Petaluma Health Center is a beautiful place showcasing the technology, open workspaces, and design that I would expect to see at a Silicon Valley start-up (minus the scrubs).
- The welcoming facility draws patients in and makes it hard to get lost.
- Multidisciplinary care teams sit together in collaborative spaces with big-screen TVs.
- Staff wear Vocera instant communication devices to solve problems and meet patient needs in real time.
- The relevant health care intelligence software shows top-level performance with patient and provider drill-downs.
- Patients check-in at touch screen kiosks.
How can I achieve Petaluma’s results if I don’t have these dazzling things?




Ten seconds into the starter co-presentation by CEO Kathie Powell and CMO Nurit Licht, our Population Health Learning Network could see that Petaluma’s real secret is their culture, not their things.
Here are five ways Petaluma’s culture drives excellence:
1. Define Success
Kathie and Nurit communicated shared and specific performance objectives balanced between patient health and employee wellness (physical, behavioral, psychological). They shared speaking roles as if they were the same person. That ability to work in sync is probably why staff feel that their leaders know what they are doing, trust each other (a key organizational value), and are keeping Petaluma focused on what matters for patients.
At the same time, every staff person can access the key organizational goals, current status, and a drill down for action today for the patients on our schedule in the relevant health information system. Goal measurements are not for leaders to hold people accountable, but fuel for care teams to work collaboratively to close care gaps and make the care system better on every shift.
I understood early in the day why employee wellness was a top-level goal and not an add-on. If success depends on the power of staff to innovate and solve problems, Petaluma needs a healthy workforce with zero psychological and cultural barriers.
2. Have Fun
Every shift (morning, afternoon, and evening) starts with a mandatory all team huddle. Every huddle starts with Huddle TV, a couple minute video that staff members watch together on big screen in each of the six team areas. These messages are a key part of setting a cultural tone that matches to the rhythm of daily work. The playful tone of Huddle TV causes smiles (good for wellness!); but, more importantly, it flattens hierarchy to create staff empowerment and ownership, a key part of Petaluma’s innovation and improvement culture.
While Petaluma also has financial incentives for high performance by clinical and non-clinical staff, it’s most successful motivator is recognition celebrations. And the number one most popular recognition for staff is a shout out on Huddle TV. To learn why, Petaluma leaders recommended we read Punished by Rewards.
3. Try, Try, and Try Again
Petaluma’s stories are full of evolution, failure, and change. Kathie and Nurit described how they encourage staff to “just try something and not be tied to it.” They stress, “If the data shows it didn’t work, move on.”
These words matter, but their action speaks louder. For instance, they told us a story about a beautifully designed program they started to engage kids in exercising. They thought it hit all of the key factors likely to both engage children and reduce BMI. However, their results showed that BMI didn’t change. They abandoned it and moved on.
At the start of the visit, our Population Health Learning Network participants said they wanted to learn a variety of specifics about the population care staff roles, structure, and processes at Petaluma. Although we did learn and see this, Director of Innovations Jessica Moore repeatedly emphasized that what we were seeing was in flux and likely to change. In fact, it might have already changed in some of the teams.
Quality Improvement Director Tiffany Jimenez told us about a focused plan for achieving substantial improvements in six key projects with multi-disciplinary teams using strong performance improvement methods. It was common to discover that one of the care teams had rapidly improving on a measure outside of the organized QI project. As a result, Tiffany’s team would go learn about that new successful process so that could be standardized and spread to other care teams.
Chief Medical Information Officer Danielle Oryn described Petaluma’s technology and process for developing a new care gap within the relevant health information system. The health center stopped using the quality care gaps built into the EHR because they were only right about 70 percent of the time. The power of their quality and care gap system was not the technology, it was in how they expected and planned for failure as a way for it to improve the system over time.
- As they build a care gap, they pull random patient chart review samples to test for false positives and negatives with end users.
- In the relevant system, staff can complain or question when they think a care gap is wrong for a patient. Multiple staff described how staff feedback through this system helped them fix their Hepatitis A/B vaccination measure to exclude people who were already immune based on lab testing. This staff reporting system has also helped improve staff communication and training on particular measures
The relevant system is open to every staff member and every staff member can see a narrative that describes the logic and rules for the measure or care gap, and the detailed SQL code. This transparency helps engage every staff member to be a failure finder.
4. Empower People
“We include and listen.” Goals for how Petaluma works are as important as quantitative results. They include:
- We need staff and patients to feel “comfortable expressing themselves” so that “we can see all sides of the sphere.”
- We need the info from our people and data so that our people can solve problems.
- We “enable people to lead themselves.”
- We make it okay and expect people to “work across silos to solve problems together.” We expect people to “work across the organizational chart” without asking permission.
Collaboration and empowerment are built into the physical design and shift-by-shift processes of Petaluma in a way that cannot be avoided. The standard huddle before each shift builds empowerment of each staff member into the care for every patient. The space, roles, and easy communication technology enables staff to act and solve problems in real time. One of the most important roles on each care team is the flow coordinator, who sits in a commanding position in each team space where the coordinator can see all of the staff and patient flow.
Petaluma creates capacity (for free!) by enabling staff to be more powerful. Petaluma found that its quality results were plateauing. It found that many of the patients not receiving ideal quality had behavioral health or social needs. So it tested and later built into standard care a social determinants assessment adapted from the PRAPARE assessment tool. Of course, it required staff more time to administer, review, and enter the PRAPARE data in the chart. It required even more time to discuss and address the issues PREPARE discovered. However, despite initial staff concerns, there have been no complaints about the additional work required to assess and act on social determinants. Staff now have a new way to listen to and serve patients.
