When the Community Health Centers of the Central Coast (CHCCC) teamed up with the local nonprofit Fighting Back – Santa Maria Valley, its providers expected to focus on intervention and preventive mental health services for teens – in particular, those experiencing adverse childhood experiences (ACES) and domestic or intimate partner violence. Then the pandemic hit. It quickly became apparent that the new alliance formed by the two organizations, known as the Peace Network, would need to switch to crisis management mode.
This was crucial to help preserve youths’ physical, psychological, emotional, and spiritual health during an unprecedented time. With so many teens suffering from isolation, disruption, loneliness, and grief, the Peace Network – short for Positive, Equitable and Affirming Childhood Experiences – would focus on expanding mental health services in the high schools. With a pandemic-related uptick in anxiety, depression, substance use, and ER visits linked to domestic violence, along with lockdowns, remote learning, and job loss, the partnership had to pivot fast.
Rather than seeing COVID-19 as an insurmountable obstacle, this coastal California partnership viewed it as a situation that accelerated the pace of innovation. To better meet the needs of the community, says Magdalena Sunshine Serrano, director of CHCCC’s behavioral health department, “we had to go beyond brick and mortar to ‘click and mortar.’”
 Serrano says partnering with Fighting Back was a natural fit. There was already an informal relationship established with the organization, which had long had “eyes, hands, and hearts” in the school district. The advocacy group, which has spent years developing school relationships, served as a bridge for the clinic-centric safety net provider. Fighting Back also has the capacity to go into students’ homes, serving as a crucial lens into their domestic situation. “That’s huge,” says Serrano. “Seeing an adolescent in their home and getting a handle on the family system — and what kinds of resources, support, and interventions might be needed — made this partnership particularly powerful and really helped us to amplify our reach beyond the clinic setting.”
Serrano says partnering with Fighting Back was a natural fit. There was already an informal relationship established with the organization, which had long had “eyes, hands, and hearts” in the school district. The advocacy group, which has spent years developing school relationships, served as a bridge for the clinic-centric safety net provider. Fighting Back also has the capacity to go into students’ homes, serving as a crucial lens into their domestic situation. “That’s huge,” says Serrano. “Seeing an adolescent in their home and getting a handle on the family system — and what kinds of resources, support, and interventions might be needed — made this partnership particularly powerful and really helped us to amplify our reach beyond the clinic setting.”
Peace Network is part of Amplify Healing Connections, a CCI program supported by the Blue Shield of California Foundation. It was created to help youth at risk of domestic violence, which includes the risk of violent or aggressive behavior within the home, often including verbal abuse, threats, and physical assault. It typically involves the abuse of a spouse or partner. In the United States, nearly 30 million children under 17 have witnessed such violence in the home. Left unaddressed, this can undermine their future intimate partner relationships, education, and health outcomes.
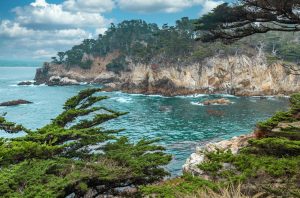
CHCCC is a safety net provider with more than 30 clinics that serve around 150,000 individual patients (with 450,000 medical visits annually) in a picturesque coastal community. The center provides culturally and linguistically sensitive healthcare to the working poor, migrant and seasonal farmworkers, individuals and families experiencing homelessness, students, and the uninsured. It also reaches rural, remote, and Indigenous residents. Fighting Back offer parenting classes and direct services to youth to develop resiliency and positive experiences in the face of problems such as substance use, truancy, and violence.
Offering timely mental health services via teleheath
As with all health clinics, CHCCC quickly shifted to virtual care not long after the pandemic emerged. That included reaching its adolescent patients remotely, too. Fighting Back referred students to clinic counselors, who also receive referrals from pediatricians.
During the peak of the pandemic, the demand for mental health treatment for youth proved enormous, even overwhelming at times. The center saw a 300% jump in referrals, according to Serrano. Their switch to a digital delivery of services—telehealth and telephone appointments and referrals—proved more effective and efficient than clinic visits, she says. It also eliminated barriers for adolescent participation, such as transportation and distance, and gave teens the ability to access culturally relevant and language accessible counseling that may have been out of reach prior to the pandemic.
And, as Serrano notes, most adolescents – unlike some older folks — are comfortable and confident navigating online platforms. There was an additional bonus to providing telehealth services to this population: It gave adolescents more autonomy and independence over managing their own healthcare. And they proved up for the task. No-show rates dropped from 20% to 12%, according to Serrano, and the level of consistent engagement in therapy jumped; on average, adolescents attended 12 counseling sessions.
Serrano, currently a fellow with the California Health Care Foundation Health Care Leadership Program, sees the benefit of combining telehealth and behavioral (aka mental health) services reflected both in data and anecdotal evidence. In the leadership program, Serrano is focusing on the state-wide development of a telehealth-based behavioral health model. From her perspective, digital equity and health equity are intertwined, and the pandemic only magnified that reality. Starting early on in the COVID-19 outbreak, the clinic went the extra mile to ensure that patients with less access to tech—in particular vulnerable Indigenous and Latinx clients—got the assistance they needed for healthcare, vaccine clinics, and mental health counseling. That outreach included cold calling current and former patients, texting clients, and handing out resources about behavioral health services to residents waiting in line for vaccine shots.
