Although one in four visits to primary care providers (PCPs) in community health centers (CHCs) result in a specialty referral, CHCs often struggle to obtain specialty access for their patients.
The paucity of specialists willing to care for CHC patients leads to major imbalances in supply and demand. Wait times for patients to obtain specialty appointments can be as long as one year, with potentially life-threatening implications, including disability, chronic disease complications and death. Poor access to specialty services contributes to known racial/ethnic health disparities. Even when referrals are made, about 30% of CHC pediatric patients never receive the needed service, with a range of 10-73% depending on specialty6. Similar findings have been reported for adult CHC populations.
These challenges for CHC patients do not affect only those who are uninsured. Medicaid patients are less likely than privately insured patients to receive needed specialty care. As mentioned earlier, some specialists are not willing to accept patients with Medicaid due to low payment rates, and Medicaid patients are more likely than privately insured patients to miss appointments because of transportation, childcare, language or other barriers. In some situations, patients can access specialty services through safety net hospitals committed to caring for patients irrespective of payer source (public hospitals, some academic centers, critical access hospitals), but more often than not, demand exceeds the supply of specialists.
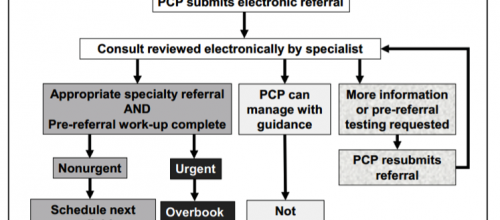
In our full report, we described a number of strategies to secure access to specialty care and ensure effective integration between primary and specialty care through comprehensiveness or coordination. Many of the innovations described overlap multiple domains.