Is a telehealth coordinator essential for sustaining virtual care services?
That was the key question we sought to answer three years ago when we partnered with the
California Health Care Foundation and the
California Telehealth Resource Center to launch a new program,
Sustainable Models of Telehealth in the Safety Net. Our hypothesis was “yes,” but we needed to put it to the test.

To do that, the program funded telehealth staff at nine safety net health centers across California, ranging from Borrego Health in southern California to Chapa-De Indian Health up north. We also provided participants with on-site training, ongoing technical assistance, and a learning community to share best practices so that they could increase access to specialty care for their patients using telehealth.
Fast-forward to today: RAND researchers evaluated the experiences of our participants and
concluded that “with a modest staffing investment, health centers were capable of rapid growth.” Lest that “modest staffing investment” be misunderstood, the researchers spelled it out: the telehealth coordinator made the difference.
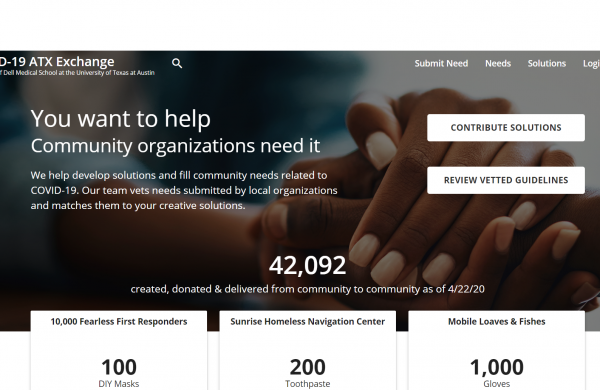
Although the program and this evaluation took place before the COVID-19 pandemic ushered in big changes in the regulation, reimbursement, and use of telehealth services, we think RAND’s findings about telehealth coordinators are still keenly relevant to health centers racing to adapt to our new virtual reality.
Here are three ways that telehealth coordinators play a vital role in implementing and growing successful telehealth programs, according to the RAND study:
1. Telehealth coordinators can free up the time of clinic medical, financial, and operational leadership.
While the scope of the role varies from clinic to clinic, these individuals generally manage the complexities of telehealth visits by overseeing the coordination of multiple staff, patients, space, and equipment. They can ensure that appointments run smoothly, collect data, troubleshoot technology, coordinate referrals, and maintain electronic health records. They can run staff training, keep up with reporting, and network with regional partners. They can even facilitate relationships with vendors and health plans, taking the burden off other staff.
In short, telehealth coordinators can run most aspects of telehealth programs — as long as they get the support and autonomy they need to be effective. One health center leader said they’re “more like a program director than a coordinator.” A telemedicine coordinator agreed, commenting that this position is “the glue” that holds everything together.
2. Telehealth coordinators can develop new policies and procedures to improve telehealth workflows.
The benefits of having a staffer dedicated to telehealth were evident early on. As early as 12 months into the telehealth program, more than half of the health centers reported that they had adopted new policies, procedures, or workflows for telehealth that had been initiated by the coordinator. As telehealth coordinators established open lines of communication with administrative and support staff across departments and clinic locations, they guaranteed that workflows account for variations in staffing, departmental protocols, and clinic capacity. And by the end of the program, many participants praised their coordinators for training medical assistants, referral coordinators, schedulers, and other key staff on improved workflows.
As one health center leader noted, “It has been very helpful to have one person focus on identifying problems at each site and that same person providing all training [or] retraining to ensure consistency.” Another put it more candidly: “If we didn’t have a coordinator to monitor all the complex moving parts, staff and providers would not support this technology due to inherent frustrations.”
3. Telehealth coordinators can engage patients to improve no-show rates.
High no-show rates are costly for health centers. But according to a RAND focus group composed of seven of the clinics’ chief financial officers, telehealth coordinators are a key solution to that ubiquitous problem.
Telehealth coordinators are key players in appointment reminder strategies. One coordinator reported calling patients multiple times per week until she reached them to confirm appointments. Another called patients two days in advance of the appointment, making three to six attempts to reach patients. These live calls — or sometimes a combination of live calls and automated reminders — proved to be more effective than just robo-reminders. Moreover, when patients missed appointments after confirming by phone, the health center could follow up to establish the cause of the no-show and to reschedule.
At the same time, coordinators got to know patients and their personal circumstances. When telehealth coordinators develop those relationships with patients — establishing trust and actively listening to their concerns — they’re able to better educate them about the benefits of telehealth and respond to their concerns or skepticism. Over the course of the program, coordinators experimented with phone calls and letters welcoming new patients, answering questions about telehealth and passing along information about no-show policies. As a result, they reduced the number of missed appointments, thus improving the health centers’ button line.
As one telehealth coordinator put it in an interview that turned out to be prescient, “We’ll only grow. There’s no going back because I mean they’ve absolutely embraced this at our executive leadership level. We’re organization-wide, so that train has left.”
Learn More
Full Research Report:
Issue Briefs:
 To do that, the program funded telehealth staff at nine safety net health centers across California, ranging from Borrego Health in southern California to Chapa-De Indian Health up north. We also provided participants with on-site training, ongoing technical assistance, and a learning community to share best practices so that they could increase access to specialty care for their patients using telehealth.
Fast-forward to today: RAND researchers evaluated the experiences of our participants and concluded that “with a modest staffing investment, health centers were capable of rapid growth.” Lest that “modest staffing investment” be misunderstood, the researchers spelled it out: the telehealth coordinator made the difference.
Although the program and this evaluation took place before the COVID-19 pandemic ushered in big changes in the regulation, reimbursement, and use of telehealth services, we think RAND’s findings about telehealth coordinators are still keenly relevant to health centers racing to adapt to our new virtual reality.
Here are three ways that telehealth coordinators play a vital role in implementing and growing successful telehealth programs, according to the RAND study:
To do that, the program funded telehealth staff at nine safety net health centers across California, ranging from Borrego Health in southern California to Chapa-De Indian Health up north. We also provided participants with on-site training, ongoing technical assistance, and a learning community to share best practices so that they could increase access to specialty care for their patients using telehealth.
Fast-forward to today: RAND researchers evaluated the experiences of our participants and concluded that “with a modest staffing investment, health centers were capable of rapid growth.” Lest that “modest staffing investment” be misunderstood, the researchers spelled it out: the telehealth coordinator made the difference.
Although the program and this evaluation took place before the COVID-19 pandemic ushered in big changes in the regulation, reimbursement, and use of telehealth services, we think RAND’s findings about telehealth coordinators are still keenly relevant to health centers racing to adapt to our new virtual reality.
Here are three ways that telehealth coordinators play a vital role in implementing and growing successful telehealth programs, according to the RAND study: