![]() The COVID-19 pandemic prompted health care providers and systems to rapidly adopt and expand telemedicine services. Telemedicine provides a safer alternative to in-person visits during the pandemic, but simultaneously introduces multiple decision points for implementation.
The COVID-19 pandemic prompted health care providers and systems to rapidly adopt and expand telemedicine services. Telemedicine provides a safer alternative to in-person visits during the pandemic, but simultaneously introduces multiple decision points for implementation.
While many providers already have telemedicine in place, emerging evidence, policies, and guidance on implementation and maintenance indicate that answers to the question, “how do we implement telehealth equitably, safely, and sustainably?” are very much still evolving. In this chapter, we summarize many of the basic components of telemedicine implementation for health care system leaders, including:
- Evidence for implementing telemedicine,
- Risks, privacy and security,
- Reimbursement,
- Vendor selection, and
- Performance measurement.
These topics are particularly important in safety-net settings that already face challenges related to limited resources and fragmented health information technology.
→ Want a more searchable and tagged version of this toolkit? Check out the Virtual Care Learning Hub!
Evidence for Efficacy and Quality
Quality and Effectiveness. Evidence is growing on telemedicine use among diverse and low-income patient populations, including individual and population-level factors associated with telemedicine uptake and satisfaction.
- Health Affairs: The Current State Of Telehealth Evidence: A Rapid Review — This review article has recent evidence regarding telehealth’s efficacy in various clinical areas, as well as its impact on health care utilization.
- Diabetes Research and Clinical Practice: Does Telemedicine Improve Treatment Outcomes for Diabetes? A Meta-Analysis of Results from 55 Randomized Controlled Trials — This review article has evidence regarding telemedicine’s effectiveness for diabetes management compared to conventional care. The authors find that telemedicine is more effective in improving diabetes outcomes than conventional care, particularly for type 2 diabetes.
- International Journal of Medical Informatics: Effectiveness of Telemedicine: A Systematic Review of Reviews — This review article has evidence regarding the impacts and costs of telemedicine, including for behavioral conditions. The authors note a continued need for larger, controlled studies of telemedicine interventions, as well as further study of telemedicine’s cost-effectiveness and impact on patient satisfaction.
- Agency for Healthcare Research and Quality: Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews — This evidence map contains 58 systematic reviews on telehealth, which concluded that there is sufficient evidence to support the use and effectiveness of telehealth for specific uses with some types of patients, including: remote patient monitoring for patients with chronic conditions, communications and counseling for patients with chronic conditions, and psychotherapy as part of behavioral health. Further, they find there is emerging evidence to support the use of telehealth for maternal and child health, as well as triage and urgent care. The PDF version is available online here.
Patient Satisfaction. Telemedicine has also been found to have high patient satisfaction, on par with in-office visits, due to ease of use and improved communication.
- BMJ Open: Telehealth and Patient Satisfaction: A Systematic Review and Narrative Analysis — This review article has evidence on patient satisfaction regarding telehealth effectiveness and efficiency.
- American Journal of Managed Care: Patient and Clinician Experiences with Telehealth for Patient Follow-Up Care — This cross-sectional study about patient and clinician perceptions of virtual video visits compared to office visits found that the majority of patients and clinicians reported no difference in overall quality between visit types.
Telemedicine to Address Health Equity. Evidence is growing on telemedicine use among diverse and low-income patient populations, including individual and population-level factors associated with telemedicine uptake and satisfaction
- American Journal of Preventive Medicine: Who Is (And Is Not) Receiving Telemedicine Care During the COVID-19 Pandemic — This research brief examines changes in telehealth use during the COVID-19 pandemic among over 6 million employer-based health plan beneficiaries. The authors found the increase in telemedicine use during the pandemic was greatest among patients in counties with low poverty levels, patients in metropolitan areas, and among adults (as opposed to children). They note the importance of prioritizing outreach to patients whose in-person care is not currently being replaced with telemedicine visits.
