Healthcare changes slowly. Many of the principles we discussed while I was a part of the Clinton Task Force on Healthcare Reform in the early 90’s have just been implemented in the ACA. One of the first uses of tablet computers in healthcare was a project that I implemented at Stanford in 1992. In the HIPAA work group we established legislation passed in 1996 that we are still struggling with today. Some days I feel like Sisyphus pushing the large boulder up the unending hill.
Is there a way to make the change process faster? What if we pioneered new operating principles for healthcare not in far off ivory towers, but right in very organizations that treat our most vulnerable patients? Could we short-cut the plodding pace of change? It was a powerful idea, but first we needed to know: was innovation even possible in the resource- and time-constrained environment of the safety net?
About three years ago a small group of visionaries got together at CCI to ask a three questions:
- How can we develop a way for the safety net to organize, identify, test and implement innovative changes to the healthcare delivery system in a real life setting, without the investment of millions of dollars to create an innovation center?
- How can we capitalize on all of the innovative ideas that our safety net staff use every day, out of necessity, to meet the needs of our patients?
- How can we share our results across the entire safety net space so that others can take advantage of what we are learning?
With these questions in mind, we found ourselves at a beginning.

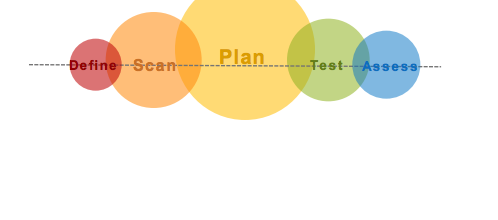
Over the last two years we created four Innovation Hubs embedded in safety net organizations. These Hubs are staffed and operated by a group of bright, curious, committed folks, who are planning, testing and evaluating innovations in addition to their day job. To date several hundred possible innovations have been reviewed in the areas of patient access, patient engagement, management of complex patients and big data application to clinical decision making. From this huge pool of possible innovations, about forty different possibilities deserved a closer look. Of these about a dozen have been in testing and evaluation with real patients and providers.
Along the way, we have learned:
- How to work around IT vendors that are reluctant to share data.
- The importance of really understanding the impact innovation work has on clinic workflow.
- The importance of human centered design.
- The importance of tools learned in our Catalyst programs.
- That it doesn’t take a lot of money to start and operate an Innovation Hub.
- Creative ways to fund our activities.
- That we can succeed.
While we have not yet really left the beginning far behind, we think we can see the start of an effective model for innovation in the safety net.
Now we are compelled to share everything that we have learned to date. We have shared tools and in our perspectives we discuss innovation in the safety net, share the successes, learn from the failures, and share how to go about the innovation process through blogs, podcasts, weekly emails, and learning opportunities.
How can we help you get started in developing and implementing an Innovation Hub in your organization? Let us know so you can build upon our successes and our failures.