As with many other clinics, Olive View found there was limited awareness of advance care planning amongst care teams and patients. Additionally, it was a difficult and sensitive topic that many providers found challenging to discuss with patients, especially if there were medical comorbidities that competed for the providers’ attention and time during the primary care visit.
Since Olive View had successfully implemented group visits for chronic conditions and age cohorts in the past, it decided to pilot group visits for advance care planning.
Group visits were an enticing care model because of enhanced access, efficiency, patient-engagement, and clinical outcomes. Olive View knew that group visits create social cohesion among patients and improve provider and staff satisfaction. Moreover, group visits would provide focused, patient-centered care to vulnerable populations.
Designing the Pilot
Olive View launched the advance care planning group visit model in their Los Angeles County Department of Health Services primary care clinic. Nine providers participated in the pilot.
Providers identified appropriate patients, then their medical assistants contacted patients to tell them about the session and invite them bring a guest, like a caregiver or family member.
These one-hour group visits were embedded in a regular clinic session and were led by physicians, along with a social work staff person. (Other kinds of group visits, like diabetes for example, are led by nurse practitioners and have had challenges recruiting both team members and patients.)
During group visits, patients were assisted in completing an advance directive, which includes a living will and durable power of attorney for health care. Living wills describe a person’s desires regarding their medical treatment (wanted or not), while and the durable power of attorney for health care designates an individual to make decisions on behalf of the incapacitated patient.
Group visits focused on adults older than 65 years old, “geriatric” patients, but could also include younger adults with frailty and complex comorbidity. At least three patients and their family members/caregivers were recruited for each group visit.

Milestones During Implementation
Start-up and planning
- Olive View identified key roles for the pilot including two physician co-leads, who served as leaders for the clinic and for this project. Other roles included a nurse manager and the nine providers, their MAs, and a palliative care social worker.
- From the beginning, it was made clear that providers would be leading group visits, testing them, and then rolling them out the wider organization. This is a departure from other group visits, which are led by nurse practitioners.
- Previously, there was a disconnect between the clinic and the social work department, resulting in gaps in services. The pilot was a great opportunity to improve that relationship. This interdisciplinary approach to advance care planning is important because patients may be suffering not just from physical problems, but also problems associated with psychological, social, spiritual, and financial concerns. They can also provide grief counseling for pre-bereaved or bereaved family members.
- The team engaged the social worker early on. She become a key part of the planning process, especially in developing the toolkit and facilitation slides.
Testing
- The team conducted two large all-clinic trainings, where they introduced a group visit toolkit and strategies for recruiting patients. The toolkit includes:
- A provider group visit facilitation guide, plus an accompanying slide presentation
- Medical assistant group visit invitation script
- Group visit agendas
- Pre- and post-visit surveys for patients and guests
- Group visit confidentiality consent
- Provider documentation and billing guide
- Tracking for patient and guest demographics, patients contacted, patients booked, show rate, and advance health care directive completion
- Patient participation varied depending on a providers’ recruitment strategy and time invested. Some providers would talk with the patient during a regular visit. Others had the MA call patients on a list and say that their provider would like them to come back for a group visit on advance care planning, which didn’t work as well. The percent of patients who booked group visits ranged from 20 percent to 90 percent.
- The first cohort of four providers demonstrated successes in recruitment and conducting the group visits. They debriefed the results of the group visits in at a large staff meeting, which gave the pilot momentum. Learning from this feedback, the next cohort of two providers implemented group visits three months later. And the final three providers implemented their pilot one to two months later.
- Patients often had many health needs that required specific one-on-one primary care provider discussion during the traditional visit. This which made it challenging for the provider to find the time to provide education, counseling, and guidance on advance care planning and completion of the advanced health care directive.
