The COVID-19 pandemic prompted health care providers and systems to rapidly adopt and expand telemedicine services. Telemedicine provides a safer alternative to in-person visits during the pandemic, but simultaneously introduces multiple decision points for implementation.
While many providers already have telemedicine in place, emerging evidence, policies, and guidance on implementation and maintenance indicate that answers to the question, “how do we implement telehealth equitably, safely, and sustainably?” are very much still evolving. Here, we summarize one of the many components of telemedicine implementation. This is particularly important in safety-net settings that already face challenges related to limited resources and fragmented health information technology.
Quality and Effectiveness. There is a considerable body of evidence supporting the quality and effectiveness of telemedicine interventions and technologies. For many clinical applications, virtual care has been shown to be either equivalent or even better than in-person care in some cases. In particular, there is strong evidence supporting the use of telemedicine for communication, counseling, and remote monitoring of chronic conditions such as cardiovascular and respiratory disease. Virtual care has shown improvements in outcomes such as mortality, quality of life, mental health conditions, and reductions in hospital admissions.
- Health Affairs: The Current State Of Telehealth Evidence: A Rapid Review — This review article has recent evidence regarding telehealth’s efficacy in various clinical areas, as well as its impact on health care utilization.
- Diabetes Research and Clinical Practice: Does Telemedicine Improve Treatment Outcomes for Diabetes? A Meta-Analysis of Results from 55 Randomized Controlled Trials — This review article has evidence regarding telemedicine’s effectiveness for diabetes management compared to conventional care. The authors find that telemedicine is more effective in improving diabetes outcomes than conventional care, particularly for type 2 diabetes.
- International Journal of Medical Informatics: Effectiveness of Telemedicine: A Systematic Review of Reviews — This review article has evidence regarding the impacts and costs of telemedicine, including for behavioral conditions. The authors note a continued need for larger, controlled studies of telemedicine interventions, as well as further study of telemedicine’s cost-effectiveness and impact on patient satisfaction.
- Agency for Healthcare Research and Quality: Telehealth: Mapping the Evidence for Patient Outcomes From Systematic Reviews — This evidence map contains 58 systematic reviews on telehealth, which concluded that there is sufficient evidence to support the use and effectiveness of telehealth for specific uses with some types of patients, including: remote patient monitoring for patients with chronic conditions, communications and counseling for patients with chronic conditions, and psychotherapy as part of behavioral health. Further, they find there is emerging evidence to support the use of telehealth for maternal and child health, as well as triage and urgent care. The PDF version is available online here.
Patient Satisfaction. Telemedicine has also been found to have high patient satisfaction, on par with in-office visits, due to ease of use and improved communication.
- BMJ Open: Telehealth and Patient Satisfaction: A Systematic Review and Narrative Analysis — This review article has evidence on patient satisfaction regarding telehealth effectiveness and efficiency.
- American Journal of Managed Care: Patient and Clinician Experiences with Telehealth for Patient Follow-Up Care — This article about patient and clinician perceptions of virtual video visits compared to office visits found that the majority of patients and clinicians reported no difference in overall quality between visit types.
Telemedicine to Address Health Equity.Evidence is growing on telemedicine use among diverse and low-income patient populations, including individual and population-level factors associated with telemedicine uptake and satisfaction
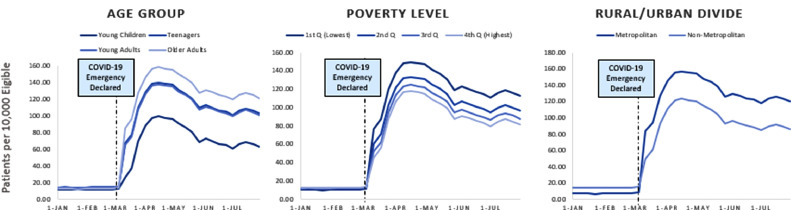
- American Journal of Preventive Medicine: Who Is (And Is Not) Receiving Telemedicine Care During the COVID-19 Pandemic — This research brief examines changes in telehealth use during the COVID-19 pandemic among over 6 million employer-based health plan beneficiaries. The authors found the increase in telemedicine use during the pandemic was greatest among patients in counties with low poverty levels, patients in metropolitan areas, and among adults (as opposed to children). They note the importance of prioritizing outreach to patients whose in-person care is not currently being replaced with telemedicine visits.
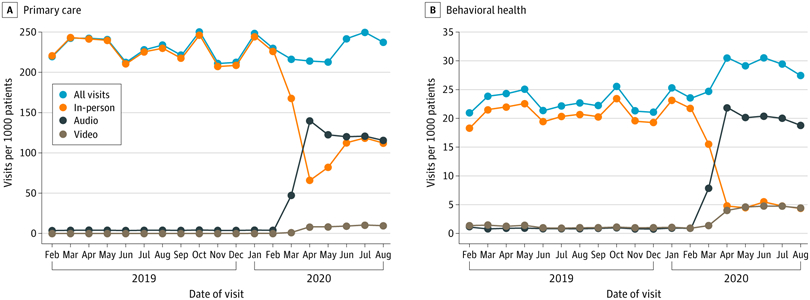
- Journal of the American Medical Association: Telehealth Use Among Safety-Net Organizations in California During the COVID-19 Pandemic — This short research letter describes the trends in the use of in-person, phone, and video visits among FQHCs in California before and during the COVID-19 pandemic. The FQHCs included in the analysis were participating in CCI’s Connected Care Accelerator program. They found that visit volume overall declined only modestly for primary care because telemedicine visits, especially phone visits, replaced in-person visits. The authors noted the importance of phone visits in meeting the needs of low-income patients.
