Dan Kurywchak is on a mission to save you from yourself – technologically, that is.
 The CEO of Telemedicine.com, Kurywchak has been working in the field before smart phones went mainstream. Over the past 20 years, he has helped organizations around the world start up telehealth programs at places ranging from Intel Corporation and a clinic in the heart of the Amazon to the UC Davis Health System, where he served as director of the Telemedicine Learning Center for 17 years before founding his company Telemedicine.com Inc.
The CEO of Telemedicine.com, Kurywchak has been working in the field before smart phones went mainstream. Over the past 20 years, he has helped organizations around the world start up telehealth programs at places ranging from Intel Corporation and a clinic in the heart of the Amazon to the UC Davis Health System, where he served as director of the Telemedicine Learning Center for 17 years before founding his company Telemedicine.com Inc.
In the wake of COVID-19, Kurywchak has been in high demand from providers forced to convert to virtual care almost overnight. He and his wife were just returning to California from a leisurely cruise celebrating their 27th anniversary when – hoping to avert a catastrophic outbreak – Governor Gavin Newsom announced a lockdown for the state’s 40 million residents. “From that time on, it’s been insane, just absolute mayhem,” Kurywchak says. “I’ve been working seven days a week from 7 or 8 in the morning to 10 at night for places from California to Switzerland.” He has some insider advice to hand out for providers and IT teams scrambling to set up a successful telehealth system for their patients. And woe to those who ignore it!
“I’ve seen people pay nearly $1 million to an outside company to set up equipment that wasn’t compatible with their existing platform,” he recalls. “You may be under enormous pressure to get a system up and running, but you’ve got to take the time to do your homework.”
A self-described “tech geek” who loved Radioshack electronic lab kits from the age of five and was so shy as a child that he would cross the street to avoid saying hello, Kurywchak is now a one-man tornado of webinars, phone calls, visits and Zoom consults about telemedicine. Here are some of his key recommendations — gleaned from talks with him and from his CCI-sponsored Telehealth Technology 101 webinar series — on how to avoid pitfalls when rolling out telemedicine:
1. Don’t blame your IT staff for all your telemedicine problems.
According to Kurywchak, few providers, healthcare administrators or even tech staff understand the basics of telemedicine, which — unlike the broader category of telehealth — always includes video-based transmission of medical data from a patient’s home to a provider. After all, many of us in healthcare still take “vertical” photos with our cell phones (!) instead of holding them horizontally to snap a shot, resulting in the wrong aspect ratio (9:16 vs the correct ratio of 16:9) and a distorted image. We don’t know 40Hz from 20khz, or a Ka band from a rock band. And why would we? According to Kurywchak, even 95 percent of IT staff have been hired to maintain network infrastructure, routers, switches, hubs, firewalls, security and server issues – not telemedicine issues.“I’ve heard of CEOs screaming at IT staff, saying, ‘What’s wrong with you — why don’t you know how to fix this?!’” Kurywchak says. “It’s not their fault — it’s a different specialty. It’s like asking a dentist to swing by the hospital and perform a C-section.”
2. Beware fancy marketing brochures.
“There is an amazing amount of grant money right now for telemedicine,” says Kurywchak. “But some of it is being wasted. Since the pandemic began, I have met with too many hospitals and clinics that are asking for help because their newly purchased software or hardware solution won’t work with their existing system or their specialists’ system. I’ve seen spending ranging from $120,000 to $1 million for something that could have been accomplished with $10,000 to $50,000 and that would have worked with their existing systems!” One problem, Kurywchak says, is that vendors often tell clinics what their software will do, but not what it won’t do – “They may not know or not tell you, for example, that their product is not compatible with your Electronic Health Record.” The bottom line: Always talk with a neutral expert before signing a contract. “There are Telehealth Resource Centers that cover every state in the country,” says Kurywchak. “That’s definitely a good place to start.”
3. Before choosing a company, call its tech support line.
Seriously: Whether you need tech support 24/7, 9 to 5 or just on weekends, call the company’s tech support line. How long did it take someone to call you back? Did they have the customer service skills you expect for your organization? “One week I called three different customer support groups and asked them to respond,” says Kurywchak. “Not one even called back.” In addition, he cautions not to forget to ask what time zone the company is in – and whether their regular working hours match yours. You don’t want to have a major data failure at 2 pm on the West Coast and find your East Coast customer support team has called it quits for the day. Make sure that the company offers top-notch, reliable customer support before signing up.
4. Test, test, test software solutions before deciding on one.
“Don’t take vendors assurances about software,” says Kurywchak. “Every place is different, and what may work for one company may not work for yours. No matter how much pressure you’re getting from management, experiment with software on a trial basis before making a decision. And make sure it’s compatible with the rest of your system before you commit to anything.”
