Quick, what’s most likely to be read: a text, email, or message on a patient portal?
If you said “text,” you’d be right. Around 99 percent of people read a text message, and 90 percent of them see it within three minutes, according to a company that specializes in business message market intelligence gathering. In contrast, email is read around 20 percent of the time. And a patient portal message? Just seven percent of the time.
Given that data, little wonder that safety net clinics are turning to short message service (SMS), more commonly referred to as texting, to reach patients where they are. Read on to find out how a rural Colorado hospital and clinic found success rolling out a texting platform for their patients – and how they dealt with hurdles along the way.
Making Patient Texts Secure

Jessica Skomp, Family Nurse Practitioner, getting ready to use OhMD for a patient’s telehealth visit.
With the emergence of the pandemic, Melissa Memorial Hospital—a small critical access hospital located in the rural agricultural region of Holyoke, Colorado—wanted to streamline healthcare for patients and offer them a safe way to access their providers. So did the Family Practice of Holyoke, a certified rural health clinic located in the west wing of Melissa Memorial Hospital. The clinic, staffed by two full-time physicians, one part-time physician, and two full-time nurse practitioners, serves a mostly underinsured population; almost half its patients identify as Hispanic/Latino.
Prior to the pandemic, the practice did not have a HIPAA-compliant way to share information via a smart phone or tablet that integrated with athenahealth, its electronic health record (EHR). But its providers wanted one. The coronavirus made contactless healthcare a necessity and catapulted this type of digital solution to the top of its to-do list.
Early on in the pandemic, it became evident that the EHR the family practice uses did not offer text messaging communication services, says Jayden Miracle, clinic manager. In addition, its telehealth platform, Miracle notes, didn’t offer a satisfactory solution. That product option was in beta testing at the time and did not meet the practice’s telehealth needs.

“Daisy Test,” a test patient, was sent our standardized intake form to complete before a telehealth appointment.
So a team tasked with solving this dilemma decided to shop around for an alternative digital option. That’s where OhMD enters the picture. OhMD is a HIPAA-compliant texting and telehealth platform providing two-way messaging, video visits, and form and survey sharing. It also transmits reminders and allows for automatic messaging, which can increase provider-to-patient contact and care coordination through improved team communication—all while integrating information into a patient’s EHR.
OhMD has been widely adopted at Melissa Memorial Hospital. Providers use the platform to provide telehealth services. Front office staff use OhMD to obtain consent and insurance forms and to complete intake forms. Medical assistants use OhMD to communicate with patients. And the software product is used by management to send broadcast reminders to patients and automatic messages.
It took some finessing and fancy dancing to integrate OhMD with the hospital’s existing EHR. But the pay off—in terms of patient and provider satisfaction—has been worth all the hurdles, according to Miracle.
While the clinic was able to integrate OhMD into its electronic health record, OhMD had to be utilized on a different platform and forms had to be downloaded into a PDF to be uploaded into the EHR, Miracle explains. “This was not true integration to us. We wanted a platform that would directly input information into the EHR.” Still, they made it work.
Oh OhMD
Once OhMD was identified as the product of choice for a pilot program, the project kicked off quickly. Staff training began in June 2020; in July the hospital conducted pre-pilot surveys with patients and staff. The project surveyed a total of 11,116 patients who gave consent to receive texts. In the survey, 75 percent of the patients said they were ready to utilize telehealth services. About 50 percent of care team providers polled in a pre-pilot survey expressed readiness to integrate and utilize telehealth services in the clinic.
The project team–including medical assistants, registered nurses, front desk staff, providers and management—embarked on a steady, measured roll-out of different service options to allow patients to receive care that was both HIPAA-compliant and socially distant. In August the team developed workflows to implement aspects of the messaging option and began utilizing the telehealth platform. In September, they developed workflows to implement broadcasts and reminders; the following month the team tackled electronic patient information forms.
