This is a time of incredible transformation in health care, and the organizations that care for our most vulnerable patients can lead the way. In 2016 the Public Healthcare System Evidence Network and Innovation Exchange, supported by Blue Shield of California Foundation, did a systematic literature review searching for a model to promote innovation and the spread of proven innovations in the safety net.
Safety Net Systems Are Ripe for Innovations, But Barriers and Gaps Remain
Safety net systems are skilled in adapting and reinventing innovations to fit them into organizational goals and priorities. The community engagement practiced by many safety net systems gives these organizations the ability to bring patients, clinic staff and leadership into the mix, strengthening the implementation or development process.
These systems, in partnership with diverse change agents, have also been effective at disseminating innovations. In part this is due to the powerful mission and values shared across many health centers. These shared values create strong peer networks, which promote inter-organizational norms that make the safety net a great place for innovative practices to spread quickly.
However, safety net organizations are always tight on staff, time and money, and may struggle to dedicate enough resources to complete an innovation project quickly and effectively. They may not be able to do the labor-intensive monitoring required to provide regular feedback during the innovation process. Leadership focus, staff turnover, fiscal solvency, regulatory environment—all of these are more up for grabs in the safety net, and this can impede innovation.
Furthermore, knowledge gaps meant that safety net systems weren’t always able to properly determine innovation-system fit, or do effective pre- and post-implementation assessment.
The Greenhalgh Model: How to Think About Innovation in the Safety Net
Given these opportunities and challenges, it’s vital for the safety net to begin thinking about innovation in a systematic way. Guided by seven elements, the Greenhalgh Model provides a rubric to evaluate an innovation in conjunction with the variables that impact an innovation’s outcome and sustainability. Notably, these variables address both the innovation itself and the environment for which it is implemented.
The innovation: This construct covers the aspects of the innovations itself such as the advantage of the innovation over the status-quo, if the innovation can be tested, and the technical support required to implement the innovation.
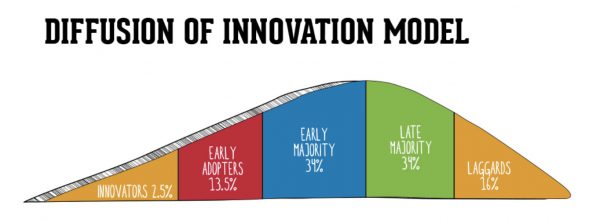
Communication and influence: These relate to how an innovation is diffused or disseminated once the innovation is implemented.
Outer context: The external organizations, environment, policies, and climate that affect the implementation and spread of an innovation.
Implementation process: The factors affecting the implementation of an innovation, such as training, resources, communication and feedback.
Assimilation: The ways in which the adopting team or department changes in order to implement the innovation.
System readiness for innovation: Aspects that affect how amenable the system is for a specific innovation.
System antecedents for innovation: More static characteristics that affect how effectively the system will be able to innovate.
What are the Takeaways for Health Centers?
- Focus on pre-implementation assessment and observation to make sure you have the resources and organizational health to implement the innovation. Try a checklist to assess your readiness for an innovation
- Don’t be afraid to create new protocols to support an innovation. Not every solution can be dropped into your system as-is.
- Make sure decide in advance how you will measure the effects of the innovation you are putting in place—both positive and negative. Try to be very detailed in your documentation of the implementation process, so you can tell if you were able to fully implement an innovative process as planned.
- Do in-depth post-intervention evaluations that assess the net impact of the innovation and how outside factors affected the process. Evaluate innovations using a framework that captures this impact more comprehensively than a standard assessment of efficacy.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.