Asthma is expensive. This chronic inflammatory disease costs the United States $56 billion each year. It’s among the leading causes of hospital stays for children, and adult suffers miss about 14 million work days a year.
To reduce hospitalizations and emergency department visits, Northeast Valley Health Corporation piloted Propeller Health, a digital platform for respiratory health management. Through inhaler sensors and internet-connected apps, Propeller helps both patients and clinics better proactively manage asthma.
A Digital Therapeutic
Northeast Valley Health Corporation (NEVHC) knew that if could educate patients to better control the disease, it could lower its high rates of emergency department (ED) visits and hospitalizations.
Through our Technology Hub program, NEVHC discovered Propeller Health. Combining this new technology with tried-and-true care coordination, this is how the health centers put it to work:
- An asthma care coordinator provides education, enrolls the patient in Propeller Health, and helps the patient download the Propeller app onto their smartphone.
- The care coordinator attaches a Propeller sensor to the top of a patient’s two types of medication:
- A long-term “control” inhaler, which is used regularly to manage chronic symptoms (airway swelling, mucus, chest tightness) and prevent asthma attacks.
- A quick-relief “rescue” inhaler, which is used in emergencies to relieve symptoms of an asthma flare-up (wheezing, coughing, shortness of breath).
- Every time an inhaler is pressed, the sensor’s Bluetooth transmitter communicates with the app, logging the time, location, and type of asthma event. The app gives patients insights on their triggers, helping them understand if air quality, temperature, or humidity are causing symptoms.
- At the same time, the app reminds the patient to stick to their medication plan and track asthma symptoms.
- Back at the clinic, the care coordinator can see this data on a dashboard. The care coordinator can monitor if the control medication is being taken on schedule and analyze what environmental factors may be triggers. And alerts are sent out to the care coordinator if the patient is frequently deploying the rescue inhaler.
- If Propeller indicates a patient’s asthma is “poorly controlled,” the care coordinator contacts the patient by the seventh day to ask about asthma education or counseling. If needed, the coordinator will schedule a face-to-face session.
- If Propeller indicates a patient’s asthma is “not well controlled,” the care coordinator contacts the patient by the 14th day to ask about asthma education or counseling. If needed, the coordinator will schedule a face-to-face session.
- If Propeller indicates a patient’s asthma is “well controlled,” the care coordinator will continue to review and monitor the dashboard weekly.
High Tech vs. Low Tech
NEVHC studied three groups of patients:
- Enrollees in the Asthma Control Quality Improvement Initiative: NEVHC enrolled 28 patients in its initiative, where they received health education from the asthma care coordinator plus access to Propeller Health.
- Education Only: An additional 28 patients received asthma education only. They did not use Propeller sensors.
- Usual Care: A third group of 27 patients did not receive any education around asthma control nor Propeller sensors.
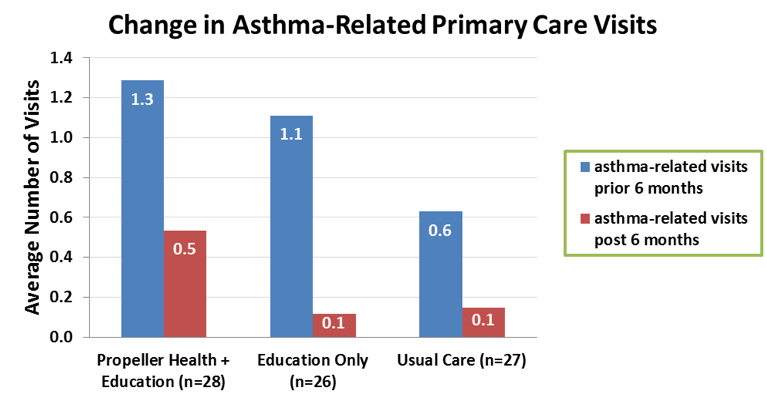
Across all three groups, NEVHC monitored changes in the average number of primary care and ED visits six months prior to the initiative. Then it compared those findings with data from the six months following enrollment.
Primary care visits decreased across all three groups:
The low number of ED visits at baseline (average <1 across three groups) limited NEVHC’s ability to document differences between groups. However, the average number of ED visits decreased across all three groups:
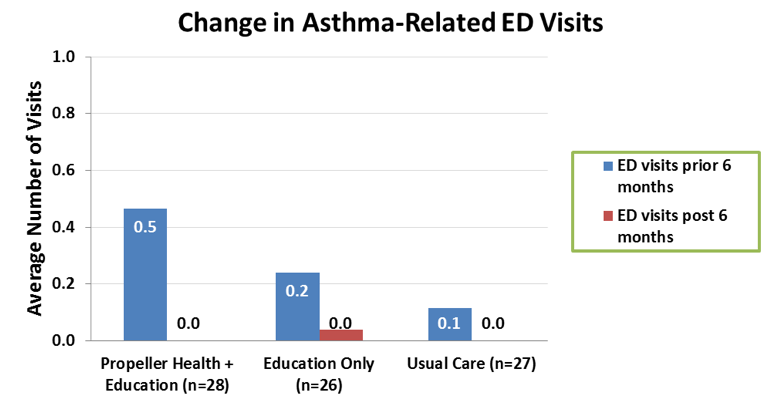
A longer-term review of patient medical records yielded better results: Of the 28 patients enrolled in the initiative, six patients had an ED visit in 2015. Following the initiative, none of the patients had documentation of an ED visit or hospitalization.