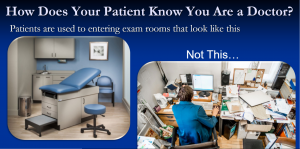
5. When doing virtual care visits, make your home office as professional as possible.
Here’s a key piece of advice from Kurywchak: Pay close attention to your video set-up for the best virtual care visit, because your patients may not. Here are some of his tips:–Check your patient’s ID (if your office hasn’t already done that).
- Dress professionally. “Wearing a lab coat, scrubs and a badge will make your patients feel comfortable,” Kurywchak says. “The ideal setting is an office with your diplomas on the wall behind you.”
- Clean up your computer desktop.
- Make eye contact. You should be looking towards the camera, not facing sideways.
- Keep your light source in front of you — avoid dark corners and backlighting unless you want to look like you’re in a witness protection program.
- Lock your door so you don’t get unintended cameos of family members.
- Invest in a speakerphone to avoid echoes and use a headset in loud or shared areas.
- Avoid swivel chairs and rocking chairs.
- Just say no to virtual backgrounds – amusing as they are, patients might get the wrong message, especially if they involve virtual wine or beer.
- Don’t eat or drink during the visit.
- Use a computer rather than a smart phone or iPad– it performs better, Kurywchak says.
- Keep your device stationary, Kurywchak says, “with no moving devices behind you, such as ceiling fans or trees moving in the wind” that might cause video distortion.
6. Take steps to avoid WiFi problems at home
If you have to use WiFi for your virtual visits, get as close to the router as you can. Also:
- Open all the doors and barriers between you and the WiFi.
- Avoid virtual backgrounds. Amusing as they are, they might strike some patients as unprofessional, especially if glasses of virtual wine are involved.
- If you’re working at home, close all applications running in the background (except for essential ones) and ask family members not to link their cell phones to the WiFi and to avoid heavy Internet use. If your kids are playing video games and watching a movie in the next room, your virtual care visit may suffer from bouts of frozen video, pixilation or worse. “You don’t want to take up more computer memory, or RAM, than you have to,” Kurywchak says. “Look at it this way – say, you have to make 100 sandwiches, One analogy is that RAM is the countertop, the fridge is the hard drive, and the computer’s “brain” or CPU is you. You need space to make all your sandwiches, so you don’t want to fill up the counter with a blender and microwave and a bunch of other stuff.
7. Get your patients’ help for a successful virtual visit.
This is valuable advice, as I can personally attest, since my first experience of a video exam during COVID left me scrambling for a flashlight so a physician could take a look at my son’s throat. If you’re able to contact your patients in advance, ask them have a table lamp or flashlight (regular or the cell phone variety) ready to help you examine their mouth or throat. Also, ask that your patients:
- Close all applications (such as email) running in the background
- Set their phones, laptops or tablets on a table to avoid movement that can results in distorted images
- Connect to home WiFi rather than cellular data
- Use ethernet if they have it
- If you’re having trouble hearing the patient, ask them to call you on the phone while keeping the video on
- If you’re having trouble with both audio and video, switch to a phone call as a last resort.
- Research what happened after the visit by starting with the basics: Check to see whether your speaker volume was down or whether it was unplugged. If you had a bad echo, try turning down the volume or moving your microphone further from the speakers. If you had problems with pixilation, move further away from the camera, reduce the connection speed, and/or turn off more apps.
- If none of these work, Kurywchak says, do some computer diagnostics by checking your settings: If your bandwidth “send column” is fine but you’re not getting any kb/s in the “receive” column, “it’s about 99% certain that your firewall is blocking it.”
8. Go wired instead of wireless if possible.
This may be an unpopular suggestion in the age of wireless, but in Kurywchak’s expert opinion, wired is by far the best solution – especially in the COVID era.

“Everyone is using the Internet – going to school, watching movies, playing video games, doing social media, vi8.siting family and friends – the Internet is overwhelmed,” he says. “No one can control Internet speed, and this can cause problems ranging from poor lip sync to pixilation or dropped calls.” Here’s how you can set up a wired system at your home:
- Get a long ethernet cable to reach the ISP network box to your computer.
- If you don’t have an ethernet port on your laptop or tablet PC, get a USB to Ethernet adapter.
- Extend ethernet over your home electrical system with wall plug-ins (avoid using it with power strips).
9. Consider investing in a Custom Telemedicine Cart
Don’t want to trip over a cable and bring all your apparatus crashing down on your head? Look into a Custom Telemedicine Cart (CTC), a lightweight, rolling cart with four hours of standby battery life. The one pictured below comes with a video camera with 12x optical zoom, a 24-inch monitor with a fixed monitor stand, and hospital-grade UPS (uninterruptable power supply). It’s equipped with touchpad passcode locking drawers, so you can secure all your medical devices (known as “peripherals” in the trade) when you need to move around, change rooms or grab a bite. Best of all, it’s designed so there are no exposed systems to be disabled or tampered with.
If you work in behavioral health, you might want to check out the more streamlined Behavioral Health Telemedicine Cart.