Healing the healers
Serrano was also proactive in dealing with staff stress due to the volume and emotionally intense demand for their services. The organization worked with Beverly Kyer, a consultant/coach who specializes in tackling compassion fatigue and professional burnout in caregiving and support services organizations. Kyer shared multiple strategies for recovery from burnout, techniques for reducing and preventing the negative effects of compassion fatigue, and methods to restore peace, calm, and self-regulation when confronted by chronic stress.
As an organization, the clinic also made a commitment to expand its counseling services to meet the needs of its community. The health center has added seven more therapists to its team, taking counseling staff to an even 20, says Serrano. During the hiring process Serrano says that the behavioral health team understood it was vital to add clinicians who reflected the demographic of the adolescent population it serves. In this case, it meant intentionally adding young, male, and LGBTQ counselors into the mix.
LGBTQ students have been particularly vulnerable during the pandemic, when in-person support systems in the school and greater community were more difficult to access or unavailable, notes Serrano. That’s particularly tough for LGBTQ students who don’t have support at home, she adds. It’s also crucial because LGBTQ youth experience mental health challenges and suicidality at higher rates than their heterosexual peers. Transgender youth are two times more likely than their cisgender peers to experience depression, consider suicide, or attempt suicide. Approximately 17% of youth (ages 6-17 years) live with a mental health disorder. Half of all mental health illnesses begins by age 14, with 75% of such illnesses emerging by age 24.
Even before the pandemic arrived, national surveys of youth have shown alarming increases in the prevalence of certain mental health challenges. In 2019, one in three high school students and half of female students reported persistent feelings of sadness or hopelessness, an overall increase of 40% from 2009, according to the Centers for Disease Control and Prevention. As U.S. Surgeon General Vivek Murthy has noted, the pandemic further exposed the country’s youth mental health crisis and the devastating impacts COVID-19 has had on adolescents.
Health centers like CHCCC see evidence of that crisis in their clinics on a daily basis. Partnering with other like-minded organizations in the area can be crucial to ensuring that youth get the behavioral healthcare services they need in a timely fashion. “The whole partnership process has taught me that it’s not enough to be of the community, you need to be in the community,” says Serrano. “It’s helped me have a better understanding of the issues beyond healthcare, and helped me understand different systems—such as schools, which are vital partners as they give us access to the most vulnerable adolescents.” That includes students who may be witnessing domestic violence in their homes, at risk for intimate partner violence themselves, or screen positive for mental health concerns.
For Serrano and her counseling team, there is no turning back. “This program is here to stay. We have created an intentional and inclusive framework with partnerships that help create pathways for us to care for the community — in this case, the physical, psychological, emotional, mental, and spiritual health of our adolescent youth. We are meeting the moment and the movement of what it really means to be a community healthcare center.” But Serrano, who was named Trauma Resource Institute ambassador of 2021, knows there is more to do. “Now we have to start looking at the entire family system and how we can support our community doing the upstream work of early intervention and prevention… so we can move the needle here on these cycles of intergenerational trauma.”
Lessons learned
Take the time to build trust with partners
It’s critical to make sure that values and mission align and that there is a deep level of trust, says Serrano, particularly on the tough days when things don’t go according to plan. Understanding your partner’s “why” can go a long way to helping navigate challenging times, she says, especially in intense areas such as intimate partner violence, domestic violence, ACES, and family trauma.
Schedule site visits
Get a sense of the physical space and staffing each organization has to work with—whether it’s a health clinic, school, or nonprofit. The pandemic made that tricky to accomplish but it helps to understand the benefits and limitations partners face at their locations.
Consider all stakeholders
For the Peace Network, bringing a third partner into the mix—a family crisis center or domestic violence shelter —would help address a larger, systemic issue around intergenerational family violence. Such an addition formally acknowledges that this healing work involves the whole family, not just adolescents, says Serrano. Particularly in a rural community, locating physically safe spaces for individuals and families to stay is crucial.
Ensure diversity among the counseling team
CHCCC realized that its counseling staff didn’t have enough male representation, lacked members who identify as part of the LGBTQ community, and tended to skew older. New hires were intentionally recruited and selected to correct that imbalance. Youth want to see people they can relate to and feel comfortable connecting with on mental health matters.
Build in time and resources to educate the community
There was a learning curve for the school district, in terms of interacting with the healthcare system, notes Serrano. Look for ways to efficiently and consistently keep all members of a community effort updated and in the loop. Information should not just live with one or two key players. Fluctuations in personnel can make that challenging, so communication is key.
Develop a community advisory board
Peer-to-peer input is invaluable; youth learn from other young adults and survivors on their own healing journey. Create and co-design a space for youth leaders who can offer feedback relevant to adolescents, including everything from the power of language to the need for more inclusive outreach materials.
Amplify Healing Connections seeks to strengthen interventions designed to prevent domestic violence and promote health and well-being for adolescent youth and their adult allies. Launched in March 2021, the 22-month program, with funding from the Blue Shield of California Foundation, is a collaboration with six California-based, multi-sector partnerships, each involving at least one community-based organization and one health care provider serving youth 12-18 years old. Youth-service organizations play a pivotal role in promoting healthy communication and providing a strong, nourishing environment for young people and their caregivers. Coordinated efforts across community organizations can amplify (PCEs) and help prevent, reduce, and even reverse the impact of early adversity.
In this Amplify series:
Amplify Healing Partnership Hosts Courageous Conversations Conference for Teens
10 Ways to Create Effective Community Partnerships
“Give the Kids a Voice”: Working on Resilience with Teens and Families at Risk
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.