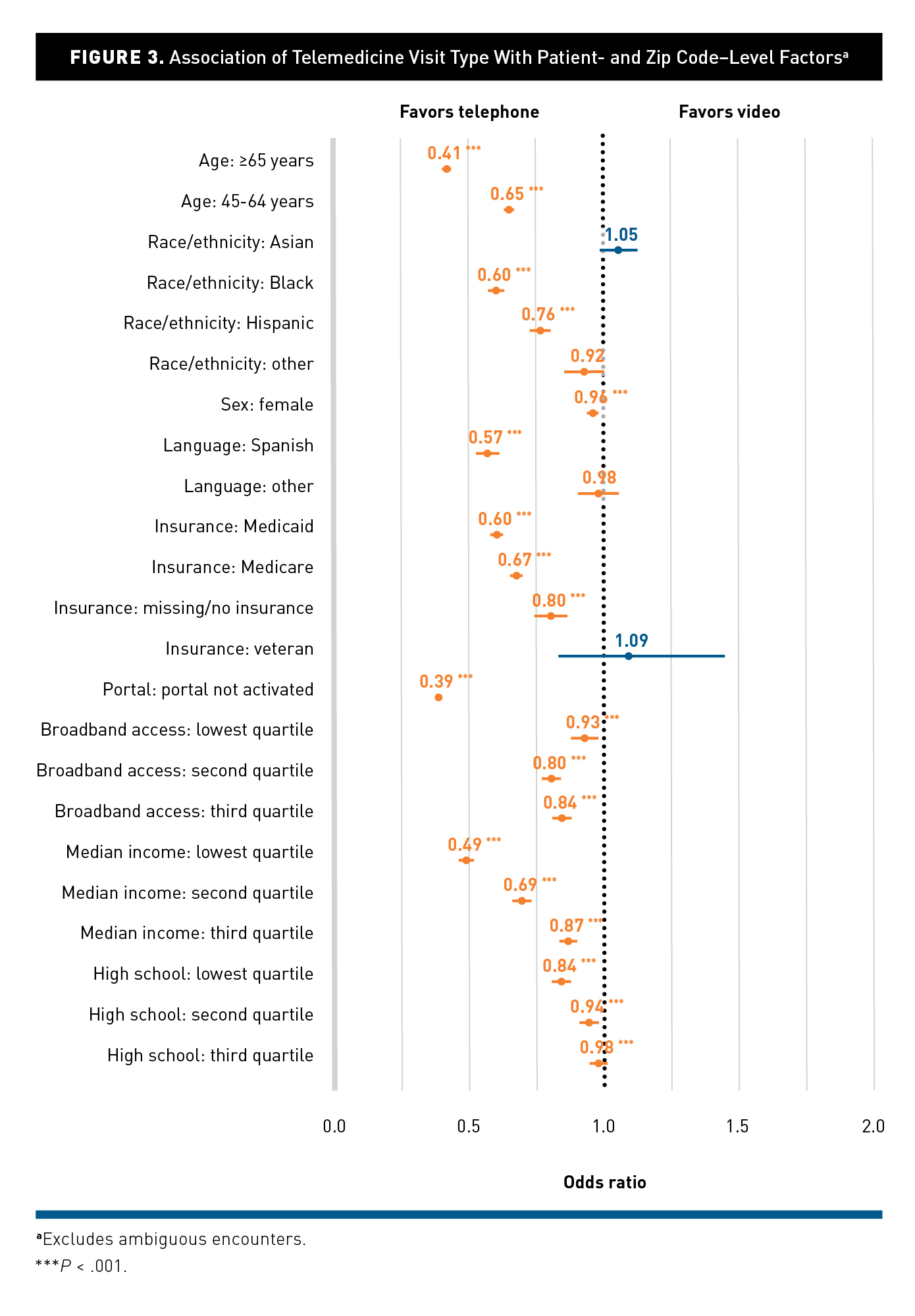
- American Journal of Managed Care: Differences in the Use of Telephone and Video Telemedicine Visits During the COVID-19 Pandemic — This cross-sectional study examined patient and neighborhood characteristics associated with visit modality (in-person, video, or telephone). They found that patients who were older than 65 years old, Black, Hispanic, Spanish-speaking, and from areas with low broadband access were less likely to use video visits. In addition, they found that practices and clinicians drove more of the variation in video visit use than patients.
- Health Affairs: Disparities in Telehealth Use Among California Patients with Limited English Proficiency — This study examines the association between patients’ limited English proficiency (LEP) and telemedicine use (phone and video visits). They also evaluated the impact of telemedicine on healthcare access and use. The authors found that LEP patients had lower rates of telemedicine use compared to proficient English speakers, and that telemedicine use was associated with increased emergency department use for all patients.
- JAMA Network Open: Patient Characteristics Associated With Choosing a Telemedicine Visit vs Office Visit With the Same Primary Care Clinicians — This article outlines patient characteristics associated with choosing between telemedicine and in-person visits within Kaiser Permanente Northern California. For example, the authors found that choosing telemedicine was associated with in-person visit barriers such as clinic parking costs. They also found that Black patients were more likely to choose telemedicine than other racial/ethnic groups, and patients living in lower socioeconomic status (SES) neighborhoods were more likely to choose telephone visits, but they were less likely to choose video visits than patients in higher SES neighborhoods.