Juliane Tomlin
 VOICES FROM THE FIELD: INNOVATING DURING THE COVID-19 CRISIS
VOICES FROM THE FIELD: INNOVATING DURING THE COVID-19 CRISIS
In the face of the COVID-19 crisis, health care organizations and providers everywhere are faced with a massive shift in care delivery priorities. Determining how to continue providing care to patients with chronic conditions, who have an increased risk for contracting COVID-19, is a challenge. We put some questions to two experts at Kaiser Permanente’s Southern California Permanente Medical Group, whose Community Benefit department funds Transforming Cardiovascular Care in Our Communities:
- Dr. Timothy Ho, Regional Assistant Medical Director for Quality and Complete Care
- Dr. Jeffrey Brettler, Area Assistant Medical Director Emeritus, West Los Angeles, Physician Co-lead for Hypertension
Check out our webinar with Drs. Ho and Brettler to learn more about their approach and lessons learned to date.
How is Kaiser Permanente prioritizing care for different patient needs related to chronic conditions?
 Dr. Timothy Ho:
Dr. Timothy Ho: To protect patients and staff, we have postponed all routine and lower risk services that require patients to come to facilities for face-to-face encounters. Though patients are still coming in for curbside pick-up of pharmacy and also for drive-through COVID-19 screening.
We screen patients who contact us for appointments to see whether or not their issue can be resolved remotely. For the small subset who do need to be seen in person, we ask medical centers to try to complete as many services as possible at the encounter — A1c, blood pressure, cervical cancer screening, medication adherence, foot exams — with a few exceptions. Specifically:
- For blood pressure checks and A1c tests, we have postponed routine checks for the time being, but have sent guidance to all of our medical centers that they should be reaching out to their patients with the highest risk. For example, we need to be talking to patients with the highest recent readings on blood pressure or A1c. We have sent them patient reports sorted by risk level and advised them to start at the top. For patients who are symptomatic — either whom we see in person, or virtually if they are able to take their own blood pressure — we prescribe additional treatment such as medication titration, an emergency department visit, or follow-up.
- For retinal exams, we have postponed all screening exams. We have considered China's experience where many COVID-19 cases were most likely transmitted during eye exams where the examiner and patient were very close
- We have been completing medication titration and coaching over the phone or video.
- Foot exams are only completed if a patient is in clinic.
- Regarding cancer screening, radiology has postponed most non-emergency or routine studies. Mammography has postponed most routine screenings and we have stopped outreach to patients due for routine screening mammograms. Cervical cancer screening is being conducted for patients who are due when they are being seen at a face-to-face encounters. No outreach for routine screening is being done at this time. For colorectal cancer screening, home FIT kits have been the backbone of screening and will continue without interruption. If anything, that program will be augmented or supplemented. Routine screening colonoscopies have been postponed, but symptomatic colonoscopies are moving forward. Colonoscopy as a procedure requires the use of PPEand judicious use of PPE is a priority during this COVID-19 pandemic.
Could you provide some more specifics about how you are prioritizing and following up with patients with hypertension?
 Dr. Jeffrey Brettler:
Dr. Jeffrey Brettler: We continue to stress “do what’s right for the patient.” The activity we have prioritized won’t necessarily help our HEDIS numbers but it will be lifesaving for patients. Our highest risk patients need the continued and urgent support of our Complete Care [population care] and primary care teams. This work can’t stop because of the crisis, but it should be modified.
We’re running periodic reports for patients with last blood pressure in severely elevated range: > 180/110 and > 200/120. These are two significant thresholds. The lower threshold defines “severe hypertension,” which generally requires face-to-face follow-up in days, not weeks. The higher threshold is for “hypertension urgency,” as defined in our system, though you’ll see different definitions for this. This latter group has a very significant short-term risk: the number needed to treat (NNT) of 2.6 for morbid events at 11 months (
Veterans Administration Cooperative Study).
For the highest risk, or “hypertension urgency,” members:
- We’re establishing a standard workflow at all medical centers through a regional webinar. We ask local hypertension teams to outreach to all patients ASAP telephonically and ascertain if the patient has a home blood pressure monitor. If not, they should inquire if interested and able to participate in remote monitoring program; then if so, send them a remote monitor. If the patient already has a home blood pressure monitor, we adjust the medication and schedule a telephone follow-up.
- Note that some medical centers have decided to do some limited in-person blood pressure checks for follow-up of > 180/110. We left this up to the discretion of the medical center, but reinforced that all patients need contact and follow-up.
- Our current remote monitoring pilot involves four medical centers.
- The nine centers not involved in pilot have agreed to start program, with these patients as first priority. Enrollment is being done virtually, which will be challenging as all prior enrollment in pilot sites was done face-to-face. We recently held a second regional webinar to review remote monitoring process with these nine centers.
- Blood pressure monitors are to be distributed to local medical centers, based on size of > 180/110 population. Our medical centers will ship monitors to patients.
- There’s a strong interest in video visits to ensure adequate blood pressure measurement competency, as initial feedback from calls raised this concern. KP has a new video platform — HealthCare Anywhere — which facilitates on-the-spot video visit.
- There’s also interest in pushing out short blood pressure competency video in addition to our usual written and on-line handouts.
For the lower risk, or “severe hypertension,” members:
- The expectation is that these lists are worked on after severely elevated blood pressure ranges are taken care of.
- This is happening in a variety of ways based on local Complete Care [population care] infrastructure, including use of RN protocol, NPs, and pharmacists who were previously doing this work face-to-face.
