With the rapid expansion of telemedicine in light of the COVID-19 pandemic, ensuring that remote care reaches diverse, low-income patients and promotes health equity, rather than exacerbating health disparities, is critical. Through a partnership between the Center for Care Innovations, UCSF’s Center for Vulnerable Populations (CVP), and the Commonwealth Fund, we have developed this toolkit to provide background information as well as concrete guidance relevant to safety-net healthcare systems looking to initiate, expand, or improve their telemedicine programs.
This toolkit focuses on telemedicine, which the Health Resources Services Administration defines as referring to remote clinical services such as phone and video visits, remote patient monitoring, patient portals, and mobile health.
The toolkit was originally published in October 2020 and was refreshed in June 2021. In the June 2021 refresh, we have added new evidence regarding equity in telemedicine uptake among diverse patient populations, as well as new resources regarding reimbursement. In addition, we have integrated “Tools from the Field” — scripts, workflows, and other concrete tools from safety-net healthcare sites participating in CCI’s Connected Care Accelerator. We hope that sharing these concrete tools will help to disseminate best practices and inspire continued testing and improvement of telemedicine programs as sites adapt these resources to meet their on-the-ground needs.
In addition to this more action-oriented toolkit, we have also expanded upon CCI’s COVID-19 Resource Wiki with information-oriented resources from our research.
If you find that we have missed a key resource on telemedicine implementation in safety-net healthcare settings, please let us know by sending an email to [email protected].
Toolkit Navigation
![]()
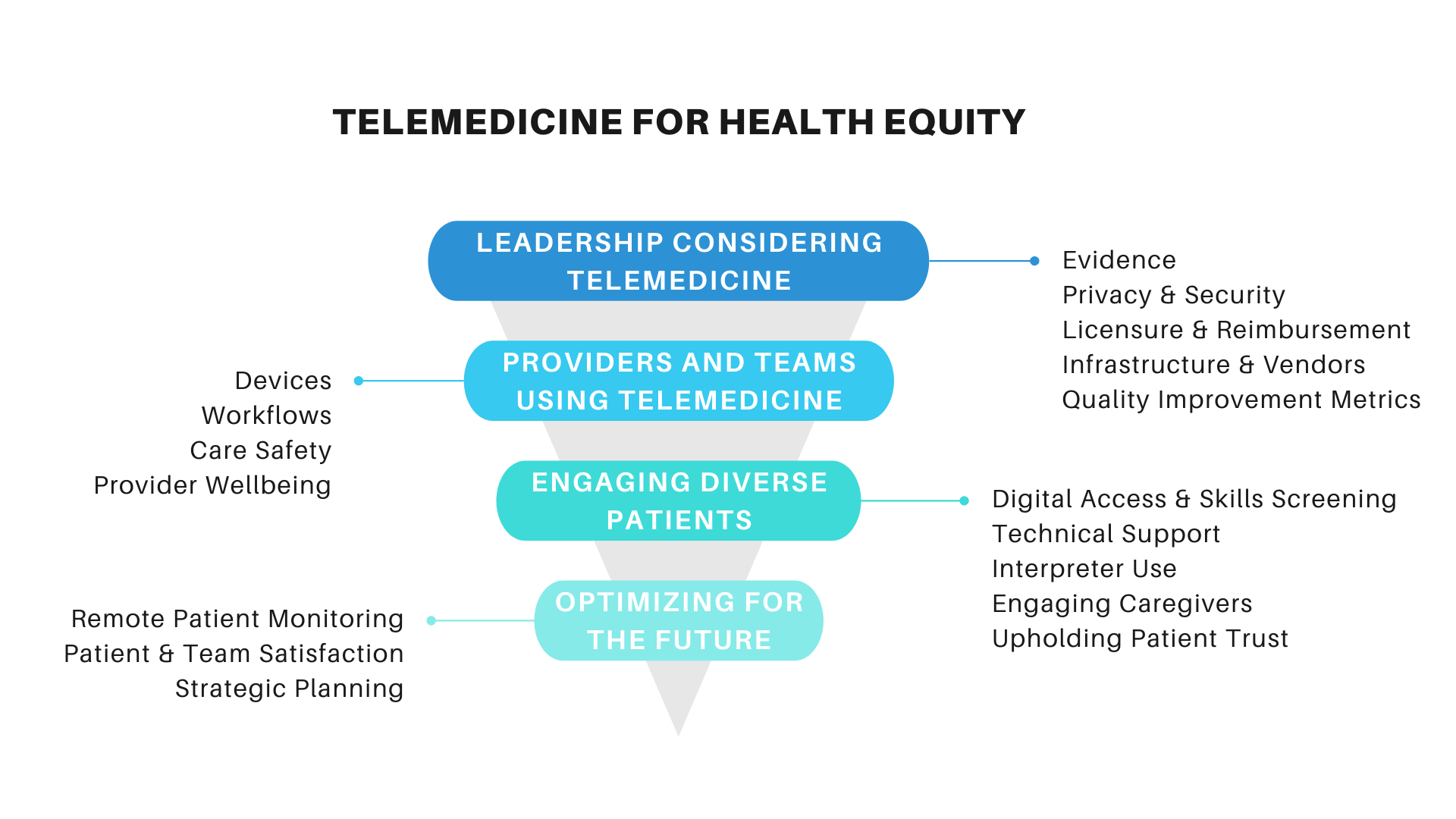
Considerations for Leadership Before Implementing Telemedicine
The COVID-19 pandemic prompted health care providers and systems to rapidly adopt and expand telemedicine services. Telemedicine provides a safer alternative to in-person visits during the pandemic, but simultaneously introduces multiple decision points for implementation.
While many providers already have telemedicine in place, emerging evidence, policies, and guidance on implementation and maintenance indicate that answers to the question, “how do we implement telehealth equitably, safely, and sustainably?” are very much still evolving. In this chapter, we summarize many of the basic components of telemedicine implementation for health care system leaders, including:
- Evidence for implementing telemedicine,
- Risks, privacy and security,
- Reimbursement,
- Vendor selection, and
- Performance measurement.
Considerations for Providers and Teams in Using Telemedicine
Once the decision to integrate telemedicine into routine care delivery is made, frontline care teams must begin to deliver telemedicine efficiently, safely, and equitably.
The key considerations for frontline teams include:
- Provider and team devices,
- Developing telemedicine visit workflows,
- Ensuring care visit quality and safety, and
- Supporting staff and team well-being.
![]()
Considerations for Reaching and Engaging Diverse Patients
Central to effective and equitable implementation of telemedicine care is engaging a diverse patient population.
Some of the most pressing areas of consideration to ensure telemedicine does not worsen existing health disparities include:
- Understanding patients’ digital access and skills,
- Connecting patients with technical support,
- Integrating interpreters into remote/virtual visits for those with limited English proficiency,
- Engaging patients’ caregivers and additional support services and teams, and
- Building a foundation of trust between patients and providers.
Optimizing Telemedicine for the Future
As we continue to scale telemedicine approaches in the COVID-19 pandemic and beyond, there will be many advanced features that can be implemented and optimized for safety-net settings, including remote patient monitoring, assessing patient and team satisfaction, and population health management.