Benefits of Advance Care Planning Group Visits Pave the Way for Spread
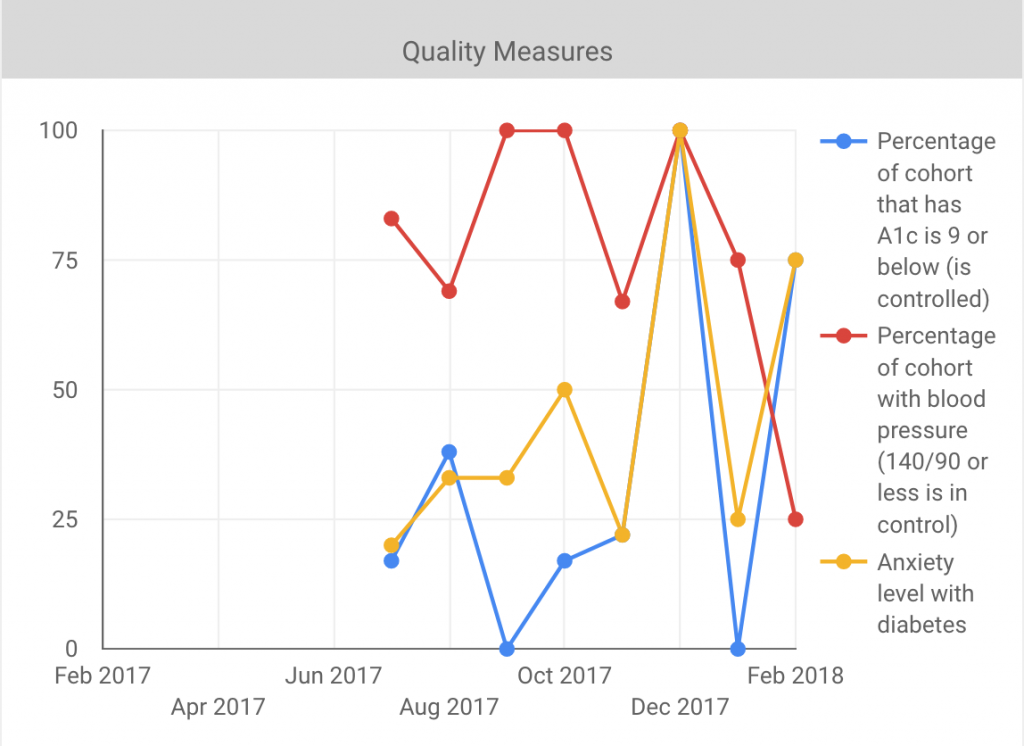
Despite advance care planning being a challenging topic to address and targeting a patient population with typically higher no-show rates, Olive View achieved productivity levels similar to usual care (average of 2.7 patients/hour). After five months, 26 percent of patients completed an advance directive.
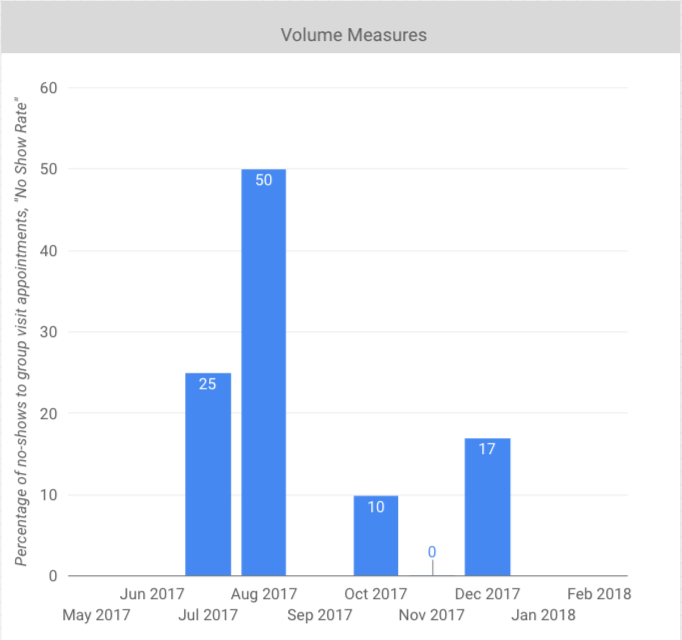
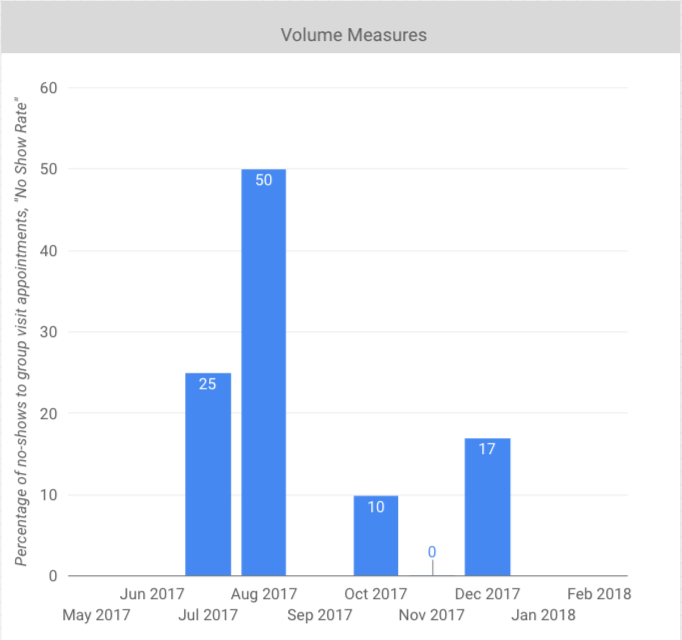
No shows varied across the different group visits.