Another example is that Petaluma provides extensive co-located behavioral health services in each care team, but the service did not fully take off until the team designed a pull system to identify patients. The behavioral health staff were concerned that they were not receiving as many referrals as they thought they should. At their own initiative, they reached out to the informatics team to build, test, and refine a care gap for patients who are likely to need behavioral health care. As part of each shift’s huddle, the team reviews a list of scheduled patients who need behavioral health and works with provider-medical assistant pairs to make a referral part of today’s plan. Now, 70 percent of the patients who need behavioral health care today receive it.
Our site visit ended with a discussion with Carol, one of Petaluma’s more complex patients, and her care team, which included Nurit. Carol showed us the power of one patient to change Petaluma. Using motivational interviewing, the team learns from the Carol’s experience and helps her reach her goals.
- Carol’s diabetes care manager said, “Carol does a great job telling you when you don’t know what you are doing and as a provider that is very important to me.”
- Another time, her diabetes care manager was frustrated in a group class and complained to that nobody was listening. Carol said, “Yes we are, this is just a lot of info.”
- Nurit said that Carol has helped her to “learn to walk in the shoes of people who are taking lots of medications and have lots of needs. I don’t make a medication change without having the whole team involved. How might this change affect things in Carol’s life.”
5. Standardize What Works
The foundation for Petaluma’s great results is their standard care system. When Petaluma figures out the current best way to practice, they build it into their standard care system. It found that it immediately reaches performance levels of at least 70 percent once staff build it into their system.
The standard system includes some of these key components; and, like everything else, continues to evolve:
- Daily (two to three times per day) huddles with standard care team work, including Huddle TV.
- relevant care gap measurement that provides decision support for the scheduled visit care plan.
- Petaluma wiki that is used for staff training and annual skills updates.
- Care team roles in the six primary care teams.
- A recall system to engage members with automated reminders based on patient communication preferences.
- A risk score system that segments patients into three groups based on their care needs:
- Low-risk patients are cared for by provider-MA teams and automated recall processes
- Medium-risk patients receive extra attention from RN care managers on each team
- High-risk patients receive intensive support by the centralized care management team.
A key feature of these standard care systems is that they are aligned: the existence of each makes the other components more effective. For example, the relevant measure and care gap system is influential primarily because it is available to all staff and built into the standard work of each care huddle for each team member.
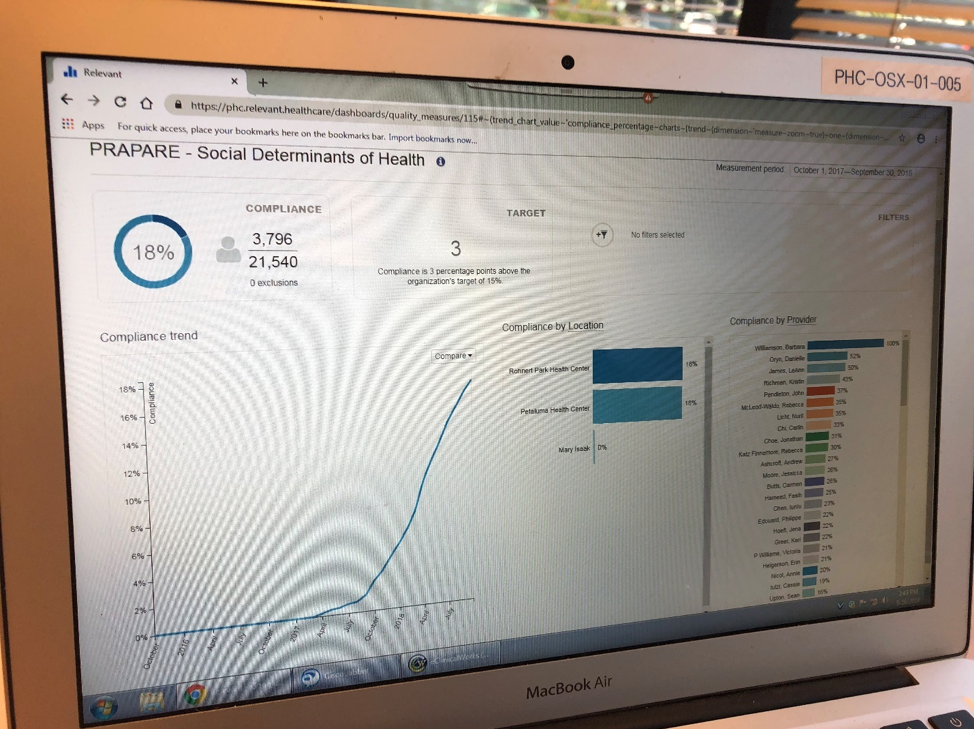
The standard care system is powerful method for moving from Plan-Do-Study-Act (PDSA) testing to develop and refine a change into full scale spread. The Petaluma team refined the PRAPARE social determinants assessment, the process for administration, and the target population through a series of PDSAs. When they were ready, they created a relevant care gap targeting patients with medium risk scores, diabetes, or depression, and build social determinants into the huddle process.
This relevant report shows first part of diffusion of innovation s-curve for completing PRAPARE assessments for target patients (about a third of all Petaluma patients). From the Spring to Fall of 2017, Petaluma did PDSA tests to develop their approach. In the Fall of 2017, they built it into relevant and the shift-based huddle process. About a year later they have screened 18 percent of patients, but this comprises most of the initial target population.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.