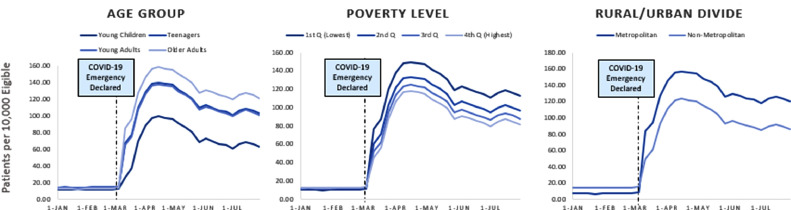
Adjusted rates of telemedicine utilization before versus that after the start of the COVID-19 pandemic. Cantor et al. 2021
- Journal of the American Medical Association: Telehealth Use Among Safety-Net Organizations in California During the COVID-19 Pandemic — This short research letter describes the trends in the use of in-person, phone, and video visits among FQHCs in California before and during the COVID-19 pandemic. The FQHCs included in the analysis were participating in CCI’s Connected Care Accelerator program. They found that visit volume overall declined only modestly for primary care because telemedicine visits, especially phone visits, replaced in-person visits. The authors noted the importance of phone visits in meeting the needs of low-income patients.
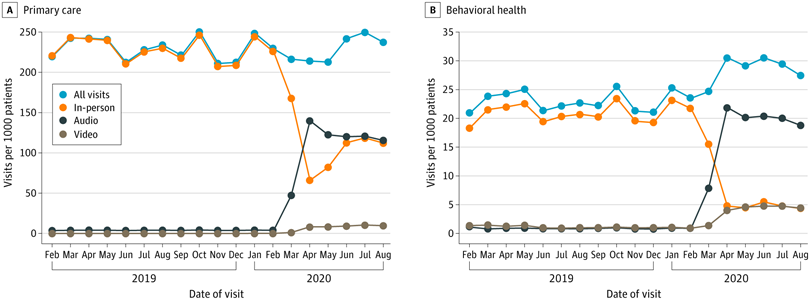
Primary Care and Behavioral Health Visits per 1000 Patients by Visit Type from February 2019 through August 2020. Uscher-Pines et al. 2021.
- American Journal of Managed Care: Differences in the Use of Telephone and Video Telemedicine Visits During the COVID-19 Pandemic — This cross-sectional examined patient and neighborhood characteristics associated with visit modality (in-person, video, or telephone). They found that patients who were older than 65 years old, Black, Hispanic, Spanish-speaking, and from areas with low broadband access were less likely to use video visits. In addition, they found that practices and clinicians drove more of the variation in video visit use than patients.
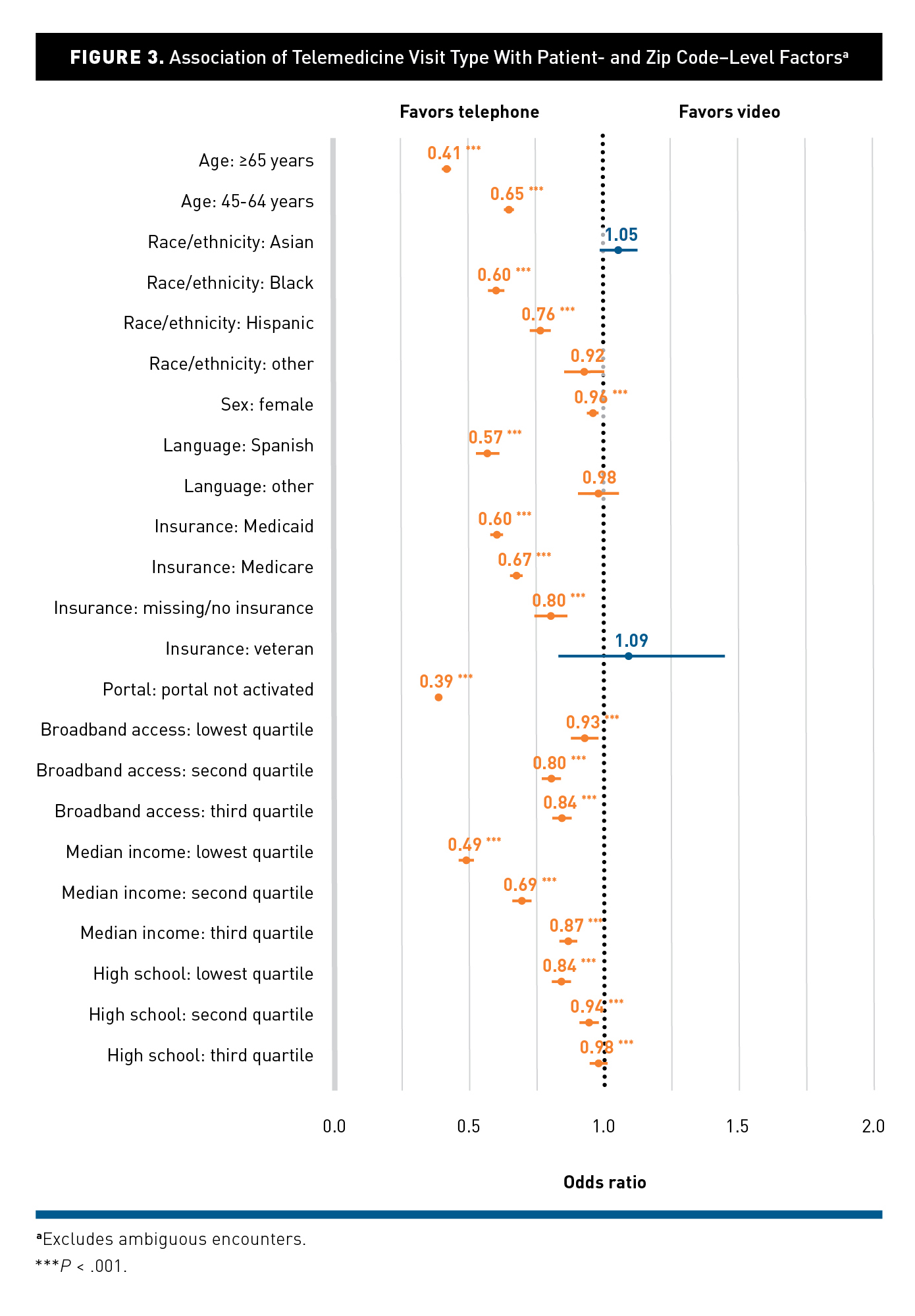
Association of Telemedicine Visit Type with Patient- and Zip Code-Level Factors. Rodriguez et al. 2021.