In December 2020 the team wrapped up the pilot with post-pilot surveys for staff and patients and a final evaluation of metrics and outcomes. They determined that OhMD was a good match for the organization and would continue. By the end of the pilot, OhMD services had been adopted by 75 percent of providers and patients. At the Family Practice of Holyoke, 100 percent of clinical staff had integrated the service into their workflow. OhMD scored a perfect 100 from respondents, who noted they were satisfied with the new service.
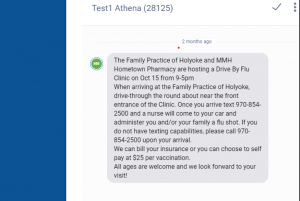
The Family Practice of Holyoke used OhMD to share a broadcast message with all patients regarding an upcoming drive-by Flu Shot Clinic.
There were other benefits: The family practice no-show rate dropped by 8 percent from 2019-2020. And while patients in all demographics use the service, staff members encouraged patients with chronic conditions that are high-risk to use telehealth services to avoid adverse health outcomes due to avoiding care. In 2020, 93 patient appointments were provided via telehealth, which represents a large percentage of this small practice’s patient population.
OhMD is a product for pandemic times and beyond. In March 2020, when Medicare announced it would cover telehealth services for an unspecified time, safety net clinics were able to accelerate the integration of creative digital innovations to treat clients from afar—and still receive critical provider reimbursement. The Vermont-based startup communication platform centered around texting integrates with major EHR platforms including eClinicalWorks, Epic, Cerner, and Allscripts.
Ethan Bechtel, founder of OhMD, might run a startup, but his family has been in the business of finding software solutions for health clinics for some time. His mother, an orthopedic nurse practitioner turned X-ray tech, earned her MBA and started a business providing financial services software to medical practices. Bechtel began working for the family firm after college and honed in on electronic medical records as the next frontier. He figured out fast that one of the greatest challenges for online medical portals was communicating with patients—that was the impetus for OhMD. As part of the company’s pandemic response, it began offering a free version of its patient-text platform to health care organizations (though the Holyoke clinic paid for this service.) OhMD also fast-tracked a video function it planned to release later during the pandemic.
“This is an inflection point for a number of us in this space,” Bechtel told a reporter for Entrepreneur. “I think if there’s a silver lining at the end of all of this, we’re going to look back and wonder why it took a pandemic to force us to use technology that actually improves patient care and access.”
Overcoming Hurdles
The integration of OhMD wasn’t without its challenges. Melissa Memorial Hospital’s original understanding was that the new product would fully integrate with the existing electronic health record (EHR), and that information would flow into or auto-populate in the EHR without prompting. Instead, MMH staff found they needed to do the initial upload of data into OhMD. Miracle explains that OhMD is its own platform that requires manual data entry of forms to be uploaded into an electronic health record.
Tamara, our population health nurse, is sharing a goal set with one of her patients. (No personal health information, or PHI, is present in this picture.)
Once a clinic visit was complete, clinic staff had to manually process the data back to athenaHealth. Given these extra steps, the hospital had to push back the rollout date for the service to re-think workflow plans. Telehealth visits were able to automatically update in athenahealth.com, notes Miracle, but e-forms and insurance cards had to be automatically uploaded. There were also hiccups with the hospitals existing intake forms, which had to be converted to OhMD Forms and required separate login, training, and workflow.
And the initial video telehealth visits proved frustrating for both patients and providers and often ended up defaulting to phone visits. It was mostly operator error: Initially, patients were selecting “deny” when asked to connect with audio or video on their devices. And providers wanted a fast fix to this newcomer problem. The hospital decided to send instructions to patient on how to connect for telehealth appointments via medical assistance appointment reminders—and voila—the problem was solved.
A big victory came with the implementation of the OhMD broadcast service option. The hospital’s first broadcast announced a flu shots clinic to more than 11,000 patients. Only 47 patients opted out of receiving such messages. And the announcement proved effective: There was such a large turnout for the flu clinic day that the hospital almost ran out of vaccines. A queue formed around the hospital building and the clinic provided 77 flu shots that day while the pharmacy provided a further 60 jabs.
