.
- Public Library Association: Digital Learn Program — This webpage has a collection of online tutorials covering computer and internet basics.
- TeleHealth Access for Seniors — This webpage has multiple guides for digital literacy basics, including translation of guides into multiple languages.
Technical Support for Patients. Finally, health care systems themselves can bolster the technical support they provide for patients. Specific questions about the platforms used within your setting are likely best handled by your organization, such as how to use the patient portal to get into a video visit or how-tos on using a specific video vendor platform.
- Alameda Health System: Digital Health Outreach Playbook — This playbook contains a wealth of resources for supporting patients in accessing digital health tools, including the patient portal, that are often necessary for telemedicine. Starting on page 10 it includes a phone script for screening patients’ digital access and helping them enroll in the MyChart patient portal, and starting on page 12 it includes a pictorial-based tip sheet to help patients download a patient portal app. The additional resources starting on page 27 also include email templates and instructions to help patients sign up for and download MyChart in both English and Spanish. This playbook was created by the Alameda Health System — an integrated public health care system of 5 hospitals and 4 wellness centers promoting wellness, eliminating disparities, and optimizing the health of diverse communities in Alameda County, California regardless of social and financial barriers — as part of their work through CCI’s Connected Care Accelerator.
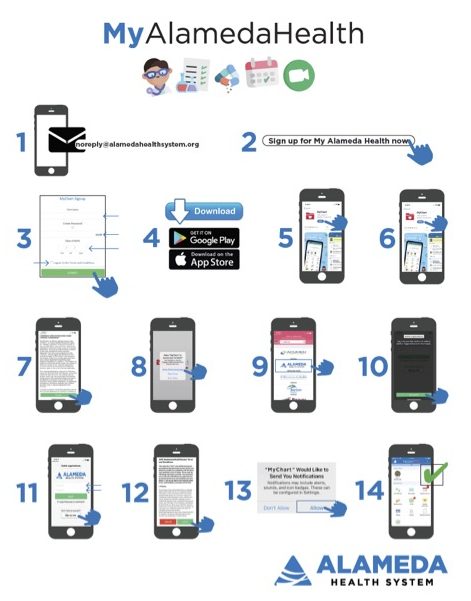
Alameda Health System
- UCSF Center for Vulnerable Populations: Resources for Telehealth at Safety Net Settings — The “For Patients” section of this webpage includes a PDF with Zoom visit instructions, as well as brief video tutorials for patients to download this app in English, Cantonese, Mandarin, Russian, Spanish, and Vietnamese on both Android phones and iPhones. Also, the section on “Considerations for using Remote Visits within Safety Net Healthcare Settings” has workflow considerations for providing care by telemedicine to patients with limited digital literacy.
- Journal of the American Medical Informatics Association: Portal Implementation Activities at Five Community Health Centers in California — This table, from a rapid ethnography of patient portal implementation at safety-net health centers in California shows a range of community health center activities to promote portal use among diverse patients.
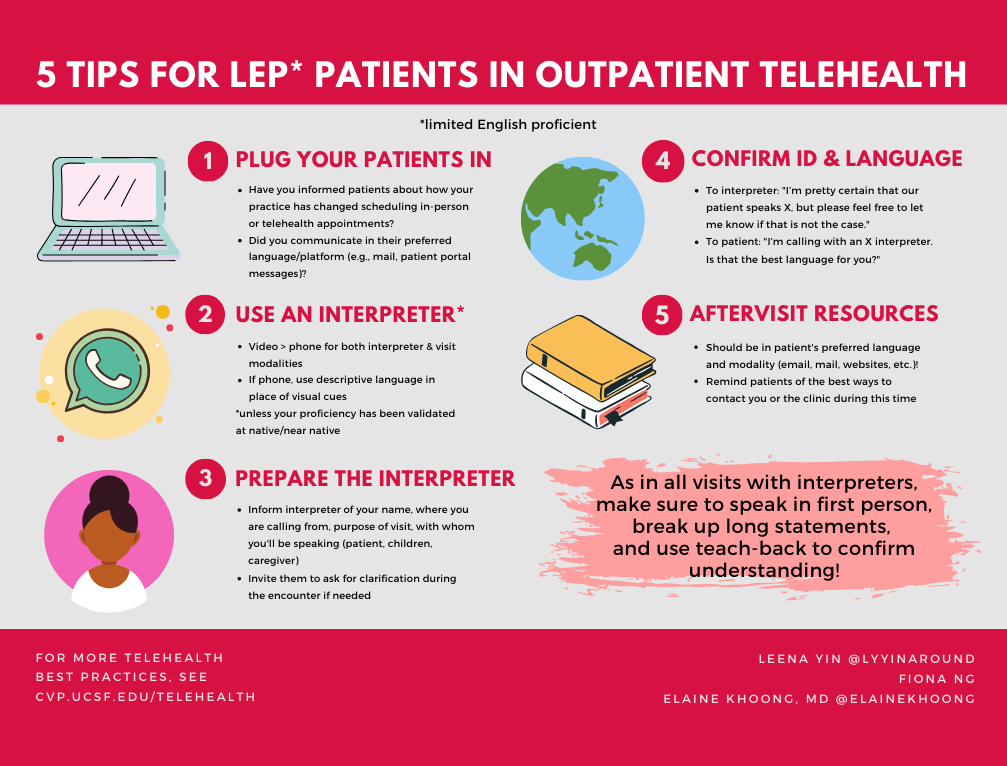
Use of Interpreters and Non-English Instructions/Prompts in Technology
Patients with limited English proficiency may experience additional communication barriers to engaging with telemedicine. Not only do all how-to and FAQ materials about platforms and systems need to be provided in multiple languages, but the use of interpreters on phone and video visits also needs specific attention. In addition, the use of three-way calling and video medical interpretation is an extremely high priority for safety net health care systems to successfully launch their telehealth programs.