- Health Affairs: Disparities in Telehealth Use Among California Patients with Limited English Proficiency — This study examines the association between patients’ limited English proficiency (LEP) and telemedicine use (phone and video visits). They also evaluated the impact of telemedicine on healthcare access and use. The authors found that LEP patients had lower rates of telemedicine use compared to proficient English speakers, and that telemedicine use was associated with increased emergency department use for all patients.
- JAMA Network Open: Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians — This article outlines patient characteristics associated with choosing between telemedicine and in-person visits within Kaiser Permanente Northern California. For example, the authors found that choosing telemedicine was associated with in-person visit barriers such as clinic parking costs. They also found that Black patients were more likely to choose telemedicine than other racial/ethnic groups, and patients living in lower socioeconomic status (SES) neighborhoods were more likely to choose telephone visits, but they were less likely to choose video visits than patients in higher SES neighborhoods.
Privacy and Security
Regulations. The U.S. Department of Health and Human Services eased enforcement of telehealth regulations in March 2020 as a result of the COVID-19 pandemic. This discretion allows providers to use any nonpublic audio or video communication tool to connect with their patients remotely. More details about these changes in telehealth regulations can be found in the resources provided below.
- U.S. Department of Health and Human Services Office for Civil Rights: FAQs on Telehealth and HIPAA during the COVID-19 Nationwide Public Health Emergency — This PDF has answers to frequently asked questions about the enforcement discretion regarding telehealth during the COVID-19 pandemic, such as which parts of HIPAA are included, and what telehealth services are covered.
