OVERVIEW
California is embarking on a fundamental shift in how it pays for health care. For you, this pivot from volume-driven payments to capitation through the alternative payment methodology (APM) pilot will create both significant challenges and important opportunities to provide more effective and efficient care.
To better prepare the state’s Federally Qualified Health Centers (FQHCs) for this transformation, we partnered with the California Primary Care Association (CPCA) and California Health Care Safety Net Institute (SNI) to launch the Capitation Payment Preparedness Program—also known as CP3. CP3 provides technical assistance around three core competency areas:
- Population health management
- Data management
- Financial management
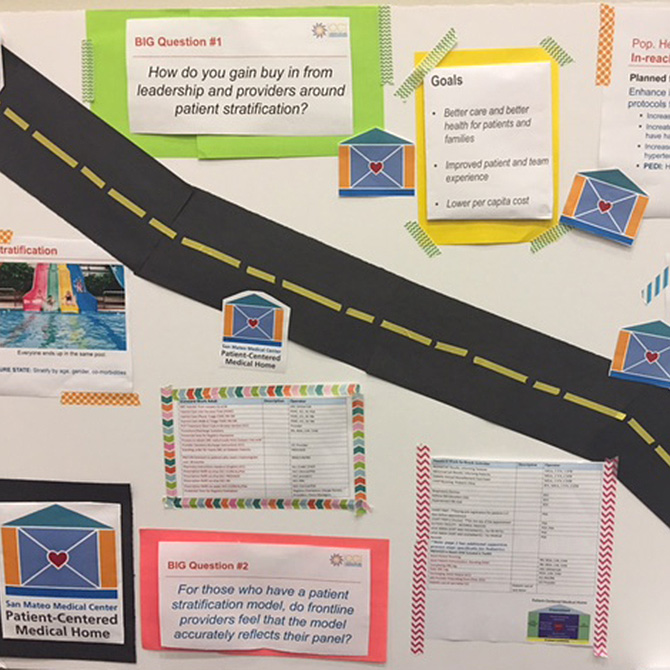
We lead CP3’s Population Health Management Technical Assistance Program. Our primary goal is to transform care processes and systems to achieve high-value, quality health care. This means providing the best possible care and patient experience while simultaneously reducing unnecessary costs to the health system.
Patients are accessing their care team in a variety of ways—visits to the clinic, email, phone, and online portal interactions. At the same time, care teams are proactively assessing and addressing the needs of their patients, and increased flexibility is needed to build a workforce to fit those patient and community needs, including reaching out to licensed and unlicensed staff to address bio-psycho-social needs. Many FQHCs have already started this transformation work by adopting the patient-centered medical home (PCMH) model. However, that work is constrained by current reimbursement rules of prospective payment system (PPS) that pay for visits with “billable” clinicians rather than paying for interactions with other members of the care team based on patient needs.