- 10 Tips for Caring for Immigrant and Limited English Proficiency Patients in the Age of COVID-19: This PDF, created by UCSF and other health care providers and researchers, outlines best practices for interpreter use when caring for immigrant and limited English proficiency patients via telemedicine during the pandemic.
- Health Information Technology, Evaluation, and Quality (HITEQ) Center: Telehealth Strategies and Resources for Serving Patients with Limited English Proficiency — This is a link to download a PDF providing near-term and longer term strategies to support limited English proficiency patients with telehealth, including the utilization of third-party services for real time interpretation and how to add interpreters on telehealth platforms.
- Mid-Atlantic Telehealth Resource Center: Telehealth Resources for COVID-19 Toolkit — The “Best Practices for Conducting a Telehealth Visit” section of this webpage has a subsection on “Meeting the Needs of Patients/Clients Who Need Interpreters” with additional considerations and links to other resources on how to approach this issue.
- TDI: Coronavirus (COVID-19) Resources — This website has specific information about telehealth access for deaf and hard-of-hearing populations.
Engaging Caregivers
There are additional considerations for telemedicine that will likely require new resources and knowledge. This includes the best ways to engage caregivers (such as family and friends, as well as case management or in-home support services) who may be integral for telemedicine uptake for certain patients. If patients want to involve others in assisting them with either the technical or the medical components of telemedicine visits, then more proactive caregiver engagement may be needed to expand telemedicine access.
- AARP: Using Telehealth to Improve Home-Based Care for Older Adults and Family Caregivers — This PDF white paper outlines the critical issues involved in supporting caregivers of older adults in telemedicine implementation.
Upholding Patient Trust
Building Trust During the Encounter. Considerations for patient trust must be woven into all efforts to support telemedicine. Previous research has clearly documented patients’ desires to maintain in-person relationships with providers and continued patient concerns about privacy and security related to telemedicine. Developing communication around how telemedicine will be used in conjunction with in-person care and as a way to increase support and connection for patients — as opposed to substitute or replace routine care — will be critical to any program. This is particularly important when caring for patient populations who experience justified mistrust of medical institutions and fears of surveillance because of historical and present abuses.
- Advisory Board: Tips to Improve Your “Webside Manner” — This website has an infographic on how to ensure telemedicine care remains patient-centered. Tips include ensuring a clear, well-lit screen view and presenting in the professional attire that works best for you. A visual ID badge may be reassuring especially for a new patient visit. Just as in in-person visits, refrain from eating or multitasking and maintain eye contact.
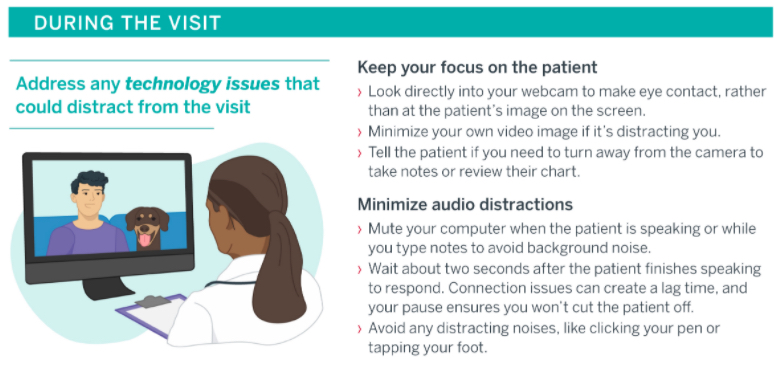
Advisory Board
- Center for Care Innovations: Empathetic Communication in Phone and Video Visits — This webinar by an expert motivational interviewing trainer reviews best practices in empathy-based communication for virtual health care settings. Links to additional PDF resources with tips for empathetic communication when providing care by phone and video can be found online here.
