I love that we are starting to think about health more broadly. Health is all around us and we see it every day. Yet, too often when we talk about health, we still think of it as care provided by doctors, nurses, and clinical staff. Going beyond the clinical walls to embrace a definition that includes the mental, social, and spiritual dimensions of health, as well as appreciating the role community plays in our health, is an exciting shift in our thinking.
At CCI we are exploring the determinants of overall health (how people feel) vs. health care (services provided) and wellbeing. In our work, we recognize that health care alone cannot change the trajectory of health outcomes. We need to partner with community organizations — public health, social service organizations, spiritual institutions — to address the social factors impacting health and wellbeing.
In May, our biannual Safety Net Innovation Network (SNIN) meeting addressed the intersections between health and wellbeing and how we might think of our roles in health care differently as we broaden our definition of health. Without a universally accepted definition for health, for the convening, we used definitions from the 100 Million Healthier Lives initiative, a collaboration of change agents who are transforming the way we think and act to improve health, wellbeing, and equity. The definitions used in the initiative define health as:
- A state of complete physical, mental, social, [and spiritual] wellbeing, and not merely the absence of disease or infirmity. — Adaptation of World Health Organization definition
- “Health is not the absence of disease but the addition of confidence, skills, knowledge and connection. But most importantly, it is simply a means to an end — which is a joyful, meaningful life.” — Cristin Lind
The mantra for our SNIN convening was Embrace, Learn and Act. We embraced a broader definition of health. We learned from local Bright Spots that have successful cross-sector partnerships with their provider or community counterparts. And we got participants to think about and write down their actions for bringing change in their clinics and communities with this broader definition in mind.
As I walked away from the first day of SNIN, I was trying to wrap my head around a structure or visualization for summarizing the relationships between the various content segments, given the complexity of the topic. To help with this, I resorted to one of my favorite quality improvement tools: the driver diagram. I use it to visually demonstrate the theory of change for a specific program, project, or initiative. The driver diagram shows the relationships between the main goals and drivers — or changes and interventions — that contribute to achieving the program’s overall goals. I use the driver diagram to:
- Communicate an overview of a program succinctly to a wide range of stakeholders.
- Engage the frontline, or people doing the work, in our improvement workgroups and teams in a fun way. They can share their ideas on goals and drivers, given their diversity of perspectives, experience, and roles.
- Focus and align ideas generated in brainstorms so ideas are clearly linked to our goals.
For SNIN, I created a driver diagram to visually show the insights and relationships gathered from our meeting:
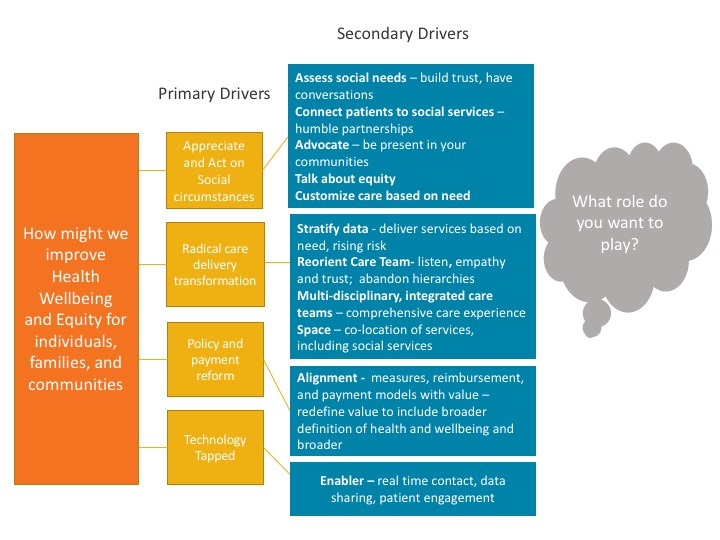
We started with our goals which broaden the definition of health to include physical, mental, social and spiritual; this focuses on wellbeing — living fulfilling and meaningful lives.
From our goals, we heard about the high level primary drivers, categories of big changes that contribute to us achieving our goals:
- Appreciate and Act on Social Circumstances: Collect data on key social determinants of health and establish partnerships in the community to address social needs of individuals, families, and communities.
- Radical Care Delivery Transformation: Provide the right care, at the right time, and in the right way based on what patients NEED, and that there is no one-size-fits-all care. It’s OK to provide different care based on patients’ unique needs — it’s what helps people get better.
- Policy and Payment Reform: Start measuring what matters. Focus on measures that assess the broader definition of health and align reimbursement and incentives with this broader definition and the recognition that the role of health care providers goes beyond clinic walls.
- Technology Tapped: Exploit the opportunities to use technology-based solutions to connect people to community resources, provide convenience and access to care, and effectively engage patients in self-care and self-management.
The secondary drivers are more specific and directly influence the primary drivers. From the secondary drivers, we can begin testing changes that will directly impact our goals. At our convening, Bright Spots and participants shared ideas for achieving a complete state of health and wellbeing for individuals and communities. Highlights I particularly enjoyed were:
- Liz Ogbu taught us how to us a key technique from human centered design — empathy — to ask open ended questions that encourage community members to share their problems and ideas for solutions to those problems.
- Roots Community Clinic: Roots is building step-wise employment opportunities for patients who struggle to find jobs because they have been incarcerated. This clinic has given patients the confidence and skills to secure jobs in their community.
- Toyin Ajayi: Toyin talked about Cityblock, which brings a new way of thinking about and acting on health. Cityblock emphasizes “knowing your population,” so that you can customize care and services based on their needs vs. providing the same care to everyone. This requires robust data that includes physical and social needs data, an appreciation of partnering with community-based organizations and providing social services together in the same space, and using technology to make health more portable.
I continue to be inspired by the research and literature focused on our evolving understanding of what we consider “good health” and how we, health care providers, might engage in creating better health outcomes for the individuals we serve and our communities. To learn about the ideas shared that were part of these secondary drivers, please read our SNIN insights and materials from the convening.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.