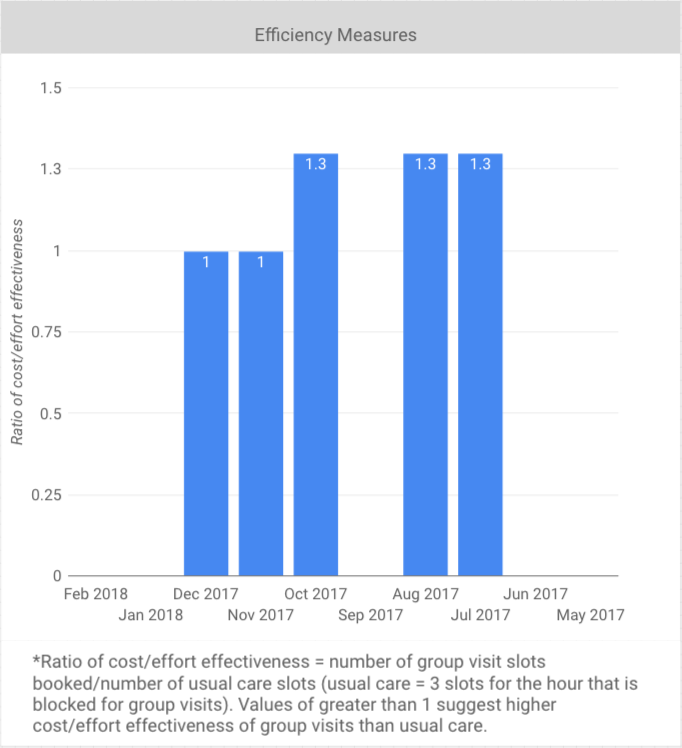
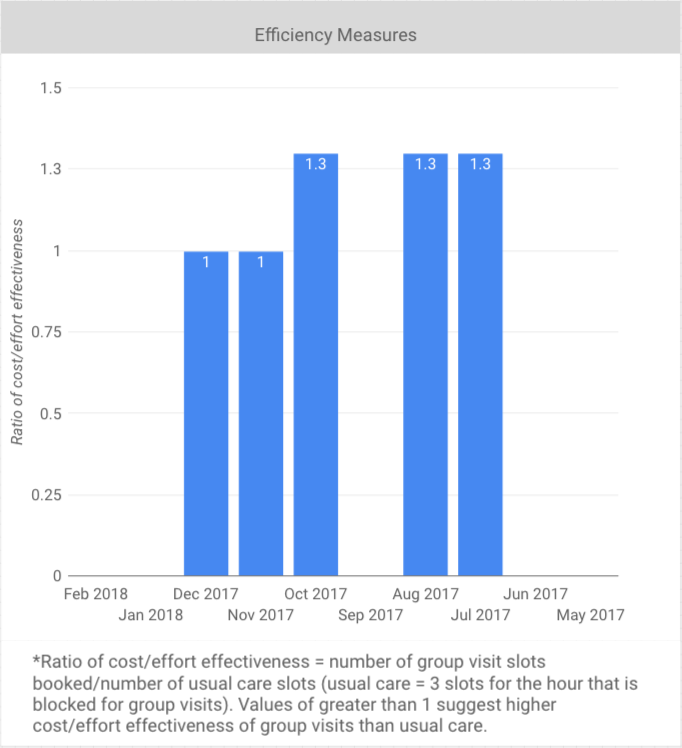
Olive View measured the ratio of cost/effort effectiveness, which was calculated as the number of group visit slots booked divided by the number of usual care slots. The results of greater than 1 suggest that group visits have higher cost/effort effectiveness than usual care.