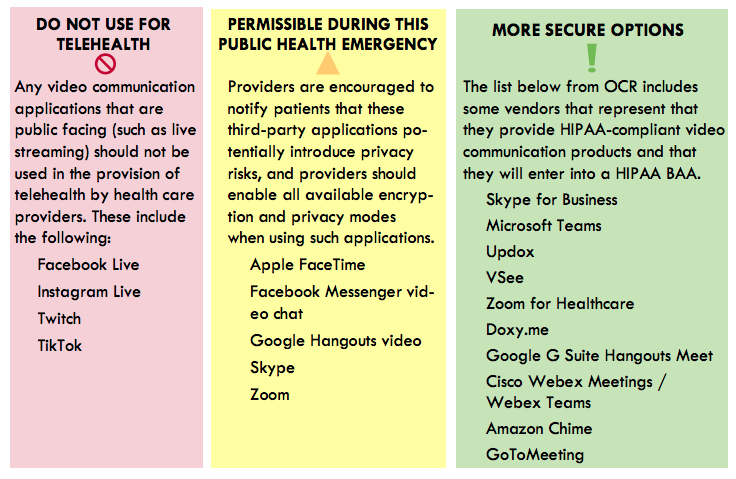
- Health Information Evaluation and Quality (HITEQ) Center: Using Non-Traditional Technology for Telehealth during COVID-19 Pandemic — This is a link to download a PDF tip sheet with important considerations for using non-traditional technologies for telehealth. It includes a color-coded guide of which technology platforms are most secure for telemedicine, which are permissible during the public health emergency, and which are not suitable for telehealth.
Cybersecurity. In implementing telemedicine, cybersecurity is a critical consideration for health systems. Main recommendations for improving cybersecurity include using encrypted devices and technology, utilizing a Virtual Private Network (VPN), and employing strong authentication parameters.
- U.S. Department of Health & Human Services and the Healthcare & Public Health Sector Coordinating Councils: Health Industry Cybersecurity Practices: Managing Threats and Protecting Patients — This PDF report provides guidance and solutions for mitigating cyberthreats facing the health care industry. Main scenarios include email phishing attacks, ransomware attacks, loss or theft of equipment or data, insider data loss, and attacks against connected medical devices that may affect patient safety.
-
- Technical Volume 1 (PDF; for small health care organizations) and Technical Volume 2 (PDF; for medium and large health care organizations) provide practical steps to implement these cybersecurity practices.
-
- UCSF Center for Vulnerable Populations: Resources for Telehealth at Safety Net Settings — This webpage provides resources for telehealth in safety net settings. The section “For Clinicians” includes a link to download a word document “Setting up your Zoom account for patient video visits” with concrete guidance on ensuring waiting rooms are enabled to maximize video visit security.
- PCMag: How to Prevent Zoom-Bombing — This article includes concrete tips on how to keep Zoom video calls secure and prevent them from being hijacked by hackers. It goes through settings like waiting rooms, making sure only the host can share their screen, and removing someone from a call.
Licensure and Reimbursement
The Centers for Medicare and Medicaid Services (CMS) and other payers have changed reimbursement policies in response to COVID-19. Further, licensure requirements for telemedicine vary from state to state. The resources below provide information about new telemedicine billing, coding, and licensure policies that are relevant for safety net hospitals and clinics during the pandemic.
- California Health Care Foundation: Reimbursing FQHCs for Telehealth Post-COVID-19 Pandemic – Medi-Cal’s Option — This report outlines policy options for California policymakers to consider as they determine the future of telemedicine reimbursement for FQHCs under the state’s Medicaid program, Medi-Cal. It also discusses how other states have approached Medicaid coverage for telemedicine, including both video and phone visits as well as e-consults and remote patient monitoring.
