LifeLong selected this tool because it was short and research has shown it has high sensitivity and specificity for identifying households at risk for food insecurity. In addition, when the team piloted the tool in a wellness center food and nutrition course, participants completed the screening questions without difficulty and were open to talking about the food issues they faced. The HVS screening questions were built into the health system’s electronic health record (EHR), NextGen, along with a third question asking patients if they wanted to talk with clinic staff about their food needs.
Desire for Assistance
“If LifeLong were to offer support, assistance, or resources to access nutritious and healthy food, would you be interested?” (yes/no)
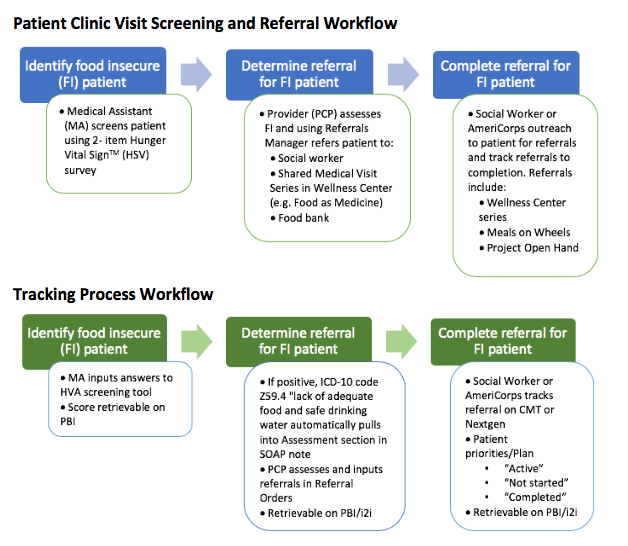
Building Manageable Workflows
In the selected primary care clinic, provider and medical assistant (MA) teams work in pairs and typically see between 10 to 15 patients in a four-hour window. Working with a provider and MA team, the ROOTS project team developed a workflow to integrate food insecurity screening and follow-up referrals into a clinic visit.
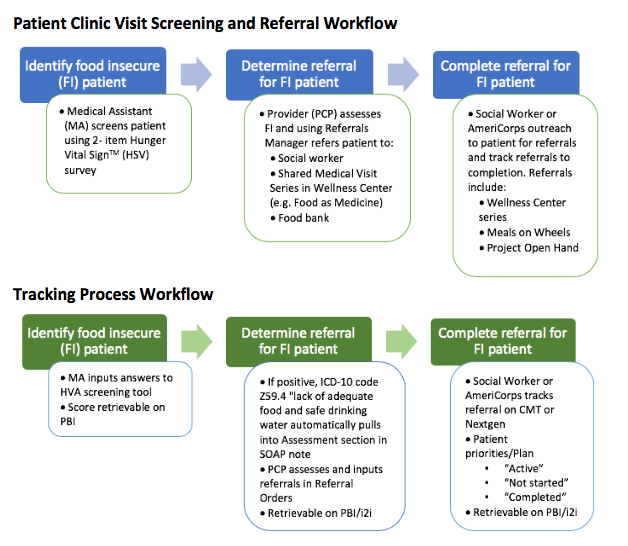
Patients either completed the screen on paper or the MA asked the questions and entered answers into the EHR during a face to face encounter with the patient. Providers reviewed the paper or EHR-based results with patients; if they identified food insecurity and patients were interested in assistance, providers made referrals to food access programs and/or the clinic social worker. The care team documented screening results and referrals using the EHR case management template, where the referral was tracked by the clinic social worker. Over time, AmeriCorps volunteers also helped track referral outcomes.
Stratifying Risk of Food Insecurity
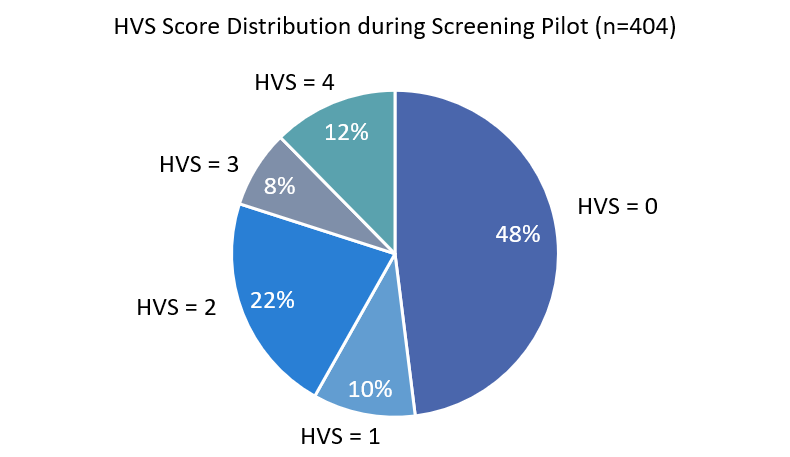
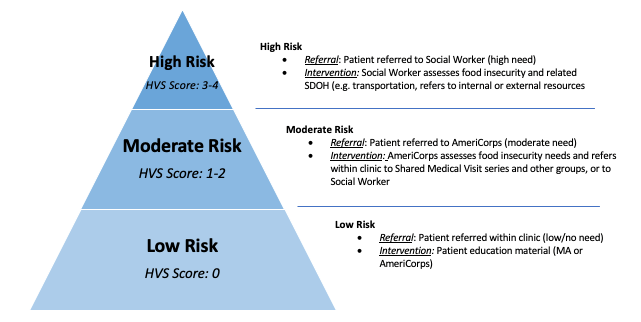
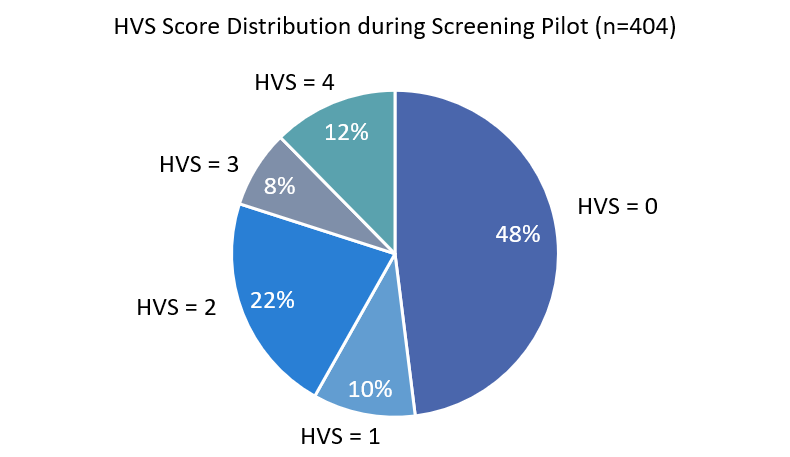
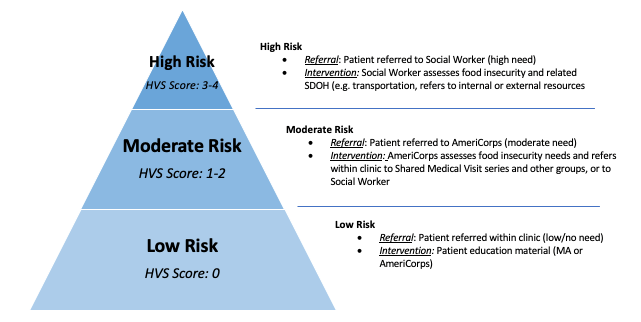
To manage referrals efficiently, the ROOTS team identified three levels of risk based on the HVS score:
- Low risk (HVS score = 0)
- Moderate risk (HVS score = 1-2)
- High risk (HVS score = 3-4)
All high- and moderate-risk patients were referred to the clinic-based social worker who would call patients to assess the acuity of food needs (e.g., did they have food to eat today?) and follow-up to ensure help was provided. Nearly half of the 404 patients screened during the ROOTS program year were low risk, a third were moderate risk, and a fifth high risk.
Challenges to Developing a Successful Food Insecurity Screening and Referral Program
The ROOTS project team faced several challenges once they started implementing the pilot:
- They had to replace the initial pilot provider/MA care team when the first provider left for maternity leave.