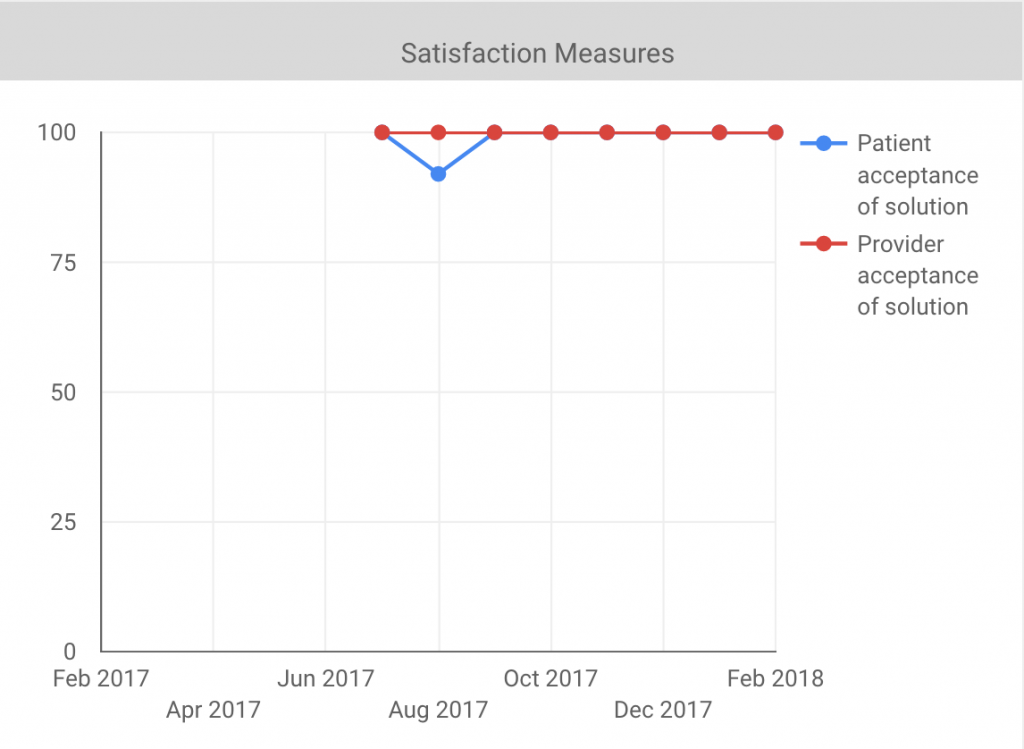
Patient and provider/staff satisfaction was high:
- 100 percent of patients and guests strongly agreed that they would recommend the group visit to other patients.
- 94 percent of care team members strongly agreed that the group visits are a means to provide higher quality care and improve relationships with patients.