And don’t believe the aphorism you can’t teach an old dog new tricks. The biggest demographic for the OhMD platform is patients with chronic condition aged 65 and older. Contrary to widespread perception, senior patients took to the technology and expressed gratitude that they were still able to meet with their providers and receive the care they needed in the middle of a pandemic, despite the uncertainty swirling around COVID-19 and the need for social distancing.
Winning Over Staff Skeptics
The innovation team knew it was vital to engage key clinical leadership to aid in staff acceptance of this innovation. There was apprehension among some management staff—including a clinic provider—around making changes that could cause potential disruptions to clinical workflow or have a negative impact on patients. Project managers worked collaboratively to ease these concerns, listening to their worries and suggesting possible solutions, according to Miracle. Team leaders and hospital management stressed that this was a pilot project. If, at the end of the pilot, staff had significant reservations about the innovation, then project leaders would explore other solutions.
For front office staff, the innovation was a no brainer. “We save time [because we’re not] filling out time-consuming paperwork,” says one front desk receptionist. “It was mostly a seamless process and an easy transition.”
Notes another front-line screener: “We could get each patients’ different point of view on their experience at the clinic or during their visit without having to call them directly. We know the patients receive our messages, unlike phone calls, that sometimes are not answered.”
Patients, too, embraced the technology. “I was able to check into my appointment and send health insurance through OhMD before seeing my doctor,” says HD, a young adult who has attended the clinic for two years. “It was easy to use and I did not have to wait.”
The bottom line: Front desk staff appreciate that they are able to begin the intake process with patients before they present for their visits and collect insurance information electronically. Medical assistants are gratified that they can still interact with their patients one-on-one. And providers would rather see their patients virtually than not at all.
Lessons Learned
- Remember vendors are selling a product and may sometimes downplay potential problems. As in any sale, it’s buyer beware.
- Ask potential vendors lots of questions—even the seemingly simplest of questions about systems compatibility, usability and workflow.
- Patience is important: Innovation takes more time than you think it will. It’s crucial to allot reasonable time for vendors to complete the tasks requested by a team. Ask the vendor for their best estimate about how long a task will take to complete.
- Changes and progress doesn’t happen overnight—nor do they need to. Give the staff time to adjust and readjust to changing workflows.
- Test and then test again. Checking that a pilot is running smoothly is key to a new innovation’s rollout success during launch.
- Manage expectations. When things don’t turn out exactly how a team had hoped, it can be tough to continue to collaborate or muster excitement for the next phase. Create realistic goals and figure out ways to fuel enthusiasm for successes along the way.
Next Steps
- Integrate OhMD with mental and behavioral health services.
- Expand OhMD to provide payment portals, payment reminders, and billing information to patients.
- Use OhMD to share care plans with chronic care management patients.
- Incorporate OhMD to integrate remote patient learning.
- Send out patient feedback surveys and analyze results.
_____________________________________________________________________________
Melissa Memorial Hospital is part of a CCI collaborative designed to support innovation to better address the health of historically underserved Coloradan communities. The Colorado Health Innovation Community (CHIC) helps health care safety net organizations identify, test, and evaluate new approaches with the potential to improve care experiences for low-income Coloradans. The program draws on human-centered design and sustainable solutions for patients and staff alike, with an emphasis on technological innovation that can help strengthen health and health care. MMH is one of seven clinics in the cohort, including Clinica Family Health, Every Child Pediatrics, Jefferson Center for Mental Health, Mental Health Center of Denver, Solvista Health, and STRIDE Community Health Center. Partners on the project include Colorado Health Foundation, The Colorado Health Access Fund of the Denver Foundation, Rose Community Foundation, Community First Foundation, and Colorado Access.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.

