
![]()
As we continue to scale telemedicine approaches in the COVID-19 pandemic and beyond, there will be many advanced features that can be implemented and optimized for safety-net settings.
Key topics for optimization of telehealth include:
- Remote/home monitoring of patients to receive vitals (e.g., blood pressures, blood glucose) or patient-generated health data (e.g., symptom reporting) in real-time,
- Virtual modes of patient engagement and feedback,
- Population health management (e.g., management of entire patient panels for screenings and treatment via remote approaches), and
- Strategic planning to assess the current state of telemedicine programs and engage in continual improvement.
→ Want a more searchable and tagged version of this toolkit? Check out the Virtual Care Learning Hub!
Remote Patient Monitoring
Remote patient monitoring can be a valuable tool that complements telemedicine by allowing patients to record clinical data from home and transmit that information to their health care team. This can be particularly useful for chronic disease management. Below are resources on implementing remote patient monitoring.
- Community Clinic Association of LA County: Federally Qualified Health Center’s Remote Patient Monitoring Tool Kit — This toolkit includes a comprehensive guide to implementing a remote patient monitoring program within FQHCs. In addition to an overview of program components (operations, developing patient inclusion and exclusion criteria, referral and discharge workflows, and more), on page 18 it includes an example consent form and on pages 28-29 it includes sample patient and provider satisfaction surveys.
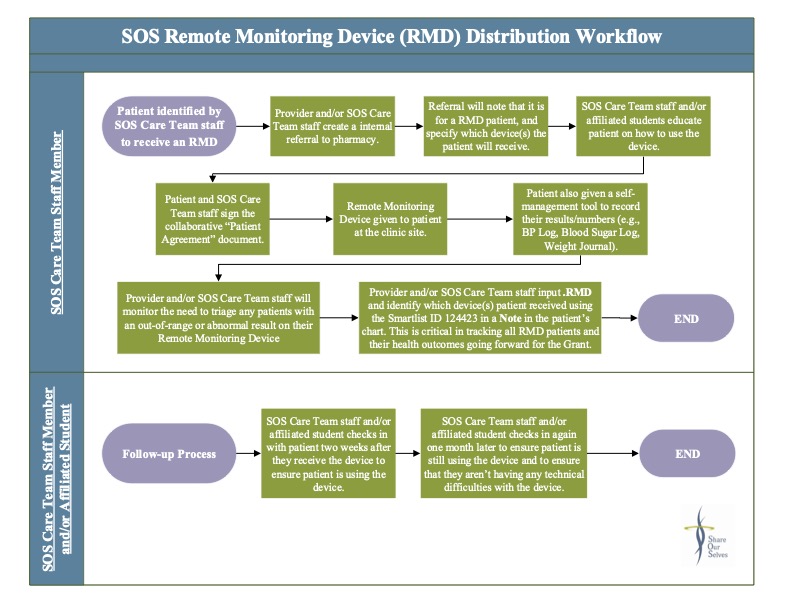
- Share Our Selves: Remote Monitoring Device Distribution Workflow and Patient Care Agreement — This workflow outlines the steps involved in distributing remote patient monitoring devices, including follow-up after the initial distribution. Also included is an example of a patient care agreement form used prior to distributing remote monitoring devices to patients in both English and Spanish. These tools were created by Share Our Selves – a nationally recognized health center, patient-centered medical home, and designated Healthcare for the Homeless provider in Orange County, California – as part of their work through CCI’s Connected Care Accelerator.
- American Medical Association: Digital Health Implementation Playbook — This PDF is a comprehensive guide to remote patient monitoring. It includes sections on before, during, and after implementation of remote patient monitoring. The appendices, starting on page 66, include useful templates to help at each stage of the process.
- Mid-Atlantic Telehealth Resource Center: Remote Patient Monitoring Toolkit — On this webpage you can watch videos outlining health care system stakeholders’ roles in successful implementation of remote patient monitoring, as well as download the toolkit as a PDF.
Patient and Team Satisfaction
Evaluating patient and health care team satisfaction with telemedicine implementation is important to ensure that the system is meeting patient and provider needs and that problem areas are identified for continued improvement. Patient advisory councils, one-time focus groups or feedback sessions, or in-depth interviews are feasible via telephone or videoconferencing. Engaging diverse and representative patient voices throughout telemedicine implementation is another strategy to enhance equity. Below are resources on assessing the telemedicine implementation process.
- Los Angeles County Department of Health Services: Post-Visit Patient Survey — This survey can be used to assess patients’ satisfaction with telemedicine, comparing their experience with video and telephone visits to in-person visits. It contains questions about patients’ experiences with telemedicine scheduling, wait time, quality of care, and how visit modality affects their sense of personal connection with clinicians. This tool was created by the Los Angeles County Department of Health Services — an integrated public health system that provides health services to residents of Los Angeles County, California and is the second-largest municipal health system in the nation — as part of their work through CCI’s Connected Care Accelerator.
- Northeast Valley Health Corporation: Case Study on Automating Patient Feedback Surveys During COVID-19 — This case study provides an overview of Northeast Valley Health Corporation’s process of developing an automated text message patient feedback survey, using the platform Feedtrail, to assess patients’ satisfaction with their phone and video visits and to gather their modality preferences (in-person, video, phone) for future visits. It also outlines NEVHC’s text message-based campaigns, in English and Spanish, to increase the number of pediatric appointments. This case study features Northeast Valley Health Corporation — a Federally Qualified Health Center with 14 sites in the San Fernando and Santa Clarita valleys in Los Angeles County, California providing medical, dental, and behavioral healthcare for uninsured and medically underserved patients with limited financial resources — and highlights their work through CCI’s Connected Care Accelerator.
- White Memorial Community Health Center: Patient Feedback Survey — This short survey, in both English and Spanish, asks patients to assess how satisfied they are with the treatment they receive via video appointments and whether they would recommend video appointments to their family and friends. This tool was created by White Memorial Community Health Center — a non-profit health center in Los Angeles, California that provides primary healthcare services to children, adults, and seniors regardless of patients’ ability to pay — as part of their work through CCI’s Connected Care Accelerator. To learn more about how White Memorial improved video visit infrastructure and assessed patient satisfaction with telemedicine, check out this case study.
- American Academy of Family Physicians: A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice — This PDF provides a comprehensive guide to developing and improving a telemedicine program. Page 30 has a sample patient satisfaction survey covering the scheduling process, pre-visit support, and the telemedicine visit itself.
- American Medical Association: Telehealth Implementation Playbook — This PDF outlines many components of the telemedicine implementation process. On pages 119-123 there are templates for gathering feedback from the implementation team, clinicians, and patients on their experiences with telemedicine.
- Center for Care Innovations: Innovative Models of Patient Engagement — This webinar discusses a diverse online/virtual member experience advisory council at the Colorado Department of Health Care Policy and Financing that provides feedback on operations. The discussion of online advisory councils begins at the 28:00 minute mark.
Strategic Planning
Virtual Care Strategic and Tactical Deployment Maturity Self-Assessment Model — This tool, created by Jim Meyers, DrPH, is designed to help safety-net healthcare sites assess the maturity of their virtual care programs. It includes a detailed matrix of indicators covering leadership and governance, technology platforms, virtual care operations, and health equity to assess whether a virtual care program is in a basic, foundational, or advanced stage. It also includes a task or function-oriented matrix to assess program maturity, including common virtual care tasks before, during, and after the visit; patient portal functions; provider-to-provider functions; and health center-to-community functions. For additional information about this tool, feel free to reach out to Meyers at 510-761-1609 or [email protected].
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.





