More than 25 million Americans are suffering from chronic pain, and the overprescribing of opioids to treat these patients is helping fuel to the country’s growing opioid epidemic.
Doctors now face a critical challenge: How can we create better pain treatment and management strategies? Riverside University Health System’s solution was to build a comprehensive opioid screening tool into its electronic health record.
Screening for Risk
Five years ago, Riverside University Health System, who is in our Technology Hub, kickstarted a major initiative to look at how it was prescribing opioid medication. At the time, there wasn’t an organization-wide policy on screening and managing chronic pain patients. So a group of doctors and pharmacists came together to develop best practices.
The team looked at what providers should be doing during each visit. They tackled the question of what tests they should order and what key metrics they should be recording. They also set out to establish expectations between the provider and the patient; this included a timeline of the course of treatment, how to quantify pain, patient risk stratification, referrals, and achieving patient goals.
The resulting assessment template — printed on paper back in 2013! — has since evolved into an easy-to-use toolset, called “Chronic Opioid Activity,” that’s integrated within Riverside’s Epic electronic health record (EHR). Over time, Riverside has minimized the amount of clicking and typing required to do this work. The system now anticipates what providers need and has eliminated much of the duplication.
Riverside continues to get feedback from its providers on how to streamline and improve the screening process. And just weeks ago, it rolled out the third version of the tool.
This update arrived at a pivotal moment in the opioid crisis. An estimated 40 percent of opioid overdose deaths involved a prescription opioid, and more than 46 people are dying every day from overdoses involving prescription opioids.
How It Works
- When a provider starts a visit with a patient, a Best Practice Advisory notification automatically pops into the EHR. (The provider can also manually activate the toolset.)
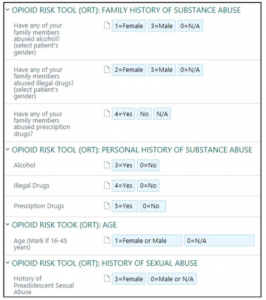
- First, prompts the provider to ask a series of screening questions. This covers the:
- Opioid Risk Tool (ORT) to assess the risk for opioid abuse
- CAGE questionnaire to test for problem drinking and potential alcohol problems
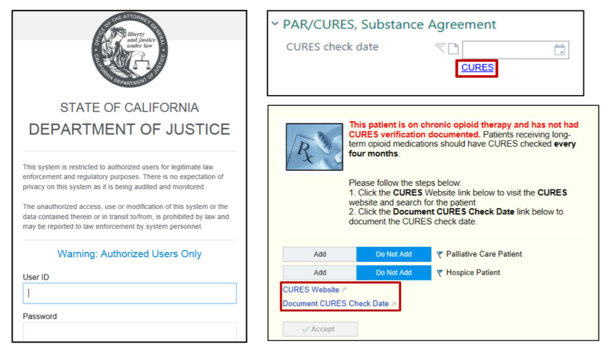
- The tool then accesses California’s prescription drug monitoring program (PDMP), which is called Controlled Substance Utilization Review and Evaluation System (CURES). This electronic database that tracks controlled substance prescriptions in the state, allowing the provider to use the patient’s prescribing history to better inform next steps.
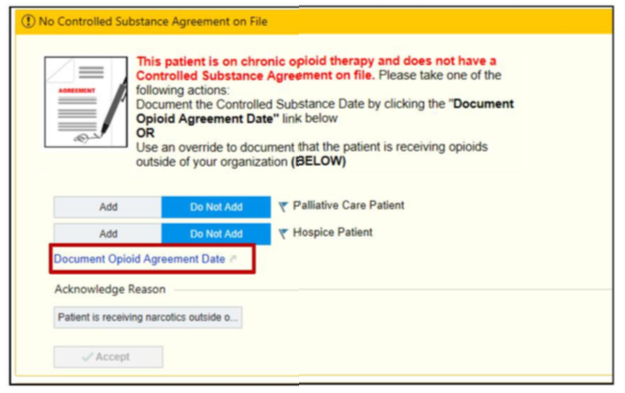
- The tool then asks if there’s a patient-provider medication agreement, also known as an “opioid contract” or “pain contract,” on file. This agreement is designed to create an open conversation between the patient and the prescriber about the benefits, risks, and limitations of opioid medicines. It also outlines the process that Riverside follows in starting, continuing, changing, or discontinuing these medications.
