Once the decision to integrate telemedicine into routine care delivery is made, frontline care teams must begin to deliver telemedicine efficiently, safely, and equitably.
Here is one of the key considerations for frontline teams.
Staff Roles. Telemedicine necessitates multiple new staff roles and workflows, including program management, site coordination, clinical oversight, technical support, and more. It is critically important to build in staff expertise and adequate time for patients with varying levels of digital literacy to successfully join and participate in telemedicine visits. Many clinics are experiencing a higher visit volume with telemedicine and scheduling should account for this higher show rate. During a visit, it is critical that each team member know their role and the needed electronic medical record documentation practices.
- California Telehealth Resource Center: Telehealth Program Developer Kit — This PDF lays out the staff roles needed for successful telemedicine implementation in the “Staffing” section beginning on page 161.
- American Academy of Family Physicians: A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice — This PDF provides a comprehensive guide to developing and improving a telemedicine program. Starting on page 16 it outlines a framework for approaching telemedicine staffing and roles, and starting on page 32 there is a section on documentation and consent requirements, including a sample patient consent form for staff to use with patients.
Scheduling and Triage. Determining whether telemedicine vs. in-person care is more appropriate, is the first step in carrying out new telemedicine workflows. The resources below offer guidance on how to approach scheduling and triage with a telemedicine system in place.
- Health Information Evaluation and Quality Center (HITEQ): Getting a New Workflow and Process Started During COVID-19 Pandemic — This is a link to download a PDF with information about getting a new workflow and process started during the COVID-19 pandemic. This guide includes a section called “Come up with a triage plan” on page 3, which outlines the key steps to determining which patients should be seen in the office and which should be seen via telemedicine.
