Top Takeaways
|

During the rapid shift to telehealth visits during the COVID-19 pandemic, safety net clinics embraced simple, cost-effective solutions to help high-risk patients manage their chronic medical conditions at home.
One of the most striking innovations: A program for people with uncontrolled blood pressure (hypertension) that allowed them to monitor their own blood pressure remotely.
Two health organizations, Community Medical Centers and Northeast Valley Health Corporation, met with success at clinic sites using an “unconnected” remote monitoring system, in which patients manually track and report their blood pressure (BP) checks — a program known as self-monitored blood pressure (SMBP). The innovation was introduced as a solution for delivering high quality, compassionate virtual care that is accessible for all as part of CCI’s Connected Care Accelerator.
“This program is close to my heart.”
For Community Medical Centers registered nurse Daniel Standart, providing home blood pressure monitors — and teaching patients how to use them correctly — is personal as well as professional. “This program is close to my heart as my maternal grandfather, maternal uncle, and my mother died due to coronary artery disease and heart failure,” says Standart, who distributed devices to uninsured patients. “Helping individuals understand the basics of blood pressure and the impact high blood pressure has on the cardiovascular system increases the likelihood of gaining better control of their blood pressure. The self-measured blood pressure program provides the opportunity for the provider and nurse to partner with our patients to promote continuity of care.”
Community Medical Centers is a primary care provider for more than 100,000 patients in underserved areas in three central California counties: San Joaquin, Solano, and Yolo. The centers service area is a mix of rural and urban communities and includes a large agricultural industry that draws migrant farm workers, mostly Latinos. Health care services are in high demand as poor health indicators — including heart disease, diabetes, and obesity — afflict the centers’ communities at disproportionate rates. Almost all Community Medical Centers patients are low-income; one third need care in a language other than English, almost 20 percent are uninsured and 8 percent are experiencing homelessness.
Like other safety net clinics, Community Medical Centers found that during the peak of the COVID-19 pandemic, when in-person clinical visits declined dramatically, the management of chronic conditions such as hypertension became more challenging, according to Maria N. Ortiz, the center’s quality improvement program manager. Case in point: The collection of blood pressure readings occurred less frequently during telehealth consults, compared with office-based visits. For patients with uncontrolled blood pressure, that drop in blood pressure checks made timely follow-ups less likely. Since the condition requires continuity of care and consistent vital signs checking, this was troubling.
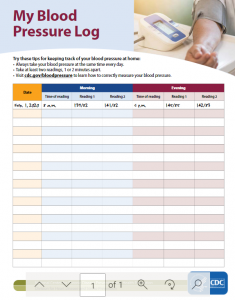 Community Medical wanted to find a solution to this problem and decided to test out a self-measured blood pressure program. It required investing in blood pressure monitors — CMC purchased Omron Series 3 and 5 devices — identifying eligible patients and educating them about how to use the equipment, record their findings on My_Blood_Pressure_Log (left) and develop a system for collecting data and patient follow-up.
Community Medical wanted to find a solution to this problem and decided to test out a self-measured blood pressure program. It required investing in blood pressure monitors — CMC purchased Omron Series 3 and 5 devices — identifying eligible patients and educating them about how to use the equipment, record their findings on My_Blood_Pressure_Log (left) and develop a system for collecting data and patient follow-up.
The health clinic wanted to see if home testing resulted in better blood pressure control and faster follow-up and medication reviews for patients, both insured and uninsured, with uncontrolled hypertension. And it did: Nearly 90 percent of patients enrolled in the program achieved blood pressure control during the following check about two weeks after receiving the monitor. As a result, clinic staff were able to adjust medications in a more timely and patient-centered way as well.
That’s a win-win. This low-tech, unconnected remote patient monitoring solution is proving an ideal complement to a holistic approach to helping patients with high blood pressure. “Teaching proper self-measuring techniques, explaining the basics of blood pressure, defining stages of hypertension and their impact on the cardiovascular system, and laying out a plan that includes home measurements, BP logs, timely follow-up appointments, and provider review to help adjust medication therapy and promote proper diet and exercise all help to promote the health and well-being of our patients that are experiencing hypertension,” explains Standart.
The innovation isn’t without obstacles. “It’s challenging at times when the patient cannot use the devices, when the internet gets disconnected, or the system is down,” says one provider. “It’s a problem with video visits when the patients are not at home when the provider calls and needs to see the patient take their blood pressure.” Community Medical also underestimated the coordination clinic support staff needed to undertake to implement the program, especially as provider referrals were very low, according to Ortiz. There’s a learning curve in making sure staff are aware these devices are available, identify patients referred to receive them, and schedule nurse or medical assistant time to teach patients how to use the monitor and record their readings.
Still, the solution has been well received by nurses, health educators, patients, and providers. Almost all patients who received a blood pressure monitor attended their follow-up blood pressure check visits — either virtually or in-person — and provided a blood pressure log with at least a week’s worth of home blood pressure readings. “Behind the numbers and statistics regarding high blood pressure are individuals and families like mine,” says Standart. “This program has so much potential in promoting health and literally saving lives.”