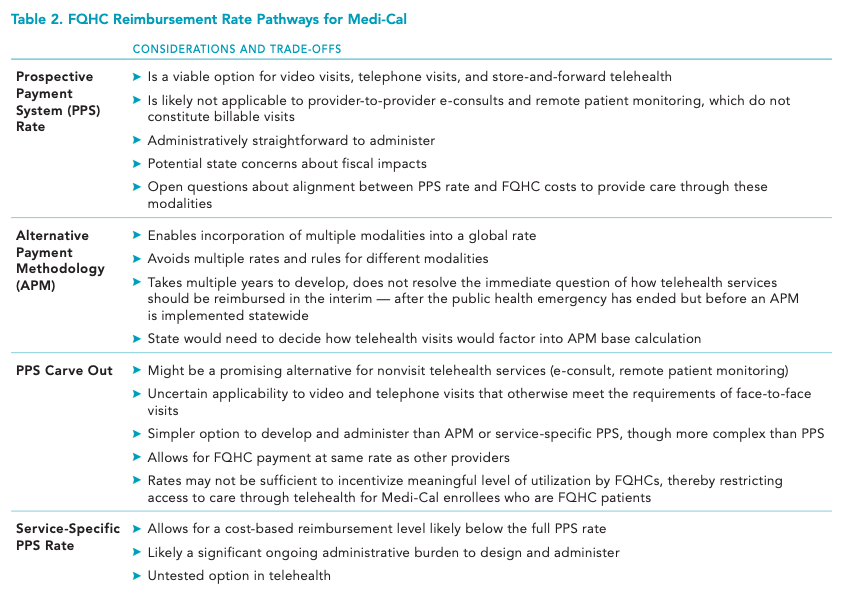
California Health Care Foundation
Resources from the Centers for Medicare & Medicaid Services:
- New and Expanded Flexibilities for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) During the COVID-19 Public Health Emergency (PHE) — This PDF has information about billing and coding policies for rural health clinics and federally qualified health centers during the COVID-19 pandemic. It includes sections on claims requirements, payment rates, cost reporting, cost-sharing, and more.
- COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing — This PDF has answers to frequently asked questions about Medicare fee-for-service billing related to COVID-19. The sections on “Expansion of Virtual Communication Services for FQHCs/RHCs” beginning on page 53 and “Medicare Telehealth” on page 59 are particularly relevant.
- Covered Telehealth Services for PHE for the COVID-19 Pandemic — This resource has a list of services payable under the Medicare Physician Fee Schedule when furnished via telehealth. A zip file of covered telehealth services during the COVID-19 public health emergency is available to download on the webpage.
Resource from the Center for Connected Health Policy:
- COVID-19 Related State Actions — This webpage has a continually updated database of COVID-19 related state actions taken by each state’s Office of the Governor, Medicaid Program, Medical Board, and/or Department of Insurance regarding licensure and telemedicine and their current status.
Technical Infrastructure and Vendor Considerations
Technical Needs. Provision of high-volume telemedicine requires appropriate infrastructure including high-speed internet connectivity and camera and microphone enabled devices. Multiple resources emphasize the importance of updating electronic medical record software in advance of telemedicine implementation.
- California Telehealth Resource Center: Telehealth Program Developer Kit — This PDF includes information about how to implement a telehealth program. Included on page 32 is a useful “Technical Needs Assessment” checklist.
- Health Information Evaluation and Quality (HITEQ) Center: Getting a New Workflow and Process Started during COVID-19 Pandemic — This is a link to download a PDF with information about getting a new telehealth workflow and process started during the COVID-19 pandemic. Included is a section called “Get Your Technology Together” with a step-by-step guide to internet speed and equipment needs.
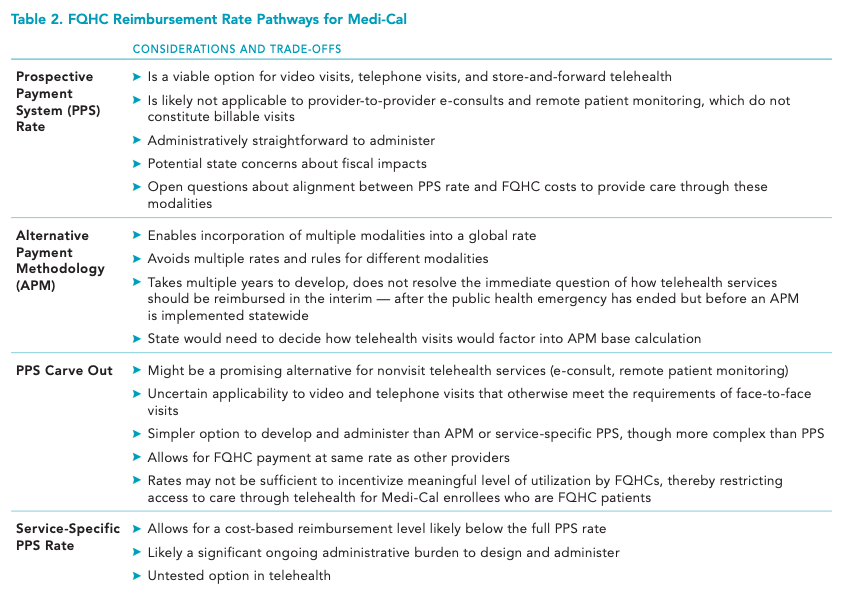
Vendor Selection. Many providers are looking to hire a telemedicine technology vendor to deliver virtual care for their patients during the COVID-19 pandemic. Key topics to consider when assessing potential telemedicine vendors include electronic medical record integration, HIPAA compliance, and good user experience for both patients and providers. The resources below offer guidance for the vendor selection process.
