A Call to Action
In 2015, Livingston Community Health embarked on a journey to better serve its community. The question that had been nagging leadership for some time was, “How can we serve more than just the patients who walk through our doors?” Livingston’s growing patient population is culturally and linguistically diverse. The majority of patients are poor with 65 percent living at or below the federal poverty level and 65 percent covered by Medicaid. Although reductions in the uninsured have improved over the years, today 15 percent are still uninsured. Employing a multilingual workforce with bilingual proficiency in Spanish is essential to serving 55 percent of patients who speak a language other than English.
Understanding this context was a key factor in why the largest local employer in Merced County reached out to a number of health centers in the area in search of a local health care partner. Foster Farms also has a culturally and linguistically diverse workforce. At their Livingston site there are 3,200 employees, a majority of which work in assembly line manufacturing. Forty three percent speak Spanish. Punjabi, Hmong, Portuguese, and Assyrian are also spoken on factory floors. Many of the employer’s attempts at providing preventative services, such as an annual biometrics screening, went underutilized. Having established elements of an employee wellness program in the past, including a “nurse line,” Foster Farms wanted to try a more localized and personalized approach. There were avoidable tragedies, like when one employee went more than a decade without any preventative screening only to one day, while at work, be sent to the hospital in an ambulance on the verge of a heart attack.
To Foster Farms, supporting the health of their employees is good business. In 2014, the company had spent more than $15 million on employee health utilization costs at the Livingston site. During this time, 35 percent of costs were associated with 1 percent, or 60 members; while another 8 percent, or 450 members, accounted for 18 percent of costs. (These numbers might sound familiar to those who have experience with the Institute for Healthcare Improvement’s Triple Aim, which has shown that 1 percent of the high-risk patients account for 25 percent of healthcare spending and 5 percent account for 50 percent of spending.)
A healthy workforce is a more productive workforce, and the case for prevention becomes tied to a reduction in health insurance claims.
A New Approach
Foster Farms has worked with numerous wellness vendors over the years. With more than 12,000 employees spread across 12 sites in six states, it realized they needed to try something different to establish a long-term investment in the health for its workforce. The company’s fundamental question was, “How might partnering with a local health center help improve health and health outcomes and drive down the cost of care for our employee population?”
Livingston Community Health was the only health center that responded to Foster Farms’ call for local partners to discuss a local partnership for employee wellness. For Livingston Community Health, numerous factors played into a successful match: a concerted focus on preventative care, an understanding of population health management, an opportunity for innovation, and a changing landscape for future reimbursement.
With the Triple Aim in mind, Livingston Community Health designed a population health management program with an ambitious three-pronged approach that was responsive to the employer’s health care utilization trends:
- Treat those who are the sickest with case management services.
- Treat those who may benefit from early intervention with disease management services.
- Treat those who could benefit from preventative education with health promotion/health education services.
Laying the Foundation
Felicia Batts, Director of Care Integration at Livingston Community Health, is no ordinary change agent. She has decades of clinical and administrative experience in health care, a public health graduate degree, and an entrepreneur’s mindset. Literally thinking outside the box, one of her first assignments was to figure out how Livingston Community Health could work with a large local school district to support students and their families, as well as how to work with Foster Farms, a large local employer, to support their employees and dependents. Felicia had the full support of Livingston Community Health CEO Leslie McGowan to work on strategic projects, and she had the space and time to engage with Foster Farms to come up with a plan that aligned incentives and delivered value to residents of the community.
Felicia describes the days leading up to the Employee Wellness Program pilot as both “intense” and “low risk.” She noted, “Everyone was at the table not knowing exactly how things would work out and felt like we had nothing to lose by running the pilot. Felicia spent nine months in the planning phase before the pilot launched. It required her to get very specific as to what exactly the key elements of the Employee Wellness Program were and how it would all work. Felicia recalls that “there was no blueprint or roadmap for what we were attempting.”
During this time, Felicia had the opportunity to submit a grant proposal on the program, forcing her to “articulate the concept in detail and really break it apart into manageable chunks.” While, Livingston Community Health did not get the funding, Foster Farms was still interested in making the upfront investment with a two-year contract to pilot the program.
Tracking Change
Brett Kirkham is Foster Farms Corporate Treasurer and manages the company’s Benefit Programs. Brett and the Foster Farms leadership team is committed to making investments even though the return might be unknown, creating space and time for that trial and error.