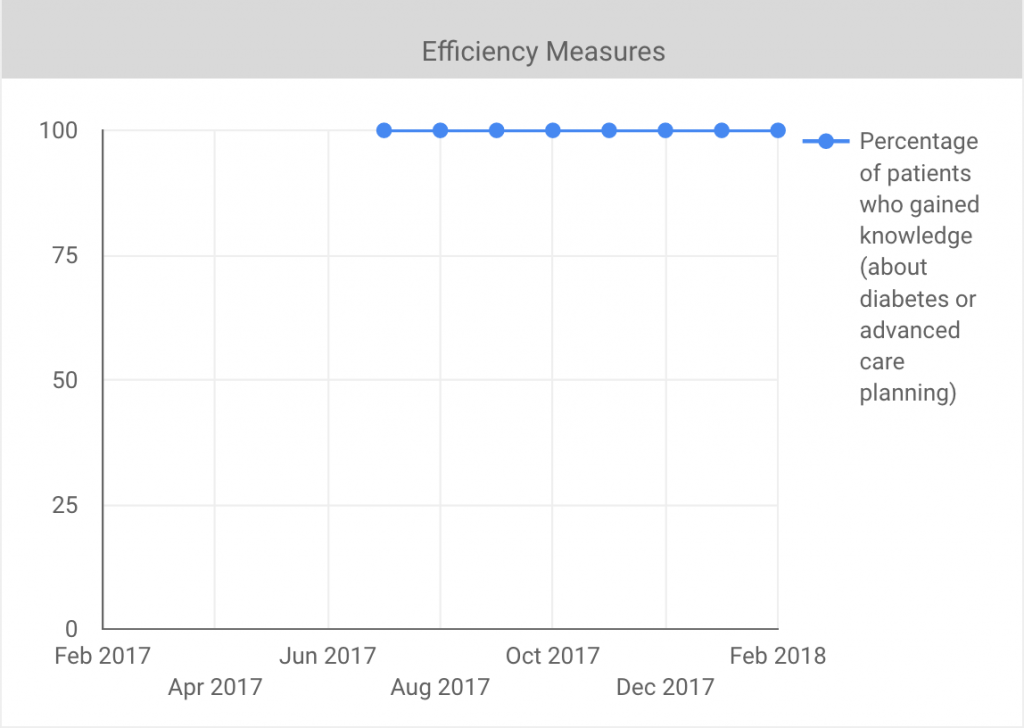
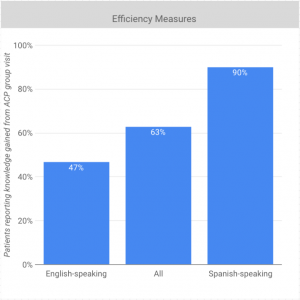
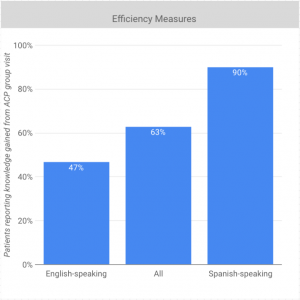
Knowledge increase as measured by the question “Do you know what an advance care plan/directive is?” varied by group visit over time and averaged 63 percent overall, with 90 percent amongst Spanish-speaking patients and 47 percent amongst English-speaking patients.
Success Factors
-
- Clinica Family Health was invaluable. Its materials were well-curated and generously shared. Clinica Family Health was also very responsive, supportive, and helpful to the team if there were any questions they had throughout the program. A compilation of materials and resources can be found here and here.
- Assessing patient and provider satisfaction helped the team see the true value of group visits.
- Creating a plan for implementation is an important way to structure the work and keep momentum going. For instance, set up clear goals about how many group visits and with which providers and clinics. Design measures and a data collection plan, especially for patient feedback. Establish team meetings to hold each other accountable for results and timelines. Provide peer-to-peer coaching.

Key Advice to Organizations Considering Implementing Group Visits
-
- Invest in laying a foundation. While creating a toolkit and attending the training at Clinica Family Health was time consuming, it was vital to a successful launch.
- Give primary care providers hands-on training for conducting group visits. The ideal scenario would be for providers to shadow a group visit with your target population. You can also enlist an experienced facilitator provide on-the-ground training at your clinic.
- Complex topics, such as advance care planning where patients face end of life decisions, necessitate an interdisciplinary approach. Engaging a social worker in facilitating group visits ensures that you’re focusing on the psychological, spiritual, social, and financial aspects.
- When going on a “site visit,” where you learn from an exemplar organization, be sure attendees bring back pictures, videos, and stories to inspire other staff and providers.


 East Valley Community Health Center, located in Pomona, Calif., has five clinics and approximately 22 providers. It serves the San Gabriel and Pomona Valleys in the Greater Los Angeles Area, where the majority of residents are Hispanic. In preparation for payment reform, they are implementing multiple strategies to improve the quality and efficiency of health care delivery, such as
East Valley Community Health Center, located in Pomona, Calif., has five clinics and approximately 22 providers. It serves the San Gabriel and Pomona Valleys in the Greater Los Angeles Area, where the majority of residents are Hispanic. In preparation for payment reform, they are implementing multiple strategies to improve the quality and efficiency of health care delivery, such as