- Roots Community Health Center: Telehealth Vendor Evaluation — This is a link to download a spreadsheet with a list of questions to evaluate the functionality and usability of a potential telehealth vendor. The questions are divided into sections regarding technical requirements and hardware, patient digital experiences, training, support, and maintenance, equity-centered considerations, and financial considerations. This tool was created by Roots Community Health Center — a nonprofit organization founded in Oakland, California with a mission to uplift those impacted by systemic inequities and poverty through medical and behavioral health care, health navigation, workforce enterprises, housing, outreach, and advocacy — as part of their work through CCI’s Connected Care Accelerator.
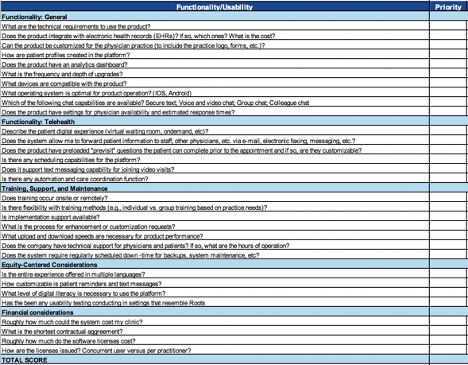
Roots Community Health Center
- National Organization of State Offices of Rural Health: Telehealth Technologies and Preparing to Select a Vendor — This PDF provides tips for selecting a telehealth vendor and includes a table of available vendors based on common types of telehealth technology.
- American Medical Association: Vendor Information Intake Form — This PDF can be used to compile information about a potential vendor using criteria about business, information technology, security, usability, customer service and clinical validation as a guide for technology vendor evaluation.
Impact on Quality Improvement Metrics and Payments
Health care quality measure sets have required modifications during COVID-19 to provide flexibility for care delivered remotely. Many measurement bodies and payers have approved adjustments to their measure sets for 2020 to align with recent telemedicine guidance from CMS and other federal and state regulators. The resources below provide information about how the HEDIS (health care effectiveness data and information set), PRIME (public hospital redesign incentives), and UDS (uniform data system) measure sets have been adapted for 2020-2021.
- National Committee for Quality Assurance (NCQA): HEDIS Measurement Year 2020 & Measurement Year 2021 Volume 2 Summary Table of Measures, Product Lines and Changes — This PDF summarizes HEDIS measurement years 2020 and 2021 changes to address when telephone visits, e-visits, and virtual check-ins are allowable.
- California Department of Health Care Services: PRIME Projects and Metrics Protocol — This PDF has information regarding the Public Hospital Redesign & Incentives in Medi-Cal Program (PRIME). For calendar year 2020, the PRIME transition metrics are most applicable as the PRIME program evolves into the Quality Incentive Program (QIP). These (here and here) may be helpful resources that outline the specific metrics.
- Health Resources & Services Administration (HRSA) Bureau of Primary Health Care: Telehealth Impact on 2020 Uniform Data System (UDS) Clinical Measure Reporting — This PDF is intended to help health centers determine how services to patients provided via telehealth should be considered for the UDS clinical measures. It includes a table to help health centers determine how services to patients provided via telehealth should be considered for UDS.
- Health Resources & Services Administration (HRSA) Bureau of Primary Health Care: Uniform Data System (UDS) Reporting Instructions for Calendar Year 2020 Health Center Data — This PDF describes the annual UDS reporting requirements for all health centers that receive federal award funds under the Health Center Program. The document contains instructions for telemedicine visits.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.