Testing a Mobile Scribe Solution
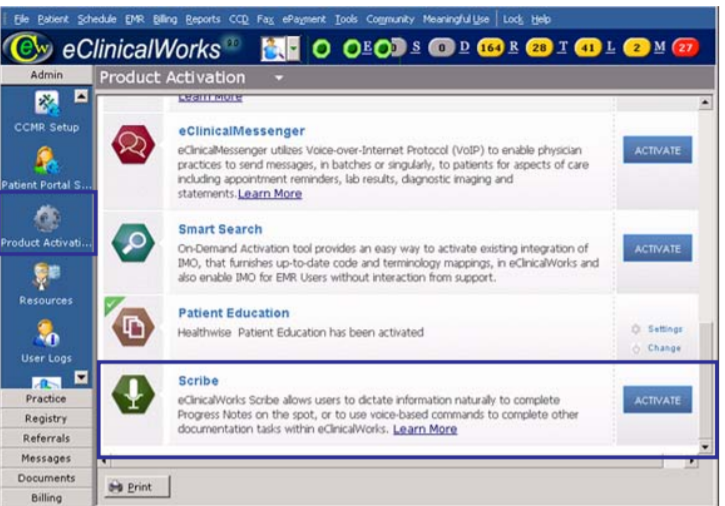
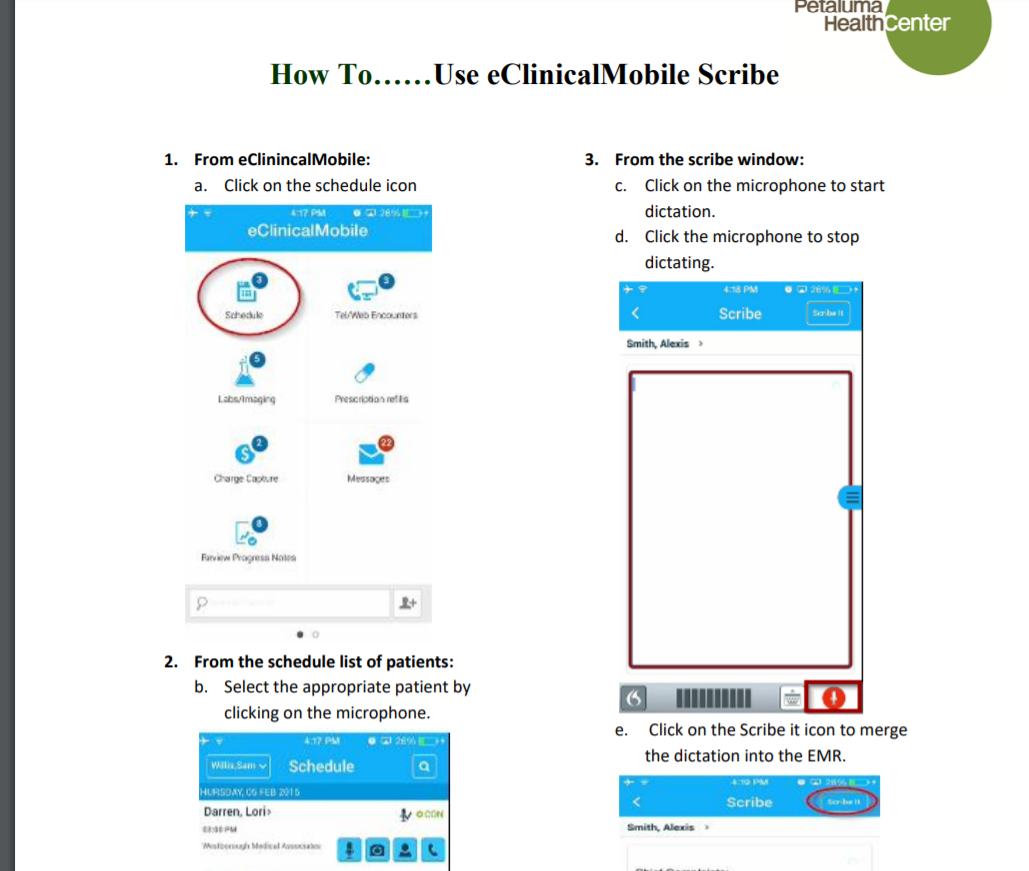
Oryn and Moore hoped to get some of the benefits of a real-life scribe by exploring some of the newer technology solutions for note-taking and dictation. They didn’t have to look far: The vendor for their electronic health record (EHR) was eClinicalWorks, the largest cloud-based healthcare IT company in the country. And among the software it offered clients was Scribe, a mobile speech recognition app.
