Dear Friends,
Here at CCI, we’re so proud of our safety net partners — the public hospitals, clinics, health care centers and networks, Indian health centers, and community-based organizations that work with us. Thank you for all your hard work! Together, we made great strides toward creating fair, just, and inclusive opportunities to be healthy. In 2022, here’s what our portfolio of programs and initiatives accomplished:
- Resilience: Deepened the practices and tools that help patients recover from trauma, navigate challenges, and rebuild connections in a time of pandemic upheaval and a nationwide mental health crisis.
- Addiction Treatment: Increased access to lifesaving medications and treatment for patients with opioid use disorder.
- Virtual Care: Shrunk the digital divide, while protecting and expanding the telehealth gains that we made during the pandemic.
- Behavioral Health: Took our first steps towards working with partners to recognize and treat substance use and mental health disorders with an equity-centered approach.
- Changemaker Community: Accelerated the pace of innovation to improve health equity through rapid experimentation, human-centered design approaches, and community building.
We invite you to take an inside look at our extraordinary collaborations this year. As our team photo below suggests, even though this work is challenging and often overwhelming, it’s also joyful and fun.
Warmly,
The CCI Team

The CCI team gathers at our first in-person retreat since the start of the pandemic.
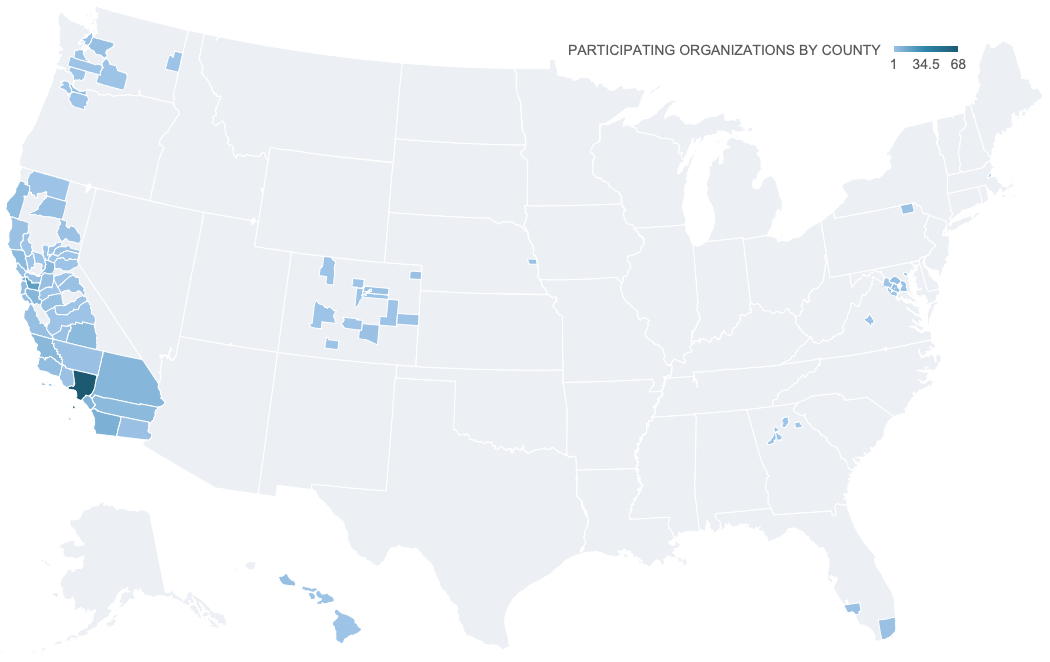
IN 2022, the center for care innovations RAN
14 PROGRAMS
that COLLABORATED WITH
308 ORGANIZATIONS
THAT SERVED A TOTAL OF
12.6M PEOPLE
Resilience
Now more than ever, supporting providers to help patients (and themselves) recover from trauma and devastating loss, navigate tough challenges, and rebuild connections is integral to our resilience work. Health care workers continue to struggle through the pandemic, experiencing exhaustion, dwindling resources, and natural disasters. The mental health of many Americans is in tatters. More than 140,000 children lost their parents and caregivers to COVID-19. Many adults have lost their jobs, homes, and health care, while hate crimes are on the rise.
Since starting this work, we’ve trained clinics and health centers representing hundreds of thousands of patients in trauma- and resilience-informed care, which emphasizes the importance of understanding a patient’s life experiences and developing a trusting relationship in order to deliver effective care and improve long-term outcomes. It can also help prevent physician burnout and staff turnover.