- New England Journal of Medicine Catalyst: Seeking Evidence-Based COVID-19 Preparedness: A FEMA Framework for Clinic Management — This article includes decision-making flowcharts to assist in scheduling decisions.
 Schmidt. NEJM Catalyst. 2020
Schmidt. NEJM Catalyst. 2020- American Academy of Family Physicians: A Toolkit for Building and Growing a Sustainable Telehealth Program in Your Practice — This PDF provides a comprehensive guide to developing and improving a telemedicine program. Starting on page 19, it includes a section on determining telehealth appropriateness, including a list of considerations for determining when telehealth vs. in-person care is better. Also, starting on page 25 there is a section on scheduling, including sample scripts to use when scheduling and confirming telemedicine appointments.
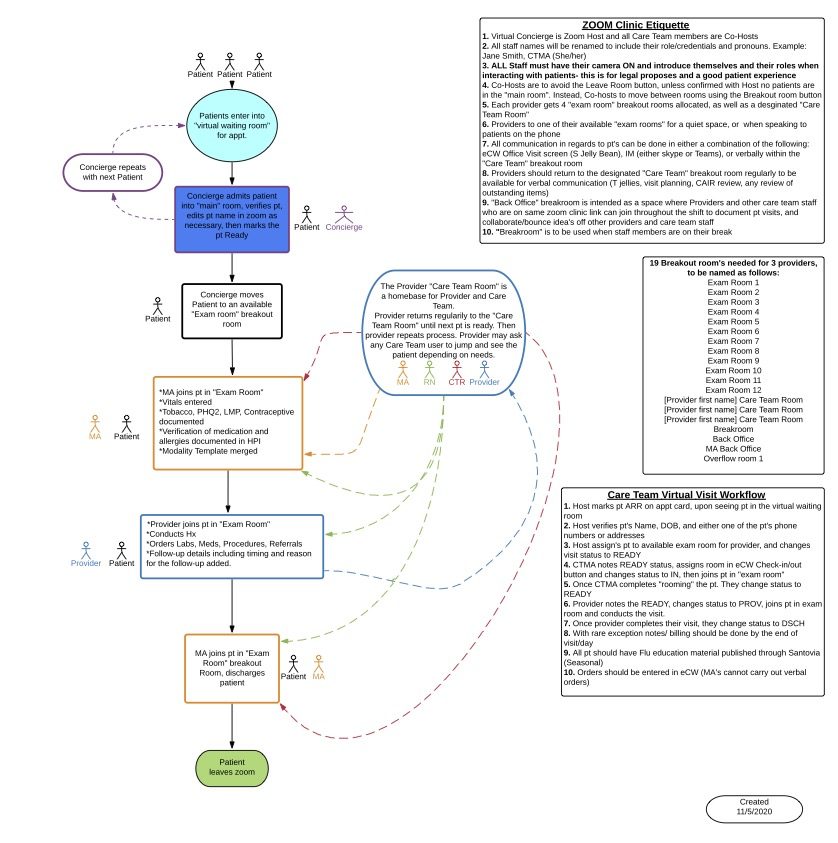
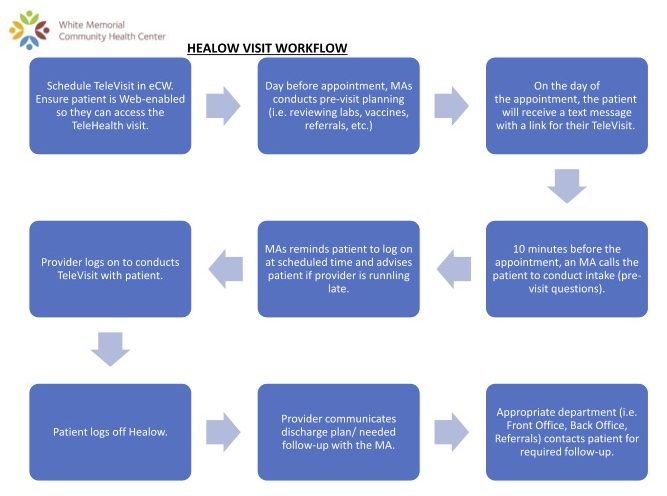
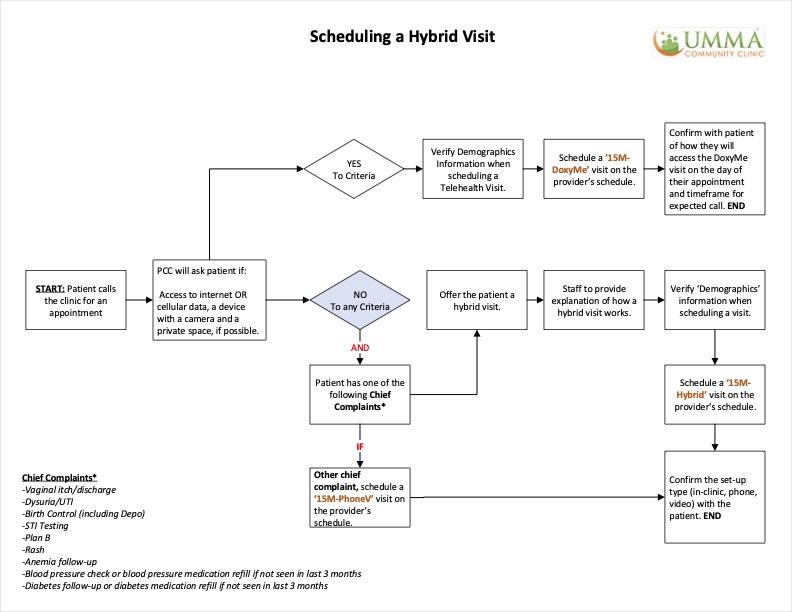
Workflows. Delivering high-quality, equitable telemedicine care requires new workflows and protocols. Transitioning team-based workflows from in-person care to telemedicine is an ongoing challenge, and many health care settings are currently experimenting and innovating on how to do this well. The resources below offer real-world examples of how various health systems have approached these aspects of telemedicine implementation, including several examples from public and FQHC sites specifically.
- West County Health Centers: Virtual Clinic Workflow Using Zoom Breakout Rooms — This workflow provides a “virtual clinic layout” for care teams using Zoom breakout rooms for telemedicine. It includes descriptions of different administrative and clinical team members’ roles in managing a Zoom clinic, from patients’ first check-in through the telemedicine visit itself and discharge. This tool was created by West County Health Centers — a Federally Qualified Health Center offering comprehensive medical, dental, behavioral health, and other specialty services to the communities of western Sonoma County, California — as part of their work through CCI’s Connected Care Accelerator.