eClinicalWorks was founded with a simple proposition in mind: “Rid doctors’ offices of paper and make every connection providers need — to pharmacies, labs, and supply chains.” The mission was to improve communication and workflows by digitizing them. Over time the company expanded its goals to include cloud-based solutions for controlling costs, reducing errors, deepening analytics and improving the quality of care. Scribe, with which doctors and nurse practitioners (NPs) could dictate their notes, seemed like an ideal test case for Petaluma.
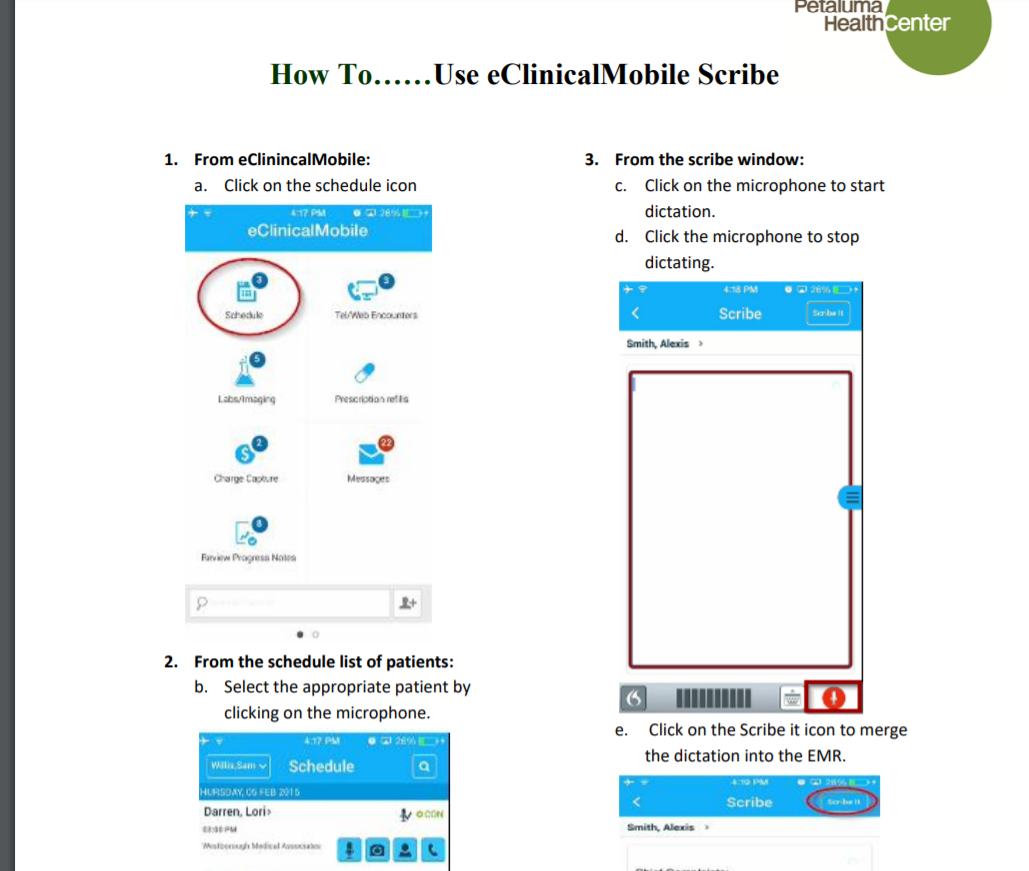
In March 2019, the eClinicalWorks’ Scribe was among the apps featured at PHC’s annual Tech-a-Palooza, which the clinic put together to show and coming technologies. “People got to test out and play with it, and we showed the app to the provider team to great enthusiasm.” recalled Oryn. In addition, the app was already available on their Petaluma Health Clinic mobile phones, which linked to the clinic’s eClinicalWorks EHR. (The team didn’t consider a desktop app because it had different requirements, so the providers do all their dictation on their PHC cell phones.)
