Diabetes, heart disease, and hypertension are among the biggest scourges of low-income communities. Left uncontrolled, these diseases can cripple and kill people long before their time.
 Fifteen years ago, Kaiser Permanente in Northern California — later joined by CCI — decided to tackle these deadly diseases with an innovative safety net program called Preventing Heart Attacks and Strokes Everyday (PHASE).
Fifteen years ago, Kaiser Permanente in Northern California — later joined by CCI — decided to tackle these deadly diseases with an innovative safety net program called Preventing Heart Attacks and Strokes Everyday (PHASE).
As part of the mission of PHASE, for which CCI became the program office in 2015, clinicians deepened their team-based care efforts, quality improvement skills, health equity interventions, and data tracking to help close the health gap. During the COVID-19 pandemic, they also expanded their care beyond the four walls of the clinics by helping patients monitor their own blood pressure and keep their blood glucose under control, with impressive results.
As Kaiser wrapped up the program this spring, participants gathered online to commemorate this last leg of the PHASE journey and of its partner program known as TC3 (short for Transforming Cardiovascular Care in Our Communities). “There is much to celebrate as we look back on our accomplishments and growth,” said Julianne Tomlin, PHASE’s senior manager. Before the pandemic hit, she reported, PHASE was reaching a record number of patients. The clinics and hospitals that belonged to PHASE helped 120,000 patients with hypertension control their blood pressure and nearly 89,000 patients with diabetes reduce their A1c levels.
“As a faculty member, I’ve been able to watch all these safety net clinics navigate through a very, very difficult year due to COVID,” said Michael Mulligan, former director of Chapa De Indian Health and faculty for the PHASE and TC3 programs. “It’s been a real privilege to see the heart and soul of these safety net clinics as they weathered through this together.”
This sentiment was echoed by Dr. Marc Jaffe, an endocrinologist and head of the Hypertension Task Force of Kaiser Permanente in Northern California, who served as a co-founder of PHASE. Participants should be proud of their work and its “fantastic results,” he declared.
Here are just a few of the many highlights shared at the gathering:
Closing a gap in equity through self-monitored blood pressure: Chapa-De Indian Health
 Many patients at Chapa-De Indian Health, a PHASE-affiliated clinic based in Auburn, California, struggled to control their hypertension in the early days of the pandemic, and the center saw an overall drop in blood pressure control. Clinic staff did whatever they could to help patients remotely. “We recognized that a key role of ours was to protect those most at risk of developing severe complications [of the disease],” said Director of Quality Improvement Brandon Bettencourt, RN.
Many patients at Chapa-De Indian Health, a PHASE-affiliated clinic based in Auburn, California, struggled to control their hypertension in the early days of the pandemic, and the center saw an overall drop in blood pressure control. Clinic staff did whatever they could to help patients remotely. “We recognized that a key role of ours was to protect those most at risk of developing severe complications [of the disease],” said Director of Quality Improvement Brandon Bettencourt, RN.
Chapa-De’s American Indian patients had poorer blood pressure control than non-American Indian patients, according to the clinic data – an inequity that clinicians vowed to fix. After a few attempts to close the gap, including drive-through blood pressure tests (which were ultimately discontinued due to inconsistent use by patients), the clinic began teaching all its hypertensive patients how to monitor their blood pressure at home, an approach called self-monitored blood pressure, or SMBP. This has entailed sending out hundreds of blood pressure cuffs to patients with high blood pressure, ensuring the right fit, and regularly recording patients’ reports of their blood pressure readings.
Chapa De’s aim was to achieve 77 percent blood pressure control among patients enrolled in the SMBP program by the end of the program – the same rate the clinic had achieved before the pandemic. Their longer-term goal is to eliminate disparities in blood pressure control between American Indian and non-American Indian patients by December 31, 2022. Changes the clinic made included sending BP cuffs to all patients with high blood pressure; sending out larger BP cuffs for people whose arms were larger than standard measurements; and involving clinical pharmacists in teaching patients how to do the BP readings.
“We were surprised by how willing patients were to receive care virtually, and how much they liked it. We were also surprised by how quickly our clinical staff adjusted,” said Bettencourt, who noted the SMBP program empowered patients and helped them take control of their health. “Patients have told us how much they like the program, and they have better BP control than those not in the program” – the latter something that was reflected in the data collected (see slide below).
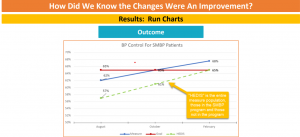
He and other staff are also gratified that their work on self-monitoring with American Indian patients has helped narrow the disparity in blood pressure control at Chapa-De. “We learned that the process of change can be accelerated by a crisis,” added Bettencourt. “However, making those changes stick once the crisis has passed is not easy.”
Learn more about Chapa De’s project here.
