Project Activities
Project Activities
Phase 1: Learning from the PRAPARE pilot
At the start of the ROOTS program year, more than 400 PRAPARE screens had been collected through the previous PREPARE pilot by four care teams: patient navigators in a primary care clinic, the HIV intervention care team, behavioral health case managers, and the Care Neighborhood community health workers. Based on interviews with 30 patients screened during the past pilot, the AHS team learned that most patients were comfortable with the screening and had high trust in AHS, especially with the behavioral health team. However, rates of success with assistance and types of assistance offered differed by care team: 80 to 90 percent of patients screened by the behavioral health team had been linked with services, compared to fewer than 25 percent of patients screened in primary care.
“What this project has uncovered— just through the screening and the response— is that we may already have some of these answers, we just need to share them.”
– AHS Chief Deputy of Administration, Programs
The AHS team believe these differences in part reflected how available staff were to work with patients on social service connections, but also differences in teams’ knowledge about available resources. For instance, because of the high housing needs among HIV-positive patients, the HIV team was very familiar with housing resources and had access to a monthly housing availability list that other teams were unaware of. And one behavioral health case manager had found a way to get patients into hotels when they needed temporary housing, something that others did not know was possible.
To share this information and ensure all patients benefit from this knowledge, staff from different implementation teams started talking to each other more routinely to identify and exchange resources. For example, the HIV program manager and care staff now attend the monthly behavioral health case management meeting.
In addition to ensuring that knowledge about resources were being shared internally, the team assessed the appropriateness of referrals for their patient population. They examined geographic proximity, eligibility requirements, and language access, knowing these factors would be of high relevance to their patient population. They also contacted community-based organizations directly to better understand how patients might experience the resources they were offering. They then developed a list of vetted resources that now forms the basis of all referrals for the entire staff.
“Even if it’s five miles away rather than two miles away, but we know that they have Cantonese, I would prefer they have to go the five miles, because at least they can get help.”
-AHS Community Services Manager
Phase 2: Developing a More Effective and Coordinated Screening and Referral Workflow
Incorporating the PRAPARE screening into established clinical workflows brought unique challenges to both patient navigators and case managers. Initially, navigators reported that some patients were surprised by the personal nature of the screening questions or became emotional during screening, as they shared their stories of hardship. Increased screening also meant behavioral health case managers were suddenly busier — they needed more time with their own patients and were receiving more referrals from patient navigators. Additionally, case managers working with HIV-positive patients were frustrated by the overlap between some of the PRAPARE screening questions and other grant-mandated surveys, worrying about patient “survey fatigue.”
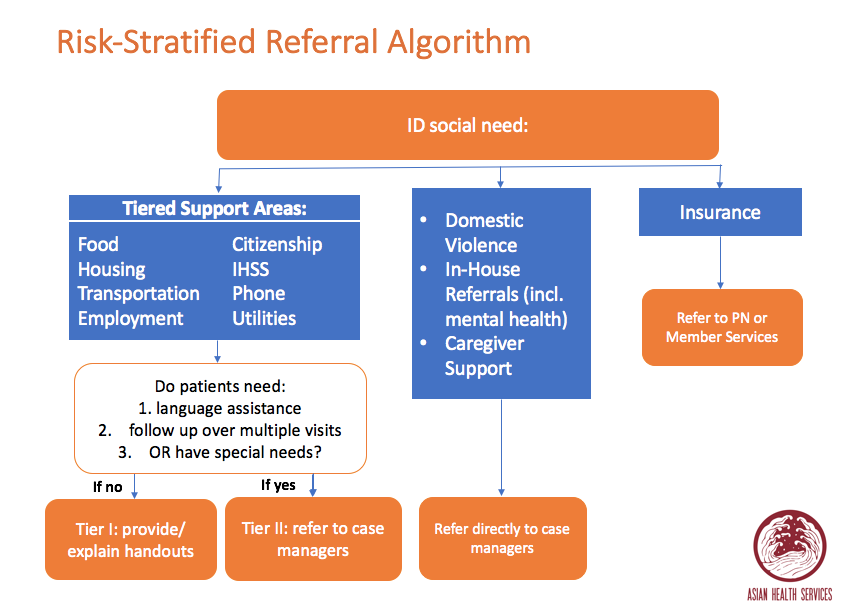
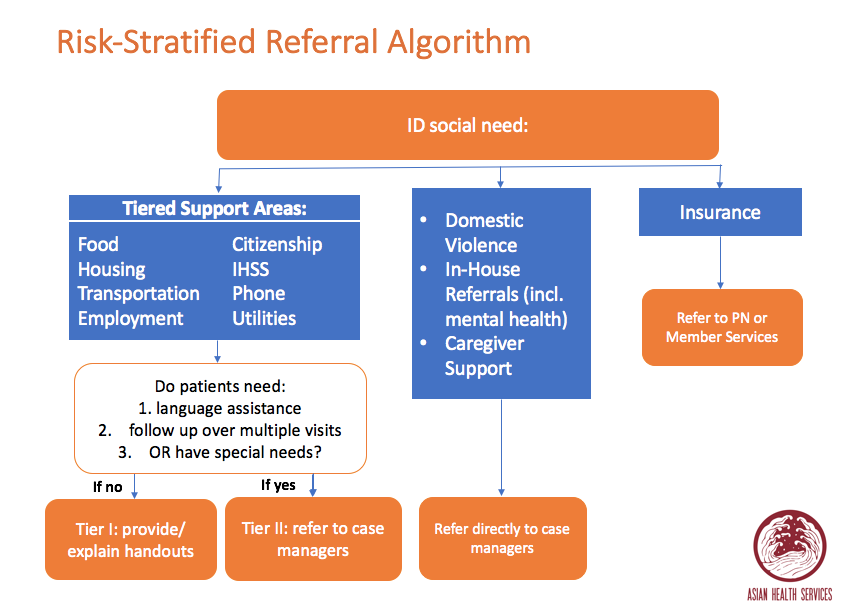
To respond to these challenges, the ROOTS project team worked with the teams implementing PRAPARE to develop a risk-stratified referral algorithm based on complexity and required level of support. Depending on specific criteria, patient navigators were trained to address more straightforward needs and to refer patients with more complex needs to either case managers or member services.
Patient navigators also met frequently with their supervisors to review how to ask PRAPARE screening questions efficiently and compassionately. To address concerns about duplicate screening questions, the team decided that only non-duplicative screening questions would be asked.