“We had thought about using an app or real scribes in the past but hadn’t tried it except with the exception of our specialty providers,” she added. “In their case we used human scribes, which worked because they only came about once a month. But in the case of our other providers, that would have been cost-prohibitive.”
Moore noted that integration with the electronic health record was a big advantage
“When we started looking at the apps available, their mobile app seemed to be a good place to start since it is seamlessly integrated into our EHR,” Moore said. The leadership team arranged to license it for a trial involving 10 providers, which grew to 14 ranging from primary care to behavioral health.”
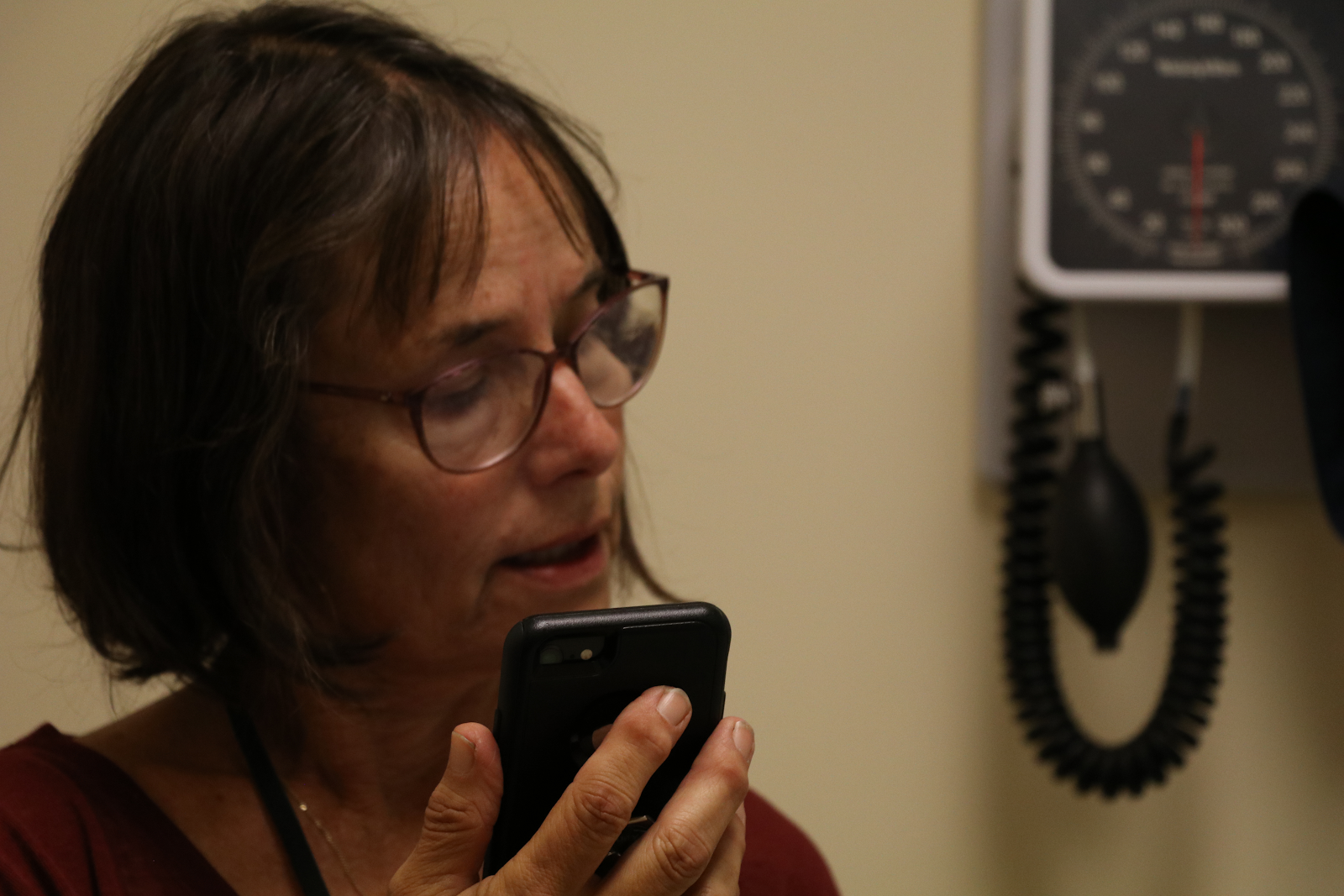
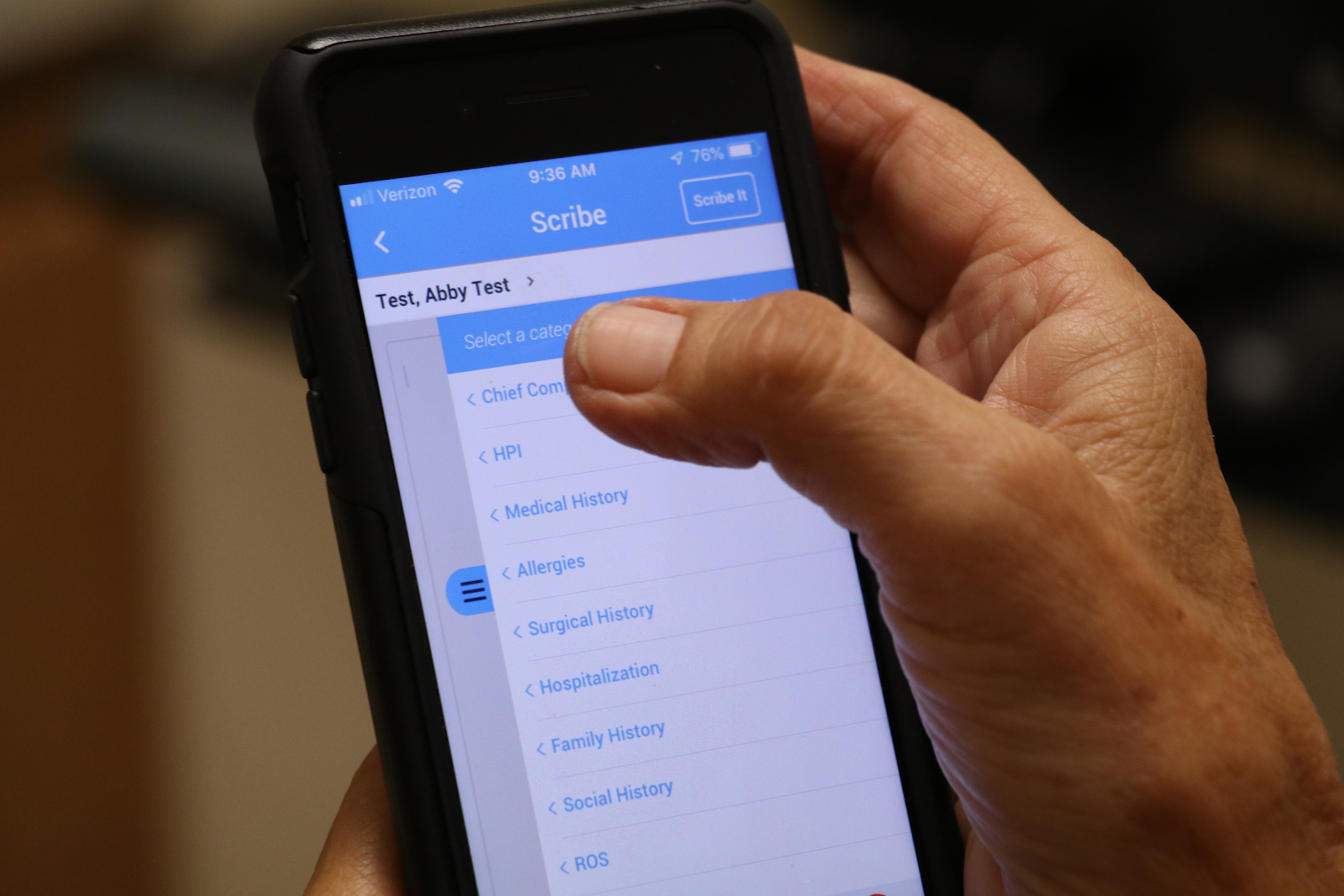
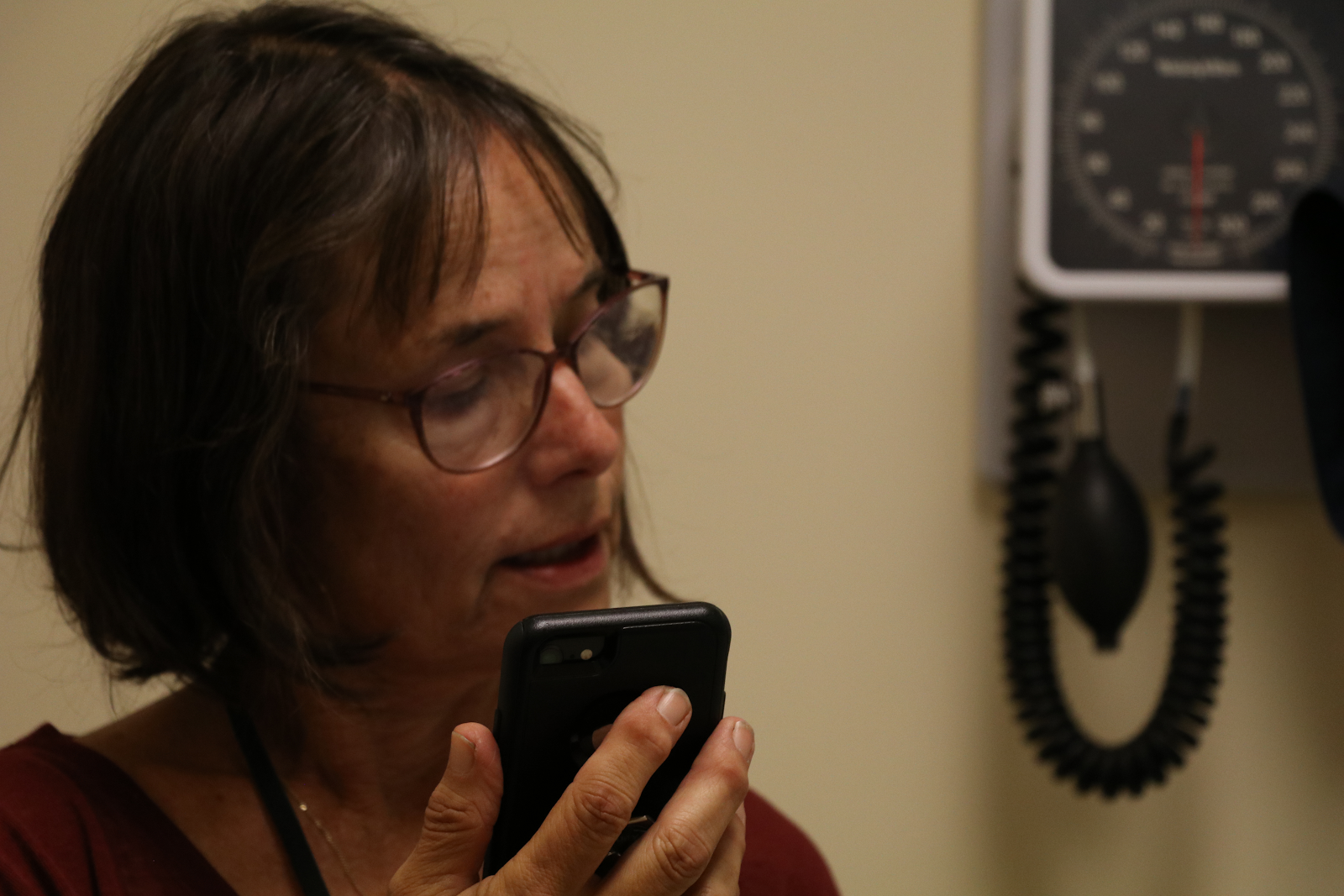
Annie Nichol, NP, gives her wrists a rest by dictating patient notes into the Scribe app on her PHC phone.