“Taking Cardiovascular Care HOME”: Los Angeles County Department of Health Services
The Los Angeles County Department of Health Services, a TC3 participant, provides care to those most likely to suffer the ill effects of hypertension, including low-income Hispanic and African American patients. More than 87,000 of its patients have hypertension, and in that group, more than 67,000 also have diabetes. One third of patients with hypertension do not have adequate blood pressure control. The COVID-19 pandemic accelerated the need for remote care, and the LACDHS came up with a striking innovation: nurse-run centers to work with patients on home blood pressure monitoring and control.
Many African Americans have underlying health conditions (such as high blood pressure, asthma heart disease and diabetes) that may put them at greater risk to serious illness from #COVID19. pic.twitter.com/w0Kn4WHDno
— LA Public Health (@lapublichealth) April 28, 2020
This is how it works: Patients whose blood pressure is uncontrolled for a period of six months are referred to registered nurses who are specifically trained and certified to titrate (that is, to continually measure and adjust the dosage) hypertension medication to help patients reach their blood pressure goals. Patients are given automated blood pressure cuffs, which they use to do self-monitored blood pressure (SMBP) readings, which show up as distinct data and display elements in the health system’s electronic health record. The nurses adjust the hypertension medication in person or remotely by phone or video, using the self-monitored and in-clinic results. One of the exciting findings: Most patients were able to hit their blood pressure goals in fewer than two visits.
“RNs are empowered to work at the top of their licenses, which improves care quality and timeliness,” said LACDHS Research Analyst III Laura Myerchin Sklaroff, MA. In addition, patients appreciated the care and support, according to patient surveys. “I thought [the nurses] didn’t care about us, but now I realize they are very caring and I’m very happy about their care,” one patient wrote. Another patient wrote in support of phone visits: “Due to the pandemic, regular phone calls are better. I am homeless I do not have transportation so calls work for me.”
The department’s original aim was to improve blood pressure control by 10 percent by the spring of 2021. To that end, the team developed a dashboard that allowed staff to drill down to primary care physician (PCP) level metrics to key indicators that can be tracked over time. Another innovation was finding a way to pull in patient readings to save as documentation notes in patients’ charts – “a really big staff favorite,” said Sklaroff.
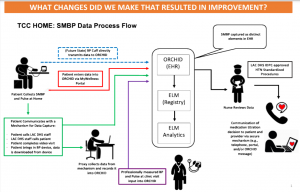
From the LACDHS’s presentation on SMBP during the pandemic
COVID-19 was the biggest barrier to project goals, since the pandemic not only required the health system to switch to remote care almost overnight but to pull RNs working on the project into emergency care. “The project has been interrupted three times by three surges” of COVID, said Jeffrey Guterman, MD, the chief research and innovation officer in ambulatory at LACDHS. The most frustrating thing has been getting up to speed, having the momentum, and having to tell dozens of these nurses, ‘You’re going to stop doing your outpatient preventive care and we’re moving you to the hospital to keep people from dying.’ Because we were running at 140 to 150 percent inpatient capacity, you know, not that long ago.”
“The biggest challenge that we’ve had are these peaks and valleys of COVID in the inpatient environment,” Guterman adds. “As an integrated delivery system, we had to make the tough decision of reducing preventive care and continuity care in the outpatient environment to get people to the besides of patients” during the COVID-19 disaster.
However, the team hopes to maintain and expand the project this year and in 2022. “I’m so proud of how this whole project has turned out,” said Guterman. “It has changed the dynamic of how the professional nursing staff views themselves in the outpatient environment. It has changed how patients feel about remote care, from it being considered second-class to something superior to what it used to be. And that’s not hyperbole. That’s what this has become.”
Learn more about LACDHS’s TC3 project here.
San Francisco Health Network: Improving disparities in BP control for Black/African American patients
The San Francisco Health Network (SFHN) is the healthcare arm of the San Francisco Department of Public Health, which runs two major hospitals and 45 clinics. This safety net hub serves hundreds of thousands of patients yearly, including a large percentage of patients with chronic diseases, including diabetes and hypertension.
Before the pandemic, SFHN’s ’s overall hypertension control rates were at the 90th percentile of the Medicaid benchmark. Its blood pressure control rate in primary care, including that of African-American patients, had improved from 61 percent to 70 percent overall. But after the pandemic struck, patients with hypertension had a harder time managing their blood pressure, especially Blacks and African Americans, whose blood pressure control dropped to 48 percent compared to 50% in the overall population. Misinformation about COVID-19 was also widespread (see CCI’s story “SF Health Network Reaches Out to High-Risk Patients to Protect Them From COVID-19”).
Racial equity in healthcare has recently been a strong focus for SFHN (see CCI’s article “Tackling Bias, Fear, Inequality and Disrespect”: Tosan Boyo’s Blueprint for a Successful Equity Journey in Healthcare). Its other goals included improving its A1c control rate to at or above the 90th percentile in the Medicaid benchmark for people with diabetes and to improve depression screening rates by 10 percent overall and for Black/African American patients.
