When patients are released from the hospital, they often feel confused and overwhelmed—not to mention sick. A care manager is meant to provide continuity between hospital and primary care, but coordinating these two realms can be difficult. Olive View-UCLA Medical Center is testing a system to notify care managers when patients seek hospital care.
Seeing the Problem
Preventable hospital readmissions due to poor post-discharge care coordination are a major source of both patient and provider dissatisfaction. Twenty percent of recently-discharged Medicare patients are readmitted within 30 days of discharge. Cumulative admissions leave patients increasingly debilitated and, according to the Centers for Medicare and Medicaid Services, cost Medicare $18 billion each year. Care managers can help smooth this process, but to have a timely impact they need to know when their patients are admitted to or discharged from the hospital. At the moment, keeping track of patients often requires time-consuming trawls through multiple databases, leaving little room for the more human aspects of care management.
The Patient Perspective
- Safety net patients do not always realize that they have insurance through Medicaid, or that they have already been assigned to a medical home.
- Patients are often discharged without a clear idea of their condition, with instructions they don’t understand and with no follow-up set to continue their care.
- Patients leave the hospital with referrals to consult with a specialist, but those consults are not always honored. When the consulting provider can’t give the patient an appointment, or schedules an appointment for many months later, patients frequently don’t know what to do. Emergency physicians or inpatient teams have no way of knowing when or how to help the patient speed up the process. Without a care manager actively involved after discharge, gaps in care often occur.
Best Uses, Biggest Impacts
While the project aims to improve care for patients, the end-user for the automated email notification system is actually their care managers and primary providers. Without automatic notifications, care managers must manually scan several different databases to find out if any of their patients have been admitted to or discharged from rescue care (unplanned inpatient or emergency department care). This process is so time-consuming that it greatly limits the impact a patient-centered medical home can have, diverting time away from population health management or health coaching. By automating this task, the notification program hopes to give care managers the ability to care for their entire population of patients, including those who may not have visited the clinic before.
How It Works
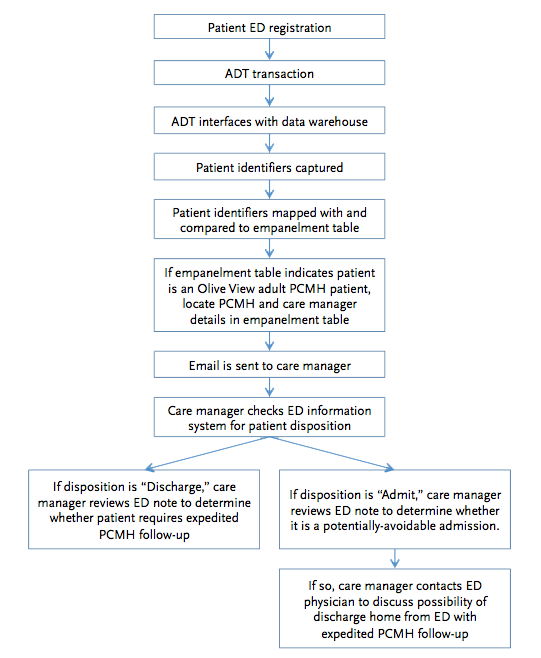
- When a patient is admitted, discharged, or transferred at a hospital, an “ADT event” is automatically logged in their electronic medical record. The notification system is built on top of this existing infrastructure.
- The ADT message is instantly transmitted via HL-7 interface to a data warehouse. A digital filter selects all ADT codes that indicate admission to or discharge from rescue care by adult patients in the system’s medical home.
- The system compares the patient’s medical record number to an empanelment table to find their care manager. If it finds a match within the local clinic system, it sends an email to the patient’s care manager.
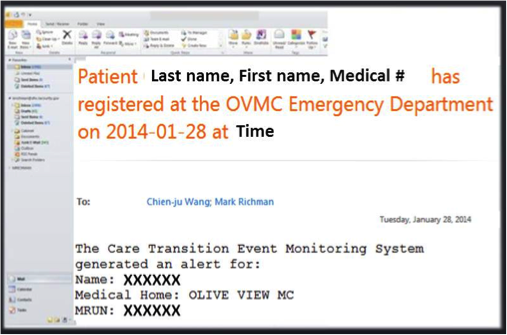
- The email includes identifying information for the patient and the PCMH, and a description of what kind of event occurred (arrival or discharge).
- Such an email could also contain information about previous and upcoming 6 months’ clinic visits, and a summary of the rescue care event.
- The email is designed to be a “one stop shop” for the care coordination resources the care managers need to see the full scope of the patient’s situation without having to check multiple databases.
Lessons from Practice
- In their early trials, Olive View–UCLA Medical Center realized that they needed to be very specific about triggering a notification, or else care managers would be overwhelmed by emails. The system was thus set to only send notifications for patients who were over 18, and who were empanelled at OVMC. In the future the system may be able to expand to include other hospitals’ emergency departments and care managers at other clinics.
- Including information on future and past appointments in the notification email greatly eases the process for care managers. First it confirms that they are your patient, as opposed to someone unknowingly empanelled to a medical home but regularly seeing another primary provider. Second, it helps the care manager identify and prioritize patients who find themselves in post-discharge limbo. If the patient has a primary or specialist appointment scheduled within a couple of days, the care manager may not need to reach out immediately. If records show no appointment scheduled for several months, care managers may need to prioritize that patient.
- To gather data about how helpful it is in preventing readmissions, Olive View created a control group by setting their system to only send notifications for patients with medical record numbers ending in even numbers. By comparing ED and readmission rates between the even and odd number groups, they should be able to determine the efficacy of the program.
What’s Next?
The innovation team at Olive View-UCLA Medical Center sees their pilot project as the start of a wider system that can seamlessly inform care managers of patient hospitalization events throughout the Los Angeles County Department of Health Services network. Currently the system only works for care managers and ED visits or hospitalizations at OVMC. If effective, the system could be expanded to other hospitals and clinics, allowing it to help a larger population, connect many more care managers, and capture hospitalizations across a wider area.
Learn More
- Olive View–UCLA Medical Center is a part of the Los Angeles County Department of Health Services. DHS sees nearly 800,000 patients annually. Nearly 75% are below the Federal Poverty Line, over 80% are minorities; and only one-third speak English as their primary language. Visit their website: dhs.lacounty.gov
- The Safety Net Innovation Challenge provides seed funding and design coaching for innovative ideas that test new solutions to common problems. The Challenge is supported by funding from Blue Shield of California Foundation: blueshieldcafoundation.org.
Find more Incubator briefs on our website: careinnovations.org - Download a PDF version of this brief.