Metrics
The metrics the team developed were intuitive: They focused on determining whether eClinicalWorks’ Scribe made it easier and more efficient for providers with pain or physical limitations to assemble their patient notes. Another explored the tool’s impact on the patient/provider encounter.
Metric 1: Self-reported efficiency of providers
Metric 2: Provider satisfaction with the tool
Metric 3: Ease of use for providers
Metric 4: Provider-reported impact on patient/provider encounter
How Scribe Works
If the work of real-life scribes was once copying texts and manuscripts for kings and queens, temples and cities, the Scribe app’s work for doctors is often equally complex (but without the danger of being beheaded if the tool makes a mistake).
For physicians, the tool lets them either type or dictate information to complete Progress Notes and to use voice commands to complete many documentation tasks. The dictation app works well to record speech, according to Oryn, and some providers have noted that a strong accent is no impediment. However, Oryn notes that it’s important for providers to edit what they dictate: “Sometimes you have to clean things up.” Here are the basic instructions and types of commands:
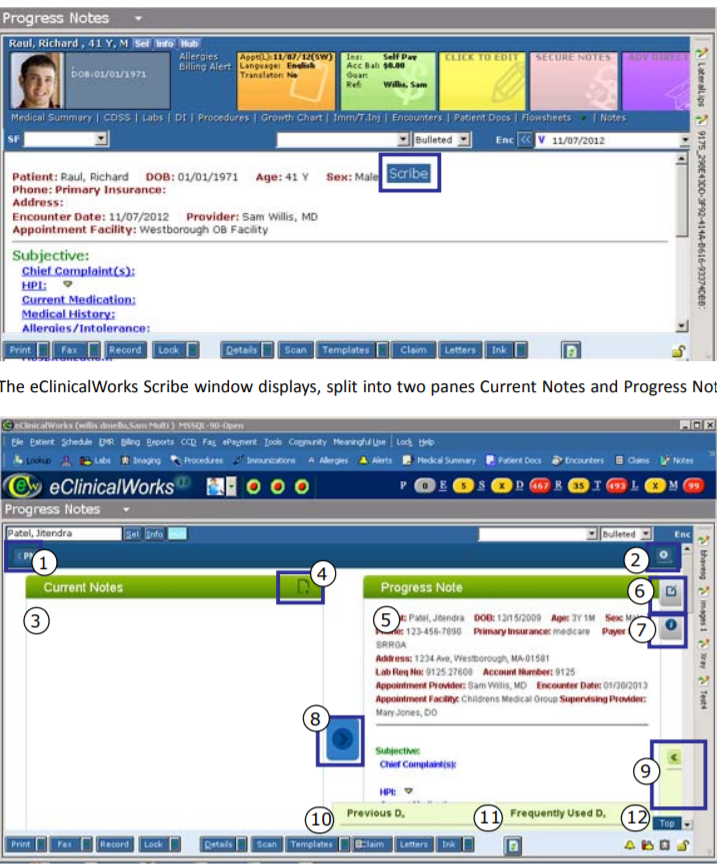
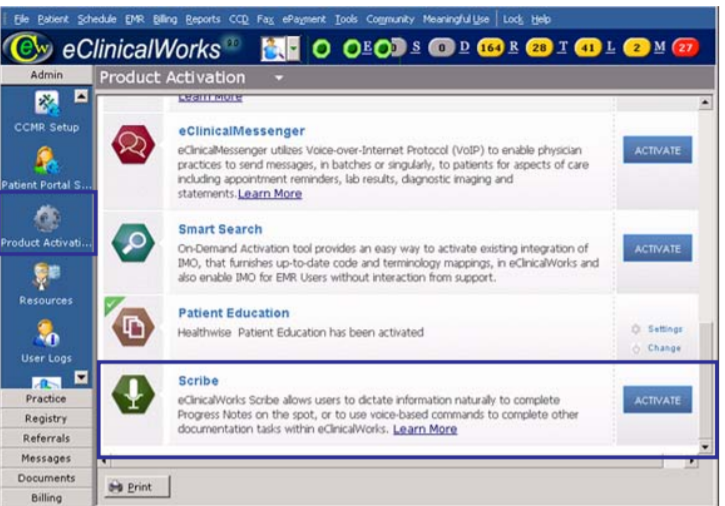
1. After scrolling to the Scribe button within the eClinicalWorks platform — possibly by having an administrator activate it — a provider can register. There will trigger a small monthly charge per physician or NP.
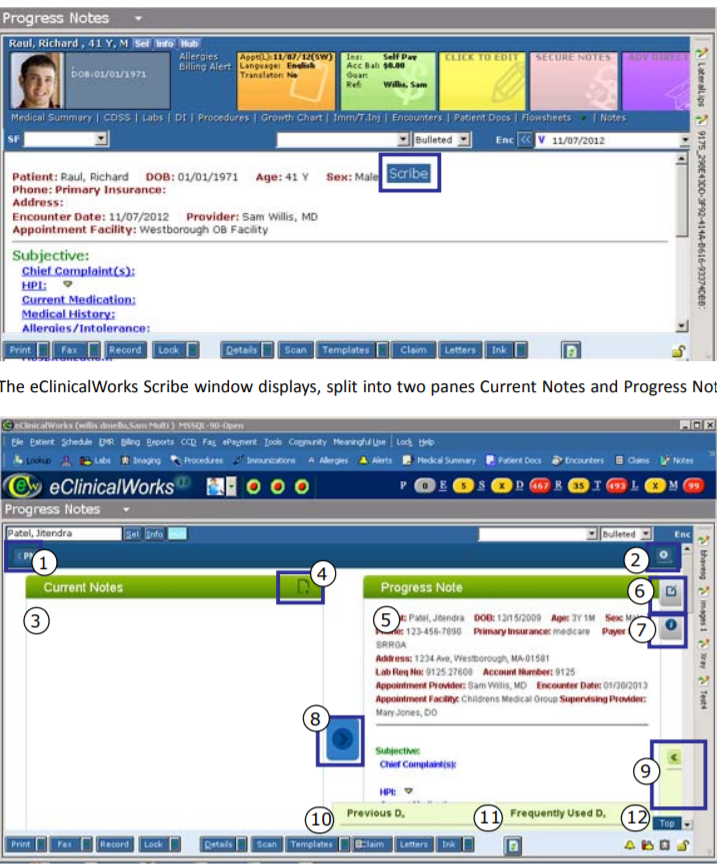
2. The provider then navigates to the patient’s Progress page within eClinicalWorks. This will contain a list of items that includes Chief Complaint, HPI (History of Present Illness), Current Medication, Medical Histories, and Allergies, among other things. He or she can tap on any of these headings to read further.
3. The pane will split into two functions: Current Notes and Progress Notes.
4. The provider can now type, dictate, or import information from HPI and other categories into Current Notes as needed. He or she can click for Suggestions on Assessments, Rx, Order Sets, and so on.
5. Touching the Help button will bring up a list of commands, such as “Import all history” and “Import Allergy, Medical History, and Hospitalization.”