- The provider/MA team was unable to consistently find time to ask about or address food insecurity during medical visits.
- The number of patients referred for follow up to the sole social worker exceeded her capacity.
- Some patients who were considered high risk based on the HSV scoring algorithm did not report food insecurity when the social worker followed up.
To overcome these challenges, the provider/MA care team experimented with different screening approaches to find the most efficient method. The team also reduced the burden on the social worker by connecting patients to referrals themselves or providing “warm hand-offs” directly to the social worker, which helped minimize the need for initial phone calls or visits. The ROOTS project team also decided to limit the number of unanswered calls the social worker made to each referred patient before closing the case.
Project Turning Point
A turning point for the project occurred when the team realized the wellness center’s AmeriCorps volunteers could help both screen patients and connect them with resources. The volunteers, who were responsible for running the wellness center’s weekly veggie giveaway, began conducting food insecurity screening during the giveaway. Volunteers were also tasked with following up with patients at moderate food insecurity risk, thereby reducing the social worker’s workload.
Expanding the Veggie Giveaway
For the past ten years, the health center has been holding a weekly veggie giveaway with unsold fruits and vegetables from local farmers markets. Often this produce was of poor quality and visually unappealing, and the event only attracted about 20 to 30 patients each week. The ROOTS team took advantage of the ROOTS project to improve LifeLong’s nutrition resources, reaching out to several food-related organizations to explore partnership opportunities. After several dead-ends, they heard that another ROOTS cohort member in the same county, Asian Health Services, has made inroads with the Alameda County Community Food Bank. A persistent AmeriCorps volunteer assigned to reach out to the food bank managed to establish contact with the organization and eventually set up a process to expand the veggie distribution.
AmeriCorps volunteers now travel weekly to the food bank to pick up fresh fruit and vegetables — as well as supplies such as blankets, deodorants, tooth brushes, and socks — which they then offer for free in an expanded location outside the clinic. By partnering with the food bank, the LifeLong team:
- Improved the variety, quality, and amount of produce they offer;
- Increased the number of people accessing the veggie giveaway from to around 100 patients each week;
- Added a mini-giveaway after wellness center classes;
- Created food bags that the social worker and community health workers deliver to patients during home visits; and
- Supplemented groceries for clinic staff.