I’d like to share with you a framework describing what it takes to support high-value health care in safety net clinics.
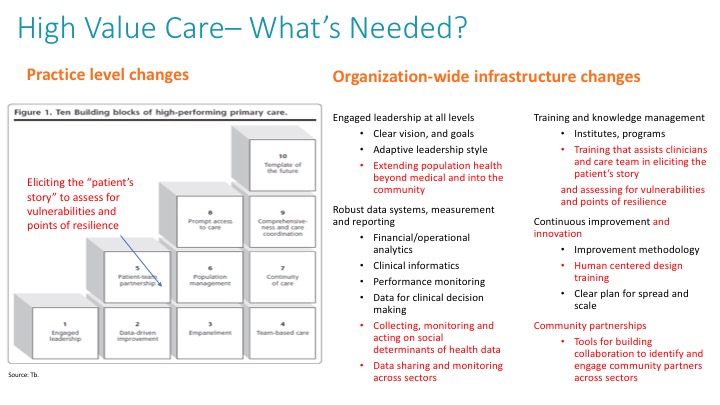
Developed at CCI earlier this year, incorporating our collective experience and the input of expert faculty, it considers the care delivery changes that are needed and well-established by Tom Bodenheimer’s 10 Building Blocks of High-Performing Primary Care. However, we added several foundational skills and organizational infrastructure to sustain these changes.
We realized that to truly impact the health of our patients and communities, we need to understand the socioeconomic and political contexts in which our patients live, work, and play. We need to focus on their cultural backgrounds, as well as the comprehensive wellbeing of their families. We also need to consider that patients are people with vulnerabilities and points of resilience that, if identified and leveraged, will help them better manage their health.
We developed this framework because there was no single source that summarized the changes clinics need to make at both the practice-site and organization levels to manage population health in a value-based payment environment. Today, we now use it as our “content theory,” or “change package,” for our CP3 Population Health Management program, a yearlong program focused on preparing federally qualified health centers (FQHCs) for value-based care and payment. Health centers have a critical role to play to ensure the care we provide leverages patients’ strengths and acknowledges their vulnerabilities.
Let’s start with the 10 original building blocks:

This initial framework includes evidence-based changes well described by Bodenheimer and his colleagues in various publications.
But the four infrastructure changes at the organization level that we have found to be critical in sustaining value based care are:
- Engaged leadership – Leaders provide resources and protected time for care teams to do the work and continuously improve it. These leaders also subscribe to adaptive leadership principles. They leave their ego at the door, see their people as assets and engage them in identifying and problem solving around “adaptive challenges.” These leaders view change as a constant part of their job.
- Robust data systems, measurement and reporting – Data is an asset to the organization and is used to drive business and clinical decision making. The right systems, people, and processes are in place to help care teams perform in their roles and carry out tasks that are vital to improving care.
- Training and knowledge management – There are processes, trainings and systems to support dissemination of knowledge and information. There is also a process for updating and disseminating that information based on what we learn and change.
- Continuous improvement – Using improvement science to identify problems and their root causes, establish goals and metrics to evaluate changes, use Plan-Do-Study-Act (PDSA) cycles to test and implement changes, and adjust approaches based on the lessons learned from continuous measurement.
As we put the framework into practice, we realized that it didn’t go far enough to address the factors that influence the health and wellbeing of populations.
Health care accounts for only 10 percent of patient outcomes, whereas 60 percent is explained by individual behavior and social determinants of health (SDOH) factors. The current framework places an emphasis on the 10 percent, principally the medical model for producing healing and wellness. We saw a missed opportunity in not addressing the changes clinics need to make to support patients in being their best selves.
It starts with a change in mindset, one that engenders curiosity and a willingness to explore different roles and more meaningful ways of connecting with patients and providing care. It means eliciting patients’ personal stories to learn about them as people, discover their vulnerabilities, and learn about their points of resilience. It requires us to start thinking about new community partners that can help us think more broadly about population health, going beyond physical wellbeing to include other dimensions of wellness – social, emotional, intellectual, financial, and spiritual – that are influenced by the larger community. By going there, we can all develop stronger, therapeutic alliances with patients and their communities to bring about a higher state of health and wellbeing. Current quality improvement methods help us make things better by improving processes and systems. When we want to rethink our roles in providing care, we must disrupt current processes and innovate to create new solutions to address patients’ needs.
To that end, we offer the following changes to the framework:
- Emphasize hearing patients’ stories to assess vulnerabilities and resilience as part of the patient engagement building block.
- Define population health management more broadly to include community health and partnerships.
- Collect SDOH data directly from patients and through cross sector partnerships.
- Add a new domain under the organization level — community partnerships — to stress the importance of working with community-based organizations to provide whole person care.
Click to download: High Value Care — What’s Needed?
Our new framework builds on my experience working in the commercial sector managing value-based care programs and teams for a high-performing, financial-risk-bearing independent physician association in San Francisco, my years of coaching clinics on care delivery transformation, and my work at CCI directing the CP3 Population Health Management program.
As we move forward in our future programming, we will continue to think about this framework here at CCI and in the communities we serve. We welcome your thoughts on how you might strengthen this framework based on your own experiences.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.