Lessons Learned
- Choose what works for patients. Although the blood pressure monitor e-prescription request process was more convenient for the Community Medical Centers clinical team, it proved more challenging for patients. Bulk ordering blood pressure monitors through Durable Medical Equipment (for insured patients) proved more efficient.
- Provide a self-monitoring blood pressure packet for each site’s clinical staff with resources such as blood pressure logs, patient education materials on how to check blood pressure at home, and information on how to check device accuracy.
- Schedule self-monitoring blood pressure staff training for all employees involved in the process.
- Set a protocol for medical assistants to collect blood pressure readings during telehealth visits and educate staff on how to document home blood pressure readings in the electronic health record.
“Patients are taking blood pressure more seriously.”
Remote patient monitoring for hypertension was also high on the list of pandemic-driven innovations at Northeast Valley Health Corporation, which successfully implemented both high-tech connected solutions and low-tech “unconnected” options for its patients.
As with every safety net clinic around the state, the COVID-19 crisis dramatically altered the delivery of care at Northeast Valley Health Corporation, a nonprofit organization and federally qualified health center centered in the San Fernando and Santa Clarita Valley dedicated to providing sustainable health care for vulnerable Southern California communities. Northeast Valley provides over 320,000 annual health care visits for 73,050 patients at 14 clinics. More than 15 percent of its patients are uninsured, 77 percent receive Medicaid, and 4 percent are experiencing homelessness. The pandemic pushed this provider and its care teams into adopting virtual care at a phenomenal pace. One issue that proved a persistent pain point: Obtaining blood pressure values and documenting blood pressure readings during virtual visits.
Credit: NVHC
That’s a major concern because the organization serves a mostly low-income Latinx population, and many of the health center’s patients are disproportionately affected by chronic health conditions, including high blood pressure, diabetes, and obesity.
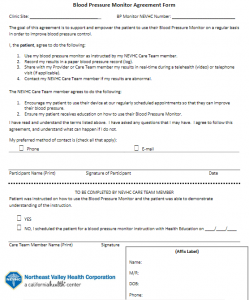
So Northeast Valley implemented protocols to provide non-connected blood pressure monitors through Durable Medical Equipment (for managed care patients) and Health Education (for uninsured patients) in an effort to help patients engage more in their care and manage their hypertension from the comfort of home. During the pilot period, 570 blood pressure monitors were distributed through Durable Medical Equipment and 239 via Health Education.
Initially, the health center scheduled group Zoom classes for education, but it proved more effective to provide education primarily one-on-one and in-person via the family medicine care coordinator, although patients were given the option of telephone or telehealth education too.
There were hurdles to overcome: Even when a patient had a non-connected blood pressure monitor, it was still an issue to obtain their blood pressure value and make sure care team members documented it correctly in the electronic health record.
But the benefits outweighed the barriers. That’s true for both care teams and patients. “Creating a workflow that enhances collaboration between well-trained care coordinators/nurses and the providers-like we have at NEVHC —is vital for maximizing the benefits of a program like blood pressure monitoring,” says a Northeast Valley clinical pharmacist.
For patients, the benefits loom large. “I noticed my patients took their blood pressure monitoring and results much more seriously when they engaged to frequently check their BPs at home,” notes an NEVHC pharmacist. “They were more willing to make medication adjustments and more adherent to their medication regimen plan when they saw how well it helped improve their home BP readings.”
Lessons Learned
- Remind patients with non-connected blood pressure monitors to be prepared to take and report blood pressure readings during telephone or telehealth visits.
- Prompt patients and heath care teams — through text messaging patients and staff reminders — to improve the likelihood that the patient’s BP value is documented in the medical record. Note: Not all patients are able to receive texts, which can impact this strategy.
- Inform care team staff that a patient has a home blood pressure monitor and train teams to properly document the readings in the electronic health record.
- Establish workflows to outline the roles and responsibilities around referral, distribution and instruction of blood pressure monitor home use via care team members, including providers, health educators, and family medicine care coordinators.
- Fail fast and move on: Not all interventions — including small group Zoom instruction classes — are efficient and effective, despite best efforts. Keep going!
|
The COVID-19 pandemic upended the way California delivers health care. Health care systems completely restructured their services to keep both their patients and employees safe. Federal policymakers acted quickly to expand coverage and payment for virtual care. The California Department of Health Care Services also dismantled previous barriers to telehealth and began requiring Medi-Cal managed care plans to pay providers for telephone and video visits at the same rate as in-person visits. As a result, many California health care providers rapidly pivoted from in-person visits to virtual patient visits. For these organizations, this shift has been transformational, as they’ve adopted new technology, overhauled workflows, and redefined team member roles. The Connected Care Accelerator — a partnership between CCI and the California Health Care Foundation, with additional funding from the Blueshield of California Foundation — selected 40 safety net healthcare centers in California to participate in a 12-month program that provided funding, methods, tools and hands-on technical assistance to enhance virtual care initiatives. In a series of case studies, CCI showcases the most sustainable and impactful solutions and shares advice for fellow safety net clinics who want to integrate similar virtual care strategies. |
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.