- Petaluma Health Center: Tech Volunteer Workflow — This is a workflow for volunteers providing tech assistance to patients prior to their telemedicine appointments. It includes steps such as checking whether patients have email addresses, eClinicalWorks patient portal access, and the Healow and Webex apps, and completing appropriate consent documentation. This tool was created by Petaluma Health Center — a Federally Qualified Health Center offering comprehensive medical, dental, mental health, and specialty care services for communities in Petaluma, California — as part of their work through CCI’s Connected Care Accelerator.

- White Memorial Community Health Center: Video Visit Workflow — This is a workflow for scheduling and completing a video visit using Healow, an application from eClinicalWorks. It includes steps such as ensuring patients’ web accessibility, conducting pre-visit planning, sending text message reminders, and following up with patients after the visit. This tool was created by White Memorial Community Health Center — a non-profit health center in Los Angeles, California that provides primary healthcare services to children, adults, and seniors regardless of patients’ ability to pay — as part of their work through CCI’s Connected Care Accelerator. To learn more about how White Memorial improved video visit infrastructure and assessed patient satisfaction with telemedicine, check out this case study.
- UMMA Community Clinic: Hybrid Visit Workflows — This collection of three workflows provides guidance for scheduling, confirming, and completing hybrid visits using Doxy.me and eClinicalWorks. Some sites have found hybrid visits useful if patients need to come on-site in order to access the internet, devices, or private space needed to complete a video visit as well as to access specialty care that may not be accessible locally. This tool was created by University Muslim Medical Association (UMMA) Community Clinic — a Federally Qualified Health Center and Patient Centered Medical Home in Los Angeles, California providing medical, behavioral health, educational, and other services to promote the wellbeing of the underserved, regardless of ability to pay — as part of their work through CCI’s Connected Care Accelerator.
- Center for Care Innovations: How San Mateo Medical Center (SMMC) Harnessed All Care Team Members to Streamline Telemedicine Workflows — This case study describes how San Mateo improved their telemedicine workflows by streamlining virtual “warm handoffs” between team members during telemedicine visits and incorporated social determinants of health screening into their standard telemedicine workflows.
- New England Journal of Medicine Catalyst: Rapid Implementation of Telepsychiatry in a Safety-Net Health System During Covid-19 Using Lean — This article provides a breakdown of applying the LEAN quality improvement approach to rapidly implement telepsychiatry in a safety-net system, including reports of hours invested per role, detailed workflows, and examples of PDSAs to apply a quality improvement approach to your setting.

- Care Oregon (Medicaid health plan): Telemedicine Technical Assistance Guide — This PDF provides guidance on what can be treated by telemedicine starting on page 2 (video, phone and e-visits). Starting on page 8, there is information about how to integrate phone and video visits into workflows. There is also guidance around telemedicine for integrated behavioral health.
- Center for Care Innovations: Telehealth and Telephone Visits in the Time of COVID-19: FQHC Workflows and Guides — This article has sample visit and documentation workflows for switching from in-person to telephone and video visits developed by FQHCs using Nextgen and eClinicalWorks electronic health record systems. These include pre-visit patient reminders with English and Spanish versions of a script, team member call initiation, intake, and clinician documentation.
- Mid-Atlantic Telehealth Resource Center: Sample Telehealth Policies and Procedures — This PDF includes real-world example workflows and protocols for telemedicine implementation.
- UCSF Center for Vulnerable Populations: Resources for Telehealth at Safety Net Settings — This webpage provides resources for telehealth in safety net settings. The section “For Clinicians” includes a link to download a word document “Quick guide to your first telehealth visit” for clinicians using Zoom, with documentation guidelines that are not specific to any electronic medical record.
- Epic: Telehealth and Remote Care to Combat COVID-19 — This webpage is about how telehealth and remote care are being used to combat COVID-19. At the bottom of the page there is a link to a white paper, accessible if your organization uses Epic, called “Managing Coronavirus Disease 2019 (COVID-19) With Epic” which is updated regularly with recommended build and workflows. In addition, there is a link to a webinar from Epic’s telehealth team, also accessible if your organization uses Epic. If you have trouble accessing these resources, you can contact [email protected].