To understand the needs of community members — and to gain their trust and respect — the Live Oak Youth Partnership meets them where they are: schools, local parks, neighborhood clubs, community organizations and the like.
In one Sonoma County clinic, a provider attributed this CCI training to his clinic’s ability to confront the unthinkable, telling us, “We had a major flood — a historic flood, and our clinic was almost underwater. We also had the fires, something that deeply impacted not only our patients but our staff. We had a heavy year of personal loss — people who passed away, people who lost their homes.” But because of the clinic’s work on trauma- and resilience-informed practices, he said, people at the clinic were able to support each other and their patients through these climate change disasters.
In 2022, our partners expanded their work to many patients and communities still raw from the turmoil of this pandemic era. In one CCI program supporting San Francisco Bay Area safety net clinics, our participants practiced a strength and dignity-based approach to family health care focused on healing and an anti-racist approach to caring for children.
Preventing relationship violence was the focus of another one of CCI’s programs in California. Created in response to the pandemic-related rise in domestic violence — a problem that already affected more than 30 million kids and teens across the country — the program’s the multi-sector partnerships worked with teens across the state to help them avoid dating violence and create healthy, loving relationships. This included creating zines and other media that model healthy relationships for pre-teen boys, videos and messaging to prevent teen dating violence, and incorporating Native culture to instill pride and confidence to help ward off intimate partner violence.

The McKinleyville Healthy Relationships Coalition incorporated activities that foster cultural, social, and emotional connection to encourage youth to make healthy relationship choices.
Timiza Wash, the director of equity and transformational change at WEAVE, a member of the Healthy Black Families Collaborative, told CCI:
“We’ve learned that we don’t have to do this work alone. We are stronger in partnership because we can depend on each other, learn from each other, collaborate, and share the load.”
Addiction Treatment
With the overdose epidemic still looming over the country, we’ve continued to advocate treating addiction like all other chronic diseases. The key to that goal is increasing access to medications for addiction treatment (MAT), the use of lifesaving medications in combination with counseling and behavioral therapies.
To date, after working in this space for six years, our addiction programs have increased the number of active MAT prescribers by 191 providers — equivalent to more than two active prescribers per participating clinic.
In turn, these prescribers have changed the lives of countless patients. We’ve supported our participants in helping more than 2,199 patients receive MAT. Many participants doubled or tripled the number of patients accessing MAT for opioid use disorder.
One patient who is being treated at one of our participating clinics told CCI, “I’ve been on the streets for years doing the same thing and just seeing so many people I know die from overdoses. This clinic welcomed me and was there to support me regardless of what happened and that made it easier for me to keep coming back if I made a mistake and get the help I want and need.” Other patients were also deeply appreciative of providers’ patience and support, with one adding, “I am grateful for the staff for not judging me.”
Central to this program’s success was the creation of learning communities, which offered a structured forum to develop new capabilities, share best practices, and discuss lessons learned. The team at Adventist Health Feather River told CCI:
“You held us accountable, kept us on track, and supported us all the way. We and the community are indebted to your stabilizing foundational work. Many thanks.”