Testing Asthma Control Measures
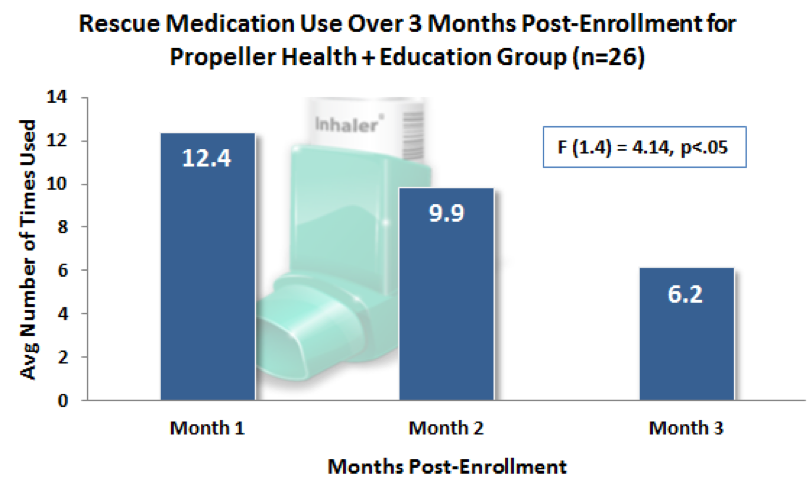
Initiative participants made good strides in improving their asthma control. Over the three-month reporting period following enrollment, the average monthly use of rescue medication decreased:
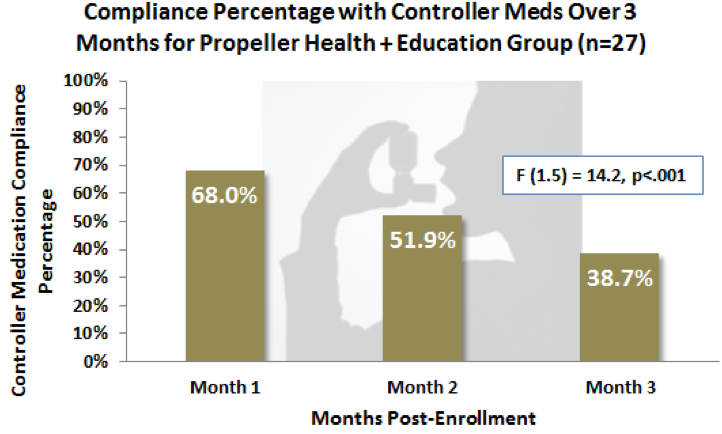
Surprisingly, over the three-month period, the control medication compliance also dropped. It is possible that patients may have decreased use of their control medication if they were feeling better, although it is not clear why this percentage dropped over the post-enrollment period. The US average medication adherence is 22.1 percent.
Transitioning to ‘Well Controlled’
Beyond the initial pilot, NEVHC has continued to deploy Propeller sensors and invite adult patients to asthma education classes at health centers. NEVHC has provided care coordination to more than 184 adult patients and has enrolled 56 patients in to the Propeller Health initiative. A little more than 88 percent of active patients have a status of “well controlled.”
One adult patient had been using his rescue medication daily, but not his control medication because he misunderstood and thought that it should only be used when his “asthma got really bad.” Multiple ED visits and meetings with an asthma care coordinator, where he learned how to properly administer his medications, didn’t change his behavior. He continued to use his rescue inhaler twice a day. In July 2015, he was enrolled into Propeller Health, and in August, his status was “very poorly controlled.” However, in September, he learned that air conditioning was an asthma trigger. With the help of the care coordinator, he was able to mitigate and prevent future flare-ups. By January 2016, the patient reported that he did not need his rescue inhaler at all, but still used his control inhaler twice a day. He is now “well controlled” and has not had any further visits to the ED.
Another success example is a pediatric patient who was not taking his medicine as prescribed, which led to frequent visits to the health center. His mother was extremely frustrated by her son’s forgetfulness. After enrolling into the initiative, the mother was able to better monitor her son’s adherence and remind him to take his medicine as prescribed. The patient is also now in the habit of taking his medicine without his mother’s reminders.
Who Pays?
To deploy this digital solution, NEVHC needed to find a way to pay for the both asthma care coordination and Propeller sensors. In 2015, it won a one-year, $50,000 grant from CVS Health Foundation to launch the initiative. Then, Valley Presbyterian Hospital, a partner hospital, provided $50,000 continue the initiative through 2017. NEVHC is currently working to identify additional sources of funding.
Today, existing staff has been trained to continue this work on a limited basis. Meanwhile, initiative participants continue to use their Propeller sensors, and NEVHC has made more sensors available for a handful of new enrollees.
But payment reform is essential to rolling out this program on a larger scale. NEVHC isn’t getting reimbursed for this initiative because patients are visiting care coordinators, not providers. Clearly the need for payment reform is critical to allow us to sustain efforts that make sense for the patient and the overall health system.
Because the benefits are clear: Propeller reports that its participants have 79 percent fewer asthma attacks, up to 50 percent more doses taken on schedule, and up to 50 percent more symptom free days.
Learn More
- Northeast Valley Health Corporation
- Propeller Health
- An 11-month study by Propeller and Dignity Health found that asthma-related hospitalizations dropped from 1.9 to 0 among 330 patients who had attached sensors to their inhalers. These patients also had 60 percent fewer ED visits.
- Another test in Louisville, Kentucky gave 140 patients Propeller sensors and tracked 5,660 rescue inhaler events over the course of two years. It discovered that proximity to public utilities and railroads were triggers asthma attacks. In addition, public spaces such as educational sites, religious gathering places, metro government sites, and residential courtyards were also associated with higher inhaler use.