Though the metrics they were tracking were very specific from the outset. At the beginning of each year, Brett and his team would isolate certain areas of interest that are known cost drivers. For example, one year they looked at hospital stays. Referencing county, state, and national averages as benchmarks they compared the hospital stay numbers of their employee population. They could then look closer at the prevalence of a particular chronic disease, like diabetes or asthma.
Brett and his team continued these annual reviews during the planning and implementation phase of the pilot — using a combination of data from vendors including a national wellness company, a biometrics company, the company’s health insurance provider, and a local health care provider. In the end, Foster Farms and Livingston Community Health were able to prioritize, design, and implement health promotion strategies and disease management efforts (e.g.asthma prevention, diabetes education etc.) that are unique and relevant to the employee population at a specific site.
The Cornerstone
Liliana Velasco wanted to walk out crying after her first few days on site at Foster Farms. Three years ago, she was the first Employee Wellness Manager hired by Livingston Community Health and stationed at Foster Farms. She did not know where the break rooms were located. The employees at Foster Farms thought she and Felicia were undercover agents trying to collect sensitive information about employees. Liliana knew from the beginning that she might not be “loved and liked by everybody.” She spent the first few weeks doing her paperwork in her car. Not having a chair and desk were the least of her problems. It took Liliana six months to gain the trust of the employees at Foster Farms. When asked how she did it, her response is very matter of fact: “I kept showing up, I kept smiling.”
On building trust Liliana adds: “I remember small things about people’s personal life and I follow up with them next time I see them.” Her experience as a Clinic Site Manager and training as a Health Coach with and in Motivational Interviewing have created foundational skill sets for her work. Felicia, who Liliana refers to as her “backbone,” describes Liliana as “a people person — patient, reliable, trustworthy, a great communicator, super independently functioning.” In addition to the weekly check-in calls that persist to this day, Felicia spent two months before the launch of the pilot training Liliana in what she describes as a “mini degree in public health.”
Employee Wellness Manager Training Checklist:
✔️ Data Review: County Health Outcomes Data
✔️ Data Review: Employee health utilization data
✔️ Industry Framework: Triple Aim model (health outcomes, patient experience, per capita costs)
✔️ Population Health Management: Non-primary care intervention efforts
✔️ Behavior Change Framework: Motivational interviewing and communication skills
Surrounded by hundreds of people every day at Foster Farms, Liliana says that “personality is huge” and being a “people person is critical.”
As the solo representative for Livingston Community Health at Foster Farms, she has effectively evolved the Employee Wellness Manager role to one of an educator and a connector. Not being a nurse or physician herself has not been an obstacle. When faced with a question about labs or medications she cannot provide clinical services, but she can connect employees to nurses back at her health center for Livingston Community Health patients, the part-time nurse onsite, or the employee’s medical home for coordinated care.
Year one of the two-year pilot was about getting a better understanding of the workforce. In the early days, Liliana was surprised by the lack of understanding employees had about their health insurance coverage and other benefits. It was not uncommon, for instance, to find employees who suffered from asthma who did not know that their inhalers were100 percent covered by their health insurance. Or employees not testing their blood sugar because they were “saving” their strips and didn’t know that these supplies were fully covered by insurance. These educational opportunities opened up more conversation about the importance of preventative care — maximizing health benefits and self-management.
It was not until the end of that first year that Felicia, Brett, and Liliana felt that the pilot had finally stabilized and they started to see positive results. These signs included:
- Program recognition.
- Employee interest in learning and making lifestyle changes.
- Employees seeking out the Employee Wellness Manager and confiding in her about their personal and family health issues.
Year two of the pilot was about driving awareness of additional programs, such as free preventative prescription coverage and annual biometric screening exams. Getting a baseline on the needs around chronic disease management enabled the team to develop tailored programming to meet employee’s health needs.