Dr. Elaine Khoong, a primary care physician from @ZSFGCare, shares how phone visits are critical to expanding access to care. @SF_DPH @elainekhoong #Thankful4Telehealth pic.twitter.com/3wuUVLMY0g
— CAPH (@CAPHSystems) April 27, 2021
“Although telehealth was convenient for many patients, we found they did not have the resources they had relied upon for blood pressure control, including regular in-clinic blood pressure checks, health and wellness classes, and Food Pharmacy,” said Aimee Crisostomo, SFHN’s primary care population health quality improvement coordinator. Among other responses, the network ramped up its support in those areas, distributed blood pressure monitors to community clinics for patients to use at home and began delivering food to food-insecure patients unsure of where their next meals were coming from.
SFHN also created a Hypertension Equity Workgroup. To include patient voices, staffers interviewed a group of five Black/African American patients with hypertension to see what they needed during the pandemic. As it turns out, the patients felt they had lost communication with their clinics and particularly missed their in-person support group for hypertension. Their suggestions included mailing medications, telehealth support, nurse chronic care visits, coaching on home blood pressure monitoring (SMBP), and a remote hypertension support group.
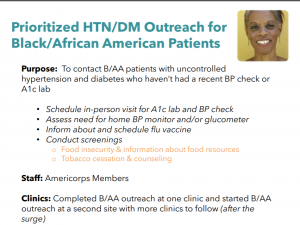
from the SF Health Network’s presentation on self-monitored blood pressure
Staff at SFHN incorporated those ideas and more, setting up in-person appointments for Black or African American patients who hadn’t had a recent blood pressure check or A1C screen and distributing blood pressure cuffs and glucometers for home use. They also screened patients for urgent social needs, such as food delivery, and set up virtual support groups and telehealth appointments. By prioritizing Black/African American patients for outreach, SFHN was able to successfully close the disparity gap in hypertension control by the end of January 2021. Its equity aim is to keep that gap closed and to achieve a 10% relative improvement rate overall and for Black/African Americans.
Read more about SFHN’s hypertension control equity work.
And learn more about all of the PHASE/TC3 teams’ exciting work here.
From the pandemic to Oz
The PHASE and TC3 program-end celebration also involved moving keynote speeches from Dr. Marc Jaffe of The Permanente Medical Group, Northern California and Dr. Timothy Ho of Southern California Permanente Medical Group, and celebratory videos, including one from CCI coach Denise Armstorff about the PHASE and TC3 teams “and the many hats” they wore throughout the COVID crisis. At the end of her reflections, which involved donning more hats than the Village People, Armstorff told participants how grateful she was to have accompanied them on this pandemic year journey “to timely, patient-centered and equitable healthcare,” which she compared to Dorothy’s journey to Oz:
“Like us, Dorothy finds herself in a place where she doesn’t want to be,” said Armstorff, who bears a suspicious resemblance to Glenda the Good Witch. “She seeks to find the Wizard of Oz, who she believes can direct her on how to accomplish her goal. She finds companions on the way and encounters many dangers and some challenges, too. Yet when they finally get there, she and her companions learn that she had the resources to go home all along, hidden in the ruby red slippers she was wearing the entire time.”
Remembering that the resources to improve lie within us is something to keep in mind as life slowly starts to return to normal – or a “new normal.” Safety net clinics, including those who have been part of PHASE, have to decide what comes next. In former PHASE clinics, many are discussing the right mix of in-person and virtual services to offer their patients. All are seeking to expand their population health work, especially efforts to empower patients by involving them in self-monitored blood pressure programs – and seeking leadership buy-in to continue.
Riding the wave
Although the program has run its course, its mission to improve cardiovascular care is as important as ever. Kaiser Permanente has again partnered with CCI to kick off the Virtual Care Innovation Network, which will offer resources that will support the work of PHASE participants in the wake of the pandemic.
Dr. Ho, regional assistant medical director for quality and complete care at Kaiser Permanente in Southern California, traced the different waves of the pandemic that washed over clinicians – with the first being the pivot to virtual care and all things COVID-19, the second wave being the impact of non-COVID 19 conditions such as heart health, cancer, and all the acute ills whose treatment was perhaps delayed because of the pandemic; the third wave being the impact of interrupted care and chronic conditions; and the forth wave is marked by “deaths of despair” – all the deaths from suicide and substance use and the deadly fallout from job loss, burnout and economic dislocation caused by COVID-19.
“As we really start to ramp up our vaccine work, it’s going to be very difficult to do population health and care gap closure and vaccine appointments,” Ho said.
“But I think there is actually an opportunity to use the vaccine work to bolster or to reinforce population work, especially chronic disease and cardiovascular care,” he continued. One of the important things that came out of the pandemic, Ho said, was gathering timely data “and actually using it” to improve care. Another was being forced, by the glaring disparities of the pandemic, to pay closer attention to social needs. Clinics and hospitals have also ramped up outreach, “which used to be an afterthought,” he added. “So the vaccine appointment is an opportunity to at least get patients re-engaged – maybe with just a blood pressure check – to re-engage and start riding the waves instead of getting hit by them.”
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.

