Who Should Watch these webinars?
Anyone looking to “share the care” within their care team—especially with nursing team members—but aren’t sure how. This web-based learning series features pioneers and practitioners of nurse-run hypertension care. Facilitated by Kate Colwell, MD, the comprehensive series covers:
Part One – The Case for Nurse-Led Care and Options for Implementation
Our Big Takeaways
- Nurse-run hypertension care– having an expanded role for nurses in the care management of patients diagnosed with hypertension–is an effective way to “share the care.”
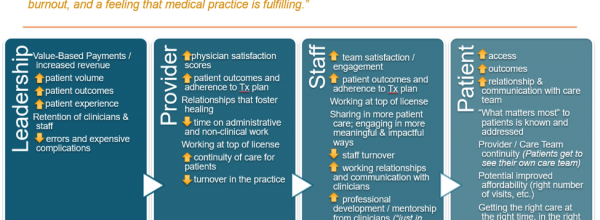
- Nurse-run hypertension care supports the quadruple aim: 1. Improved population health, 2. Reduced care costs, 3. Satisfied staff, and 4. Satisfied patients.
- There is no one way of doing nurse-run hypertension care. Common models include: standing orders, standard work, co-visits, and standardized RN procedures. There are organizations in PHASE doing all of these models as well as pharmacist-run clinics.
Part Two – Developing the Guidelines and Procedures
Our big takeaways
- Start small, but start somewhere. If hypertension care seems too big a leap, other RN-run clinics could include IZ clinics, lice treatment, etc.
- Nurses taking on functions traditionally done by physicians work under standardized procedures or protocols.
- Successful implementation hinges not only on external legal compliance (in CA, defined by Business and Professions Code 2725) but also approval from internal leadership. Involve these stakeholders early on.
- MDs can be convinced by evidence. Evidence is used to develop guidelines and guidelines need to be translated into workflow. Workflow is refined, refined, refined.
- Above all, getting buy-in from clinical staff and patients is a matter of change management and building trust.
Part Three – Moving to Action: Training & Implementation
Our Big Takeaways
- Making a good nurse-run care program work is an ongoing process, nurse training, the right technical tools and EHR integration, continual nurse support, and troubleshooting.
- Training nurses in both clinical competencies and communication helps increase confidence and buy in from both nurses and providers. Provide continuing education to refresh knowledge periodically.
- Make the right thing to do the easy thing to do: Build standardized procedures and protocols into EHR workflow and make them accessible for reference.
Resources referenced in this series
- Webinar: Practical Considerations for Applying the New Hypertension Guidelines, Dr. Mike Rakotz
- Alameda Health System’s Nursing Standardized Procedure Training
About the Speaker

Kate Colwell, MD
Kate Colwell is a retired Family Medicine doctor who consults on projects that will transform healthcare. She currently works with Safety Net clinics to develop systems changes. Her work focuses on teaching and coaching on quality improvement skills to improve clinical care the health of populations.
Dr. Colwell received her BSN from UCSF School of Nursing in 1979; a Masters in Health and Medical Sciences from UC Berkeley in 1985, and an MD from UCSF in 1987. After completing a residency in Family Medicine in 1990 at the Contra Costa Regional Medical Center she had a busy Family Practice at the county’s Richmond Health Center for 18 years.
In addition to clinical work, for the past two decades Dr. Colwell has focused on improving the quality of care for underserved patients in California. From 2000-2004 she was the Assistant Medical Director of Contra Costa Health Plan and from 2004 to 2008 Dr. Colwell led chronic illness improvement work for Contra Costa Health Services. In 2005 she completed a two year Health Leaders fellowship, sponsored by the California Health Care Foundation. From 2006-2012 she was Medical Director of Contra Costa’s Health Care for the Homeless.
In the 1970s, prior to becoming a physician Dr. Colwell was an organizer for the United Farm Workers Union, and then a health worker and lay midwife in UFW clinics. As an RN she worked in a community clinic in New Mexico and then was a Labor and Delivery nurse at San Francisco General Hospital while completing pre-med and medical school.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.