Today, the program offers three main services:
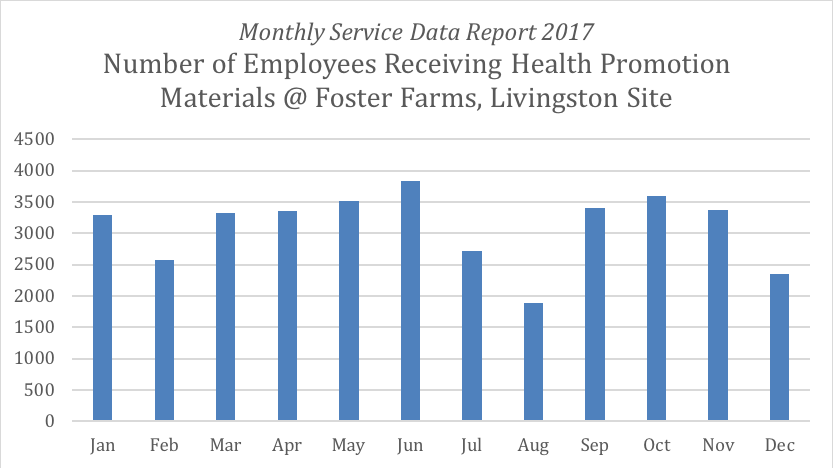
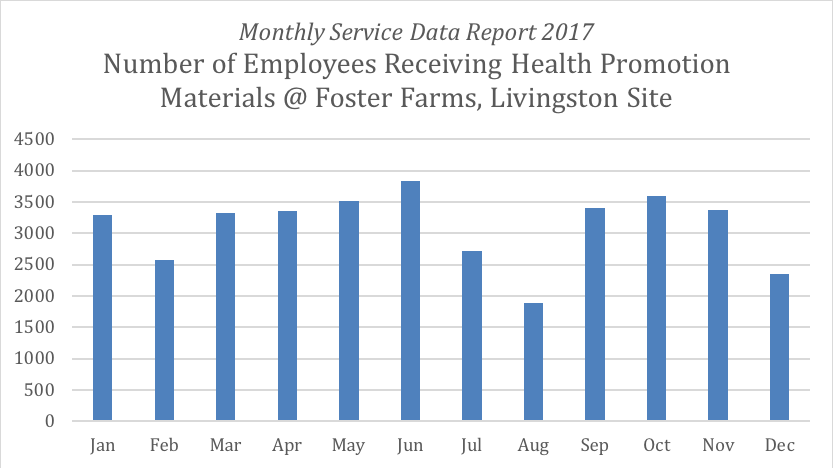
- Health Promotion Services, which include monthly health topics reviewed with 1,200+ employees across seven departments each month.
- Disease Management Services, which include a 22-week health education program utilizing an evidence-based curriculum that includes weekly classes for employees with pre-diabetes.
- Case Management Services, which are being planned to identify high-risk high cost claimants (e.g. employees, spouses, dependents) and design a clinical support compliment.
Before the pilot launched, Liliana aimed to see 400 employees per month. Today she has 3,300 interactions per month, of which 1,257 are unique visits.
For the past 18 months Liliana has been running monthly health promotion sessions. Last month, it was hypertension awareness. Earlier in the year, it was diabetes prevention. Asthma is an upcoming topic.

About her role she says, “it’s a lot of educating and a lot of explaining.” She wears a Livingston Community Health Polo Shirt and Badge every day to continue to distinguish her role at the Foster Farms sites. She remains mindful to discuss only health related topics and stays away from addressing Foster Farms-related business. This separation is important because these days, while there are still some people who are suspicious and do not engage, hundreds of employees now confide in her daily. They tell her that when Liliana is onsite with them it’s their “happy time.”
A Happy Surprise
Both partners recognized a boost in employee morale, an unanticipated outcomes of the pilot program. What started out as case management, disease management, and health promotion services resulted in not only an increasingly health conscious workforce but also a happier one.
For Livingston Community Health, this experience has created excitement around additional opportunities to design and expand health care services outside of its four walls. For Foster Farms, this low-risk experiment confirmed investing in local community partnerships is worth replicating at additional sites.
The adventures of these partners continue with Livingston Community Health needing to increase staffing and build capacity to respond to the demand for adding this program to new Foster Farms sites.
Beyond the Four Walls
How can innovative approaches in health care help to advance the health and well-being of all people? How can community health centers and large employers mutually benefit from health care partnerships? How would more community collaborative efforts advance health outcomes, create positive health experiences, and drive down costs?
Thinking “outside the box” is not a reimbursed service in health care today, but there is a business case for working outside of a clinics four walls. Health care organizations today must prepare for a future of “value driven care” one that is reimbursed for good and improved health outcomes rather than the number of visits a day. All employers want to run productive and profitable operations, making investments in their employee’s health and wellness essential to achieving those goals.
Interested in learning more about this project or how to test it in your organization? Contact Felicia Batts, Director of Care Integration at Livingston Community Health.
Get In Touch