CCI staff and program participants greet each other during a virtual learning session.
Virtual Care
Virtual care often brings to mind the image of a provider in their office talking through a screen to a patient at home. But for CCI and our partners in 2022, this next frontier of care delivery reached patients in tent cities and shelters, schools, clinics, and even in cars in parking lots. These are people facing major — and multiple — barriers to accessing care.
One CCI program supported clinics looking to solve complex challenges associated with the implementation, improvement, and sustainability of virtual care in Washington, Oregon, California, Hawaii, Colorado, Georgia, Maryland, Virginia, and Washington, DC. To hear from voices in the field, we sent a documentary crew on the road. With CCI’s support, the Community Clinic of Maui, which works with tent cities along the coast, was able to add a nurse to its street medicine team that uses telehealth to connect unhoused patients with physicians back at the clinic. That new nurse, Charlotte Jones, told us:
“The patient gets the care, and you see the look of relief that they didn’t have to go to the emergency room and be let out at the middle of the night to try and figure out how to get back to their encampment. And that makes it all worthwhile.”

Charlotte Jones helps an unhoused patient see a provider.
Our other mini documentaries show health tech navigators building connection in houseless shelters in Los Angeles, the joy of culturally competent translations in Denver, and telehealth counseling for addiction in Orange County, California. In the latter, Christopher Rodas, a patient who has struggled with a substance use disorder for 14 years, says telehealth is helping his recovery: “A lot of us are in situations where we don’t have licenses, we can’t travel, we’re house-arrested, or people are just coming out of penitentiaries and they need the help, but they don’t know where to go. They don’t know where to turn, but if you have a phone, it’s right there.”

Christopher Rodas said, “The program helped me out throughout my journey and in knowing that I’m not alone in that journey. It’s like a blessing.”
Two years ago, at the start of the pandemic, another one of our virtual care programs created a telehealth testing ground for California health care organizations. In 2022, we looked at the data and saw that many patients who can benefit the most from telehealth still aren’t receiving it. So we kickstarted the next phase of that program with a new virtual care equity collaborative, where our participants continue to work on closing those care gaps. As one leader said, “The people who are facing the digital barriers are often the same families that are facing challenges in terms of transportation and competing demands. Telehealth has huge potential to improve equity and access to care, but we’re not going to get there until we address the digital and language barriers.”
In 2022, CCI also continued building out the Virtual Care Learning Hub, where we’re sharing the best of the best for improving health equity through virtual care. We’ve synthesized 20+ years of experience to create this learning hub filled with great ideas you can start testing right away. There you can find a telehealth scheduling guide, which helps frontline staff, schedulers and care team members determine if a patient’s needs can be addressed with a virtual visit. And be sure to check out our journey map for virtual visits, which allows you to click on a timeline and find helpful resources for each step along the patient journey in telehealth – and to filter by different audiences, from patients to administrators.
Behavioral Health
One of our newest programs addresses a growing mental health crisis. People with behavioral health conditions suffer poorer health overall, and those with serious mental illness or substance use disorder risk dying 20 years earlier than others. Yet even in California, access to behavioral health services is maddeningly slow and inequitable, especially for people of color.
Using an evidence-based model, our participants are learning how to recognize and treat mental health and substance use disorders, identify urgent social needs such as food insecurity, and reduce barriers to care – including racism, discrimination, stigma, and trauma – by embedding health equity practices in all their programs.
And through this work, we’re starting to return to our one of our most-loved CCI activities — site visits. The program traveled to Cherokee Health System in Knoxville, Tennessee, to check out its nationally-acclaimed integrated behavioral health work and learn practical approaches from this exemplar organization. It was a trip that participants found inspiring, fun, powerful, and deeply gratifying. One told CCI:
“I am having positive vibe withdrawals. It was a real privilege to be amongst such a positive and forward-thinking group.”