- Cleveland Clinic: COVID-19 Response Digital Health Playbook — This PDF provides guidance from the Cleveland Clinic on the expansion of telemedicine and digital health platforms. It includes a section on “Empathy in Virtual Visits” on pages 43-47 with helpful tips on establishing patient relationships, expressing empathy, and conveying value and respect during virtual visits.
- UCLA Pediatric Psychology Consultation Liaison Service: COVID-19 Tips—Building Rapport with Youth and Adults via Telehealth – These two PDF resources provide tips on setting the scene, introducing telehealth to patients, building rapport, and keeping adult and youth patients engaged in telemedicine visits. While some information is specific to mental health, most is broadly applicable to telemedicine care. The PDF focused on adults also includes a section focused on group telemedicine sessions.
Communicating Changing Models of Care. Special attention should be paid to communications regarding changes to protocols and models of care due to the COVID-19 pandemic. Clarity regarding office open hours, in-person availability, safety protocols, and new telemedicine offerings will be crucial to maintaining patient trust.
- North East Medical Services: Video Visit Flyer and Instructional Videos —These flyers were designed to promote the availability of video visits in English, Chinese, and Vietnamese. The flyer also includes instructions on how to download and use Zoom for the video visit. In addition, these short instructional videos in English, Cantonese, and Mandarin help patients navigate using Zoom. These tools were created by North East Medical Services (NEMS) — a community health center serving the medically-underserved populations of the San Francisco Bay Area, California and one of the largest community health centers serving Asians in the United States — as part of their work through CCI’s Connected Care Accelerator.
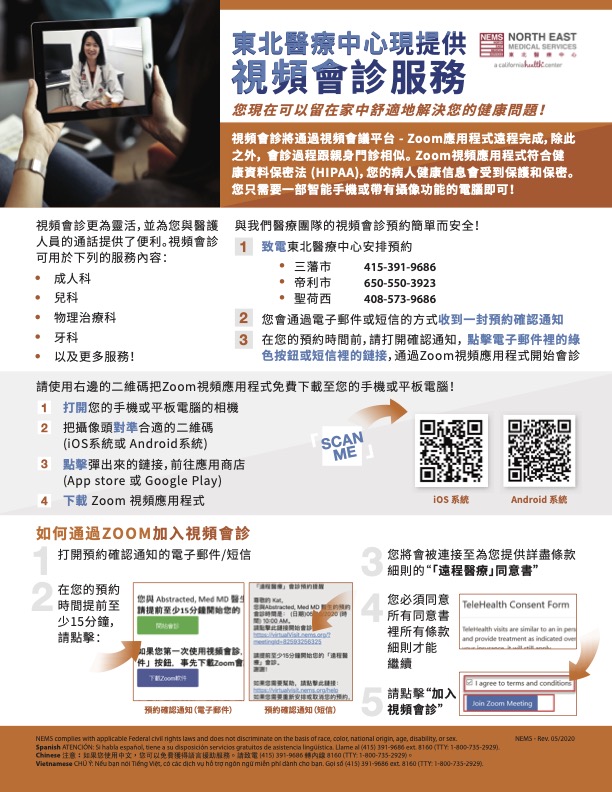
North East Medical Services
-
- Neighborhood Healthcare: Demonstrating a Video Visit Workflow — This video walks through the entire video visit process using eClinicalWorks and Doxy.me, from when a patient calls for an appointment to the visit itself to the post-visit follow-up. The goal is to help demystify the telemedicine process for patients who may be unsure about what a video visit entails. This tool was created by Neighborhood Healthcare — a Federally Qualified Health Center with sites throughout San Diego and Riverside counties in California that provide medical, dental, and behavioral health services to every member of their community, regardless of situation or circumstance — as part of their work through CCI’s Connected Care Accelerator.
- Northeast Valley Health Corporation: Patient Video Visit Tutorial (Spanish) — This video provides a Spanish-language overview of the video visit process using Otto Health. It outlines what a video visit is, what the visit confirmation texts and emails will look like, tips for logging on with a compatible web browser and checking connection quality, displaying the video visit portal instructions in Spanish, giving access to the device’s camera and microphone, the virtual check-in and waiting room processes, how to use the chat function, and how to add an additional person to the visit. This tool was created by Northeast Valley Health Corporation — a Federally Qualified Health Center with 14 sites in the San Fernando and Santa Clarita valleys in Los Angeles County, California providing medical, dental, and behavioral healthcare for uninsured and medically underserved patients with limited financial resources — as part of their work through CCI’s Connected Care Accelerator.
- California Medical Association (CMA): Reopening a Medical Practice: Communicating with Your Patients and Others — This PDF is about communicating with patients and others about re-opening a medical practice during the COVID-19 pandemic. This guide has recommendations and templates to help health systems communicate with patients and other health care organizations about changes via email, social media, and signage. These templates can be modified to suit the needs of your practice.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.