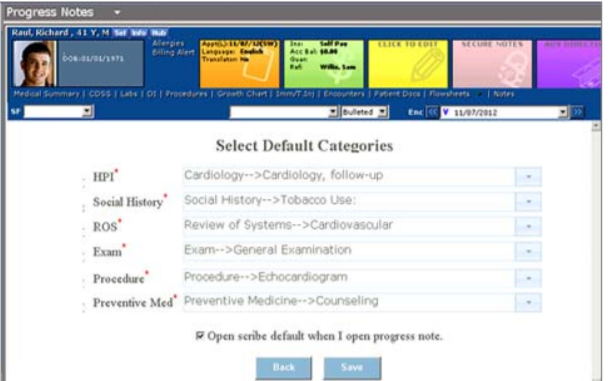
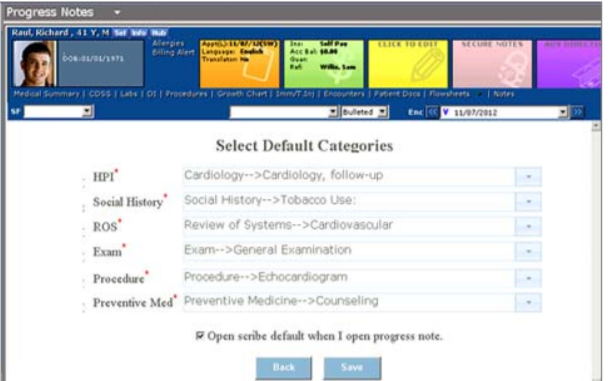
6. For Progress Notes, select the default category the text should appear in.
7. To combine your Current Notes with the Progress Notes, press the blue Synchronize button. (Current Notes are the medical notes from the most recent visit; Progress Notes are records meant to be shared with other healthcare workers involved in a patient’s treatment plan; otherwise, the healthcare workers would have to start over from scratch at each visit. Progress Notes keep staff up to date on patient care and include treatment plans, medical history and other crucial information.)
(For readers interested in learning more about how Scribe works or how doctors react to it, a series of YouTube videos about EClinicalWorks’ Scribe describe step-by-step functionality and serve as instructional guides.)
Challenges and Obstacles
The team planned to look at whether or not the tool improved provider experience and satisfaction with documentation. However, several problems cropped up.
“We had difficulty scheduling providers for training, so our implementation was delayed,” said Moore. “We were also not able to collect back-end user data to see how much pilot providers were actually using the app so as to better target re-training and better evaluate the ROI [return on investment]. Because of the initial delays with training, we spent more money than expected because we licensed the product before we had everyone trained — and it’s a per-use model.”
In other words, some Scribes were collecting a fee but not taking notes — at least in the beginning.
After the training, some staffers were less enthusiastic than others. In addition, most confined their digital note-taking largely to the History of Present Illness — a disappointment for leadership.
“Reviews were mixed: It clearly wasn’t a panacea for documentation frustration,” Moore recalled. “It required more effort to on the provider end to become fluent at using than they expected or we had hoped. It was most beneficial for behavioral health providers who often have a lengthy and detailed HPI to document, but their documentation in other areas of the progress note is minimal. Even our medicine providers reported using mobile scribe primarily for documenting the HPI, but found it clunky for documenting an entire note.”
Because of the initial delays with training, the clinic spent more money than expected, according to Oryn. However, the tool was a big win for those whose injuries or physical limitations made writing difficult or painful.
“Training was really good but I needed a follow-up. It would help me in my work but I need to brush up on how to use it more effectively,” said Carol Oppenheimer, a licensed clinical social worker at the clinic.”I’lI think this is a great idea and am hopeful that, when I am retrained I will use it to reduce strain on my wrist. I don’t think it will reduce the time it takes to chart, but that is secondary to me.”
Another employee, clinical psychologist Rosemary Healy, was also gratified to be able to dictate her notes rather than write them. “I found the app really helpful both for my finger joints — less typing — and for saving me time on my intake notes,” she said.