- The tool links to a Morphine Equivalent Daily Dose (MEDD) calculator, which automatically calculates prescriptions within the EHR. This calculator can be used as an indicator of potential overdose and other dose-related risks for adverse drug reactions. An ad hoc version MEDD calculator also allows providers to evaluate any changes to medication management.
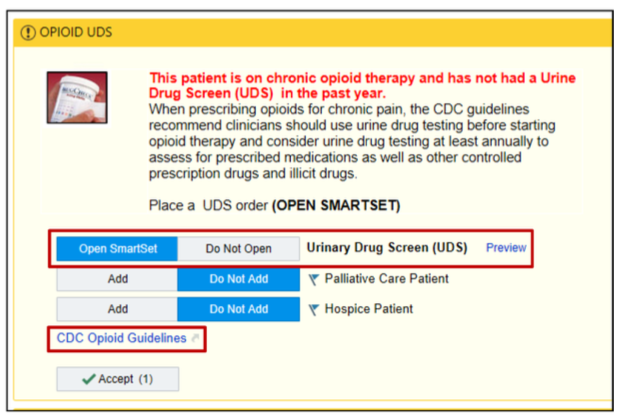
- The screening tool reminds the provider that patients starting opioid therapy should have a urine drug screening test at least once a year. This allows the provider to evaluate the patient’s use of other controlled prescription drugs or illegal drugs.
- The tool gives the provider multiple referral options. For instance, the patient may need to see orthopedics, physical therapy, the spine clinic, or behavioral health.
- The tool tells the provider when the patient should return for the next pain assessment.
- Lastly, the tool autogenerates a progress note with all the aforementioned information to close out the visit with the patient.
Reception
Riverside understood that you can’t just push out a new platform and expect the staff to know how to use it. Rolling out this screening tool to 10 Federally Qualified Health Center (FQHC) clinics, as well as two family medicine clinics and one internal medicine clinic based at the medical center, required quite a bit of training.
The project team came up with a workflow, so everyone knew their individual roles in this new initiative. They won the buy-in of clinic managers, spoke at every department meeting, and conducted several pilots. Most importantly, the team clearly explained the benefits of the tool for the staff and their patients.
Today, providers enjoy that they no longer have to memorize the long list of screening questions. They especially like the EHR’s ability to generate data and reports on their own progress.
“Providers are getting credit for the work they’re already doing. It’s elegant and easy to access,” said Dr. Edward A. Bacho, who works as one of the associate medical directors of the Outpatient Community Health Center EHR, co-chair of the Outpatient Informatics Committee, and an EHR physician champion.
Dr. Khang Myint and Dr. Edward A. Bacho
On the patient side, the project team encountered bigger hurdles to adoption. At first patients felt like Riverside was targeting them. The general feeling was, “I’m just in pain — why are you making me jump through so many hoops?”
But over time, the tool established a rhythm to visits, so patients can expect to hear these screening questions — it’s a lot less jarring. And now that the opioid crisis is all over the news, patients more clearly understand the risks. Today there’s very little resistance.
“The patients are asking for their urine drug screening cups ahead of time. They ask if it’s time to sign the medication agreement. It’s amazing. They’re very open to it,” said Bacho.
What’s Next?
This isn’t a complete solution. Riverside has several items on its to-do list. For the fourth version of the tool, the health system is working to develop:
- A pre-visit screener where patients can enter information about their pain. This will help identify risks and help staff plan prior to a visit.
- Primary chare chronic pain management algorithms
- Opioid weaning algorithms
- Integration with medication-assisted treatment (MAT)
- Collaboration with the emergency department. The goal is to counsel patients and guide them into primary care for pain management.
- Collaboration with the Centers for Excellence in Chronic Pain
- Patient outreach tools
- Data-driven action
Learn More
Riverside University Health System has been the foundation of health care, community wellness, and medical education in California’s Riverside County for more than 100 years and employs about 6,000 team members.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.