CCI participants tour the clinic and speak to different members of the care team.
Changemaker Community
At CCI, we grow and nourish changemakers in every single one of our programs. These are the folks that inspire, challenge the status quo, and embrace community wisdom. But we also run skill-building programs so that they can better ideate, prototype, and test to bring about real, lasting change.
In 2022, our award-winning “design thinking” program supported the recovery and renewal of our communities in the wake of the pandemic. Participants reported that the program helped foster a much stronger relationship with their community partners and community members at large. One mentioned how discussions of racism, although “inherently uncomfortable,” gave them and her coworkers hope that their health care organization would change for the better. Said another: “A strength of the process was the depth of relationship with our community. People felt like they were being included in the process. They felt listened to. They felt valued. They felt respected for their time.”
Among the program’s most gratifying community partnerships was one led by Marin County, which discovered that social isolation was one of the root causes of deaths among unhoused people. The county started a circle called “seed of hope” to foster social connection through art, meditation, goal setting, group text chats, and other activities, which resulted in more engagement and better health care.
CCI also brought design thinking to Colorado, where applied projects span designing a mental health website for youth to using technology to prevent unnecessary emergency room visits, and the National Association of Community Health Centers, where participants are using the same methods and mindsets to improve vaccine equity among vulnerable patient populations.
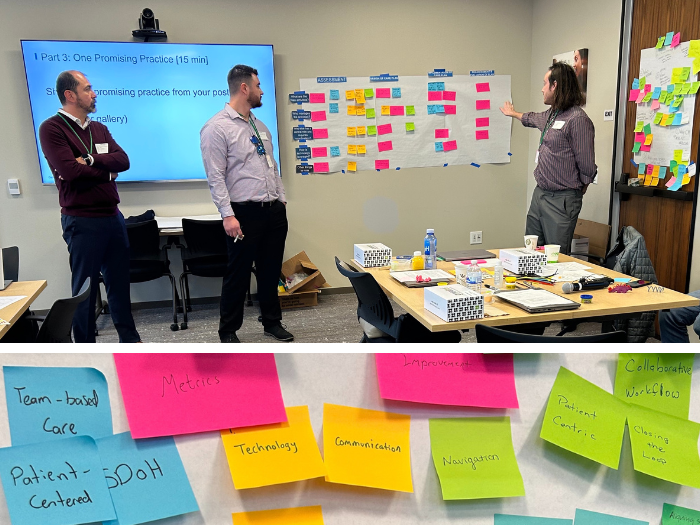
CCI participants discuss the care coordination process to surface best practices, gaps, and areas for improvement.
To experiment with community building online, CCI leaned into podcasting in 2022 — sharing generously and learning from one another, so no one has to reinvent the wheel alone. Our Health Pilots podcast highlighted the successes and failures that emerged from CCI’s program that helps safety net health systems to vet, pilot, evaluate, and spread innovative digital health solutions. Our community taught us how to revamp the patient portal, create an automated patient recall system, and hire community health tech navigators. Dr. Anshu Abhat, director of patient engagement in the office of patient access at the Los Angeles County Department of Health Services, told CCI’s podcast hosts:
“It’s been a very joyful time to be able to see our navigators getting trained. It’s a lot of young people who are bilingual, who are of the community, who really bring a tremendous energy.”
We also partnered on a California “test to treat” program teaching folks how to speed delivery of lifesaving COVID-19 medicines. CCI has engaged organizations across the state to learn from each other in peer groups, work with expert coaches, and receive technical resources, making it easy for community practices to learn from each other and improve equity and access to COVID-19 treatments.
And in the waning months of 2022, we launched a telehealth improvement community, which is working to expand access to video visits in the safety net. Our lessons learned will be open to all — we hope you’ll join us as we innovate together next year.
Thank you to all our program participants and alumni – we have so enjoyed working with you. And lastly, a big thank you to our funders: we couldn’t do it without you. We want to express our gratitude for our past and present funders, including the support and funding for 2022 from the Blue Shield of California Foundation, California Department of Health Care Services, California Department of Public Health, California Health Care Foundation, Cedars Sinai, Colorado Health Foundation, Genentech, Kaiser Permanente and the regional associations and primary care associations in states with Kaiser Permanente providers, National Association of Community Health Centers, National Health Care for the Homeless Council, and Physicians for a Healthy California. Also, thank you to our board and Tides for their unwavering support.