CCI spoke with Arlene Brown, Recovery Support Navigator at Northern Inyo Healthcare District, to learn more about how they build relationships inside and outside of their MAT clinic to support patients with opioid use disorder (OUD).

Northern Inyo Healthcare District partnered with local law enforcement to help those struggling with opioid use disorder by creating a pathway to treatment.
How did you develop your relationship with the sergeant of police? Why was it important for you to develop this relationship? The local high school in our area was hosting an opioid awareness event, so I called to offer support by providing an informational booth with local resources. Sergeant Ron Gladding, Bishop’s narcotics operations supervisor, was doing part of the presentation and the principal of the school asked us to help present. From that point on, we developed a relationship and I told him that I would be happy to come meet people when he encountered anyone who needed help. Sergeant Gladding did just that and began calling me to meet with people. He has transported people to the emergency room to meet with me as well. It is important to me that we have allies across all sectors because it helps reduce stigma and discrimination and encourages people to reach out for help. Additionally, it is a crucial component to reducing fatal opioid overdoses because people will be more likely to call law enforcement when they know they are coming to save a life and not to make arrests or be punitive. Modeling this relationship with law enforcement will hopefully set the standard and inspire other agencies and officers to reach out more for assistance that can help save lives and interrupt cycles of addiction.
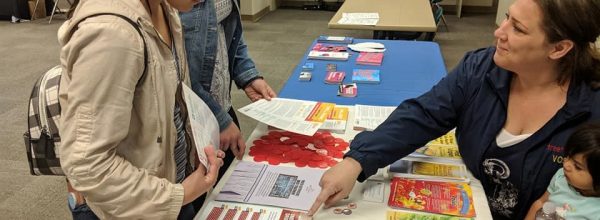
In August 2019, Northern Inyo Healthcare District hosted an Overdose Awareness Event to educate the community.
Can you tell us about your Overdose Awareness Event? Who was involved in putting this event together? Outreach services, such as events, are crucial to help inform the community. I and another community member organized the event and asked local organizations if they wanted to support it. Owens Valley Career Development Center provided 150 dinners and Northern Inyo Hospital provided dessert. We gave out 150 Opioid Overdose Kits which included Narcan, CPR masks, gloves and resources. We provided Naloxone training and overdose education and we also had Dr. Anne Goshgarian, physician at Northern Inyo Healthcare District and our ED Champion, present on OUD. Sergeant Gladding shared more about his role as a police officer and encouraged people to always call 911 when someone is overdosing. Additionally, Antonio Cardenas Jr., a harm reduction advocate who specializes in community healing, gave a presentation on native MAT and the benefits of making MAT culturally specific. I also presented on the dangers of stigma and discrimination and how, as a community, we can work toward changing the narrative surrounding addiction and the way we talk about it.
In January 2020, Northern Inyo Healthcare District is presenting at a local event to educate and empower friends and family members of those with OUD.
Tell us about the upcoming event. What members of your MAT team are involved? In January, Dr. Goshgarian and I are going to present at an event hosted by the tribal community. The name of the event is How to help a loved one with Opioid Use Disorder. For me, it is really important for family and friends to receive education about OUD and treatment options. Friends and family are there more than we are and can observe how their loved one is doing, including whether or not they’re taking their Suboxone. Or, they can be there in times of a relapse and be trained with Naloxone in case they need it.
You mentioned that much of your success is due to you having a supportive and involved MAT team. Who is on your MAT team and what are their roles/responsibilities? We have a great MAT team and we all work really closely with one another. We have four x-waivered providers at our clinic. Dr. Goshgarian comes on Monday and sees a majority of patients in the program. I am the Recovery Support Navigator and I usually am the first point of contact for people looking for help or who have questions. I also meet patients in the emergency room when asked. Additionally, I help with Narcan distribution and we recently were approved as a state-authorized syringe exchange program, so I have a play a large role in that as well. I also do groups for our MAT program and we are looking at starting a Contingency Management Program which I will run. We have 3 RNs who help with our MAT patients and they can also do ASAMS with them. We have a licensed clinical social worker and she puts the patient’s treatment plans together.
Is there anything else you feel we should share with the larger ATSH network? We work really hard to ensure that we have the lowest barriers to receive help. All of the staff at the clinic had received training on historical trauma and MAT. Additionally, staff have received training on stigma and discrimination so patients are hopefully never exposed to any of that. Community outreach is really important as we try to reduce infectious diseases and empower those with lived experience that they are worthy of any and all the help we can provide. Truly, everyone should have a seat at the table, no matter what their story is.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.