- There are competing priorities as some Complete Care departments are now tasked with managing COVID-19 test results. There is some opportunity with primary care nursing, as essentially all primary care physician visits are now telephonic or video.
- Some centers have created waitlists for these patients to return in six to eight weeks; others will generate usual reports once this public health crisis is resolved.
We put some questions to two experts at Kaiser Permanente’s Southern California Permanente Medical Group.
In the face of the COVID-19 crisis, health care organizations and providers everywhere are faced with a massive shift in care delivery priorities. Determining how to continue providing care to patient…
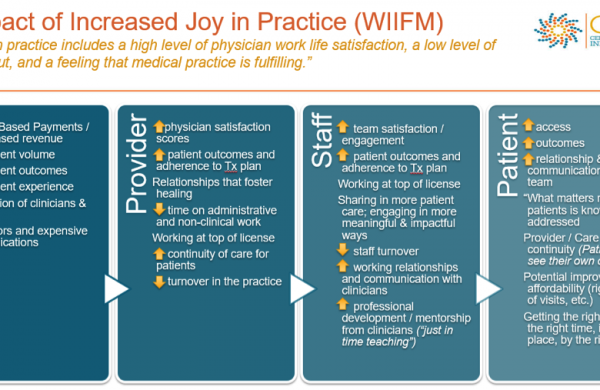
It’s only when we take the time to understand the readiness for transformation that we can offer the most effective support.
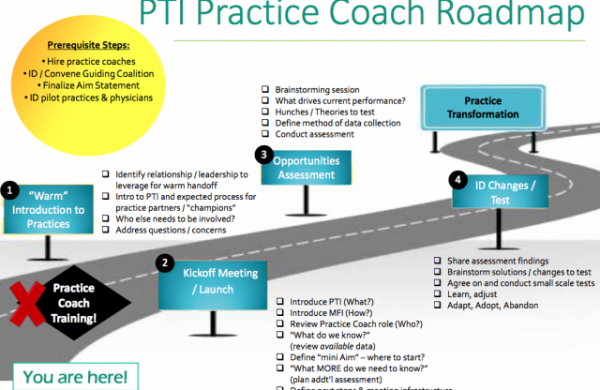
Senior Improvement Advisor Juliane Tomlin shares how to nurture the development of 4 key learning attributes, so we can better navigate today’s uncharted waters.
CCI’s Senior Improvement Advisor lays out how to make the case for these vital transformations, and how to do it when you are ready.
CCI’s senior improvement advisor walks through the different stages of coaching through practice transformation.
 VOICES FROM THE FIELD: INNOVATING DURING THE COVID-19 CRISIS
VOICES FROM THE FIELD: INNOVATING DURING THE COVID-19 CRISIS Dr. Timothy Ho: To protect patients and staff, we have postponed all routine and lower risk services that require patients to come to facilities for face-to-face encounters. Though patients are still coming in for curbside pick-up of pharmacy and also for drive-through COVID-19 screening.
We screen patients who contact us for appointments to see whether or not their issue can be resolved remotely. For the small subset who do need to be seen in person, we ask medical centers to try to complete as many services as possible at the encounter — A1c, blood pressure, cervical cancer screening, medication adherence, foot exams — with a few exceptions. Specifically:
Dr. Timothy Ho: To protect patients and staff, we have postponed all routine and lower risk services that require patients to come to facilities for face-to-face encounters. Though patients are still coming in for curbside pick-up of pharmacy and also for drive-through COVID-19 screening.
We screen patients who contact us for appointments to see whether or not their issue can be resolved remotely. For the small subset who do need to be seen in person, we ask medical centers to try to complete as many services as possible at the encounter — A1c, blood pressure, cervical cancer screening, medication adherence, foot exams — with a few exceptions. Specifically:
 Dr. Jeffrey Brettler: We continue to stress “do what’s right for the patient.” The activity we have prioritized won’t necessarily help our HEDIS numbers but it will be lifesaving for patients. Our highest risk patients need the continued and urgent support of our Complete Care [population care] and primary care teams. This work can’t stop because of the crisis, but it should be modified.
We’re running periodic reports for patients with last blood pressure in severely elevated range: > 180/110 and > 200/120. These are two significant thresholds. The lower threshold defines “severe hypertension,” which generally requires face-to-face follow-up in days, not weeks. The higher threshold is for “hypertension urgency,” as defined in our system, though you’ll see different definitions for this. This latter group has a very significant short-term risk: the number needed to treat (NNT) of 2.6 for morbid events at 11 months (Veterans Administration Cooperative Study).
For the highest risk, or “hypertension urgency,” members:
Dr. Jeffrey Brettler: We continue to stress “do what’s right for the patient.” The activity we have prioritized won’t necessarily help our HEDIS numbers but it will be lifesaving for patients. Our highest risk patients need the continued and urgent support of our Complete Care [population care] and primary care teams. This work can’t stop because of the crisis, but it should be modified.
We’re running periodic reports for patients with last blood pressure in severely elevated range: > 180/110 and > 200/120. These are two significant thresholds. The lower threshold defines “severe hypertension,” which generally requires face-to-face follow-up in days, not weeks. The higher threshold is for “hypertension urgency,” as defined in our system, though you’ll see different definitions for this. This latter group has a very significant short-term risk: the number needed to treat (NNT) of 2.6 for morbid events at 11 months (Veterans Administration Cooperative Study).
For the highest risk, or “hypertension urgency,” members: