The COVID-19 pandemic prompted health care providers and systems to rapidly adopt and expand telemedicine services. Telemedicine provides a safer alternative to in-person visits during the pandemic, but simultaneously introduces multiple decision points for implementation.
While many providers already have telemedicine in place, emerging evidence, policies, and guidance on implementation and maintenance indicate that answers to the question, “how do we implement telehealth equitably, safely, and sustainably?” are very much still evolving. Here, we summarize one of the many of the components of telemedicine implementation for health care system leaders. This is particularly important in safety-net settings that already face challenges related to limited resources and fragmented health information technology.
The Centers for Medicare and Medicaid Services (CMS) and other payers have changed reimbursement policies in response to COVID-19. Further, licensure requirements for telemedicine vary from state to state. The resources below provide information about new telemedicine billing, coding, and licensure policies that are relevant for safety net hospitals and clinics during the pandemic.
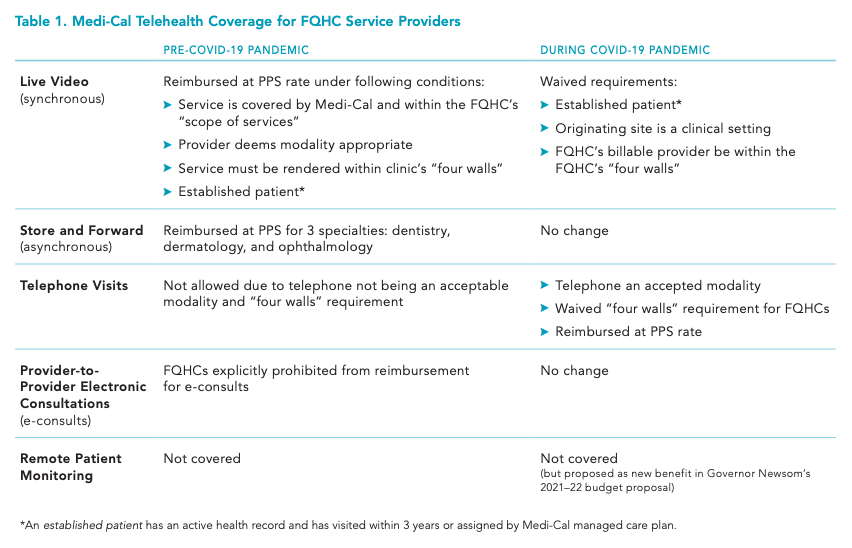
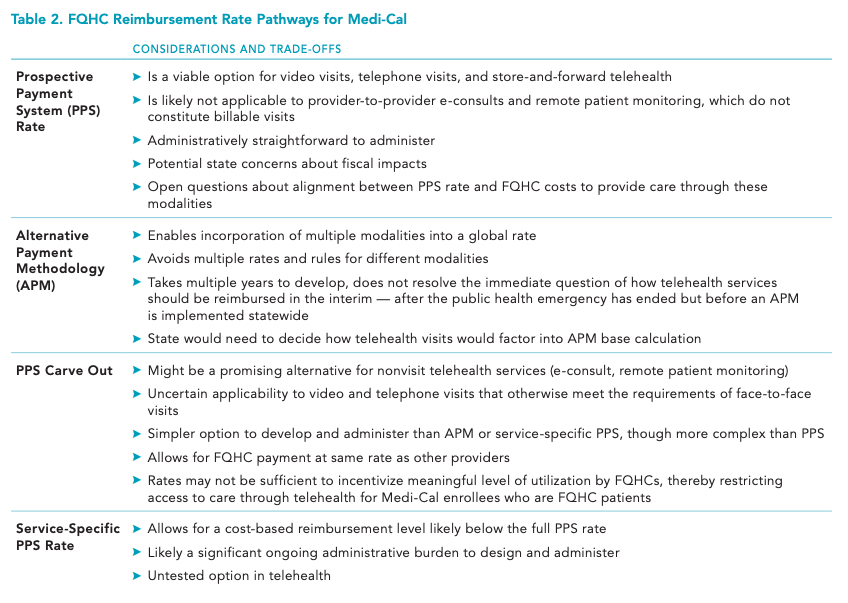
- California Health Care Foundation: Reimbursing FQHCs for Telehealth Post-COVID-19 Pandemic – Medi-Cal’s Option — This report outlines policy options for California policymakers to consider as they determine the future of telemedicine reimbursement for FQHCs under the state’s Medicaid program, Medi-Cal. It also discusses how other states have approached Medicaid coverage for telemedicine, including both video and phone visits as well as e-consults and remote patient monitoring.
Resources from the Centers for Medicare & Medicaid Services:
- New and Expanded Flexibilities for Rural Health Clinics (RHCs) and Federally Qualified Health Centers (FQHCs) During the COVID-19 Public Health Emergency (PHE) — This PDF has information about billing and coding policies for rural health clinics and federally qualified health centers during the COVID-19 pandemic. It includes sections on claims requirements, payment rates, cost reporting, cost-sharing, and more.
- COVID-19 Frequently Asked Questions (FAQs) on Medicare Fee-for-Service (FFS) Billing — This PDF has answers to frequently asked questions about Medicare fee-for-service billing related to COVID-19. The sections on “Expansion of Virtual Communication Services for FQHCs/RHCs” beginning on page 53 and “Medicare Telehealth” on page 59 are particularly relevant.
- Covered Telehealth Services for PHE for the COVID-19 Pandemic — This resource has a list of services payable under the Medicare Physician Fee Schedule when furnished via telehealth. A zip file of covered telehealth services during the COVID-19 public health emergency is available to download on the webpage.
Resource from the Center for Connected Health Policy:
- COVID-19 Related State Actions — This webpage has a continually updated database of COVID-19 related state actions taken by each state’s Office of the Governor, Medicaid Program, Medical Board, and/or Department of Insurance regarding licensure and telemedicine and their current status.