Pediatrician Maggie Gilbreth applied to the Resilient Beginnings Network to help herself work through frustrations with the healthcare system. “I really just felt something was very broken with how we were treating each other,” says Gilbreth, who takes care of pediatric patients at Zuckerberg San Francisco General Hospital (ZSFGH). “For me, it was really about workplace culture and community. If we can’t treat each other with more compassion and respect, how can we bring those values to our patients and families?”
After her workplace was accepted into Resilient Beginnings Network (RBN), a three-year learning program launched in November 2020, her team has made major strides in practicing healing and trauma-informed care among both patients and team members and finding time for urgently needed connection and support. As she notes, “It’s not just how much work you do; it’s how you show up for the work…We need to radically re-envision ourselves.”
Gilbreth and her team are one of 15 safety net organizations in the San Francisco Bay Area that participated in the Resilient Beginnings Network, led by the Center for Care Innovations with funding support from Genentech Charitable Giving. This spring the Center for Community Health and Evaluation (CCHE) released its final evaluation report, which found the program successful in its long-term efforts to shift the broader clinic culture to be more trauma-and-resilience-informed in its approach to patients and each other.
The teams could choose their entry points into the program in one of four domains, although they were free to expand their work in all of them. The three cross-cutting themes in all the domains were equity and racial justice; strength-centered approaches, and patient and family engagement.
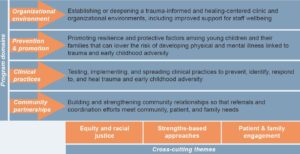
From the CCHE final report on the Resilient Beginnings Network
Evaluators concluded that RBN made considerable progress in using screening for adverse childhood experiences (ACEs) as a point of entry to a healing culture and elevating staff and provider well-being during a time of nationwide trauma and climate disasters. As one participant told the evaluators, “You’ve got to start with your caregivers, resource your caregivers. Because if you want them to be able to pour into your patients you’ve got to pour into them first.” CCHE also found that RBN had shifted the broader clinic culture to be more trauma-and-resilience-informed and expanding clinics’ understanding of the connections between equity, racial justice, and trauma-informed care.
The evaluators also reported that RBN’s flexible approach in meeting teams where they are, as well as the 3-year program timeline, allowed teams to apply their new knowledge and take advantage of emerging opportunities. “That was incredible,” one participant said. “To have a grant that gave us space to try what we needed, where the expectations were very flexible was such a gift. It’s one of the best things I’ve ever done.”
To learn more, read the executive summary here.
And find out more from CCHE’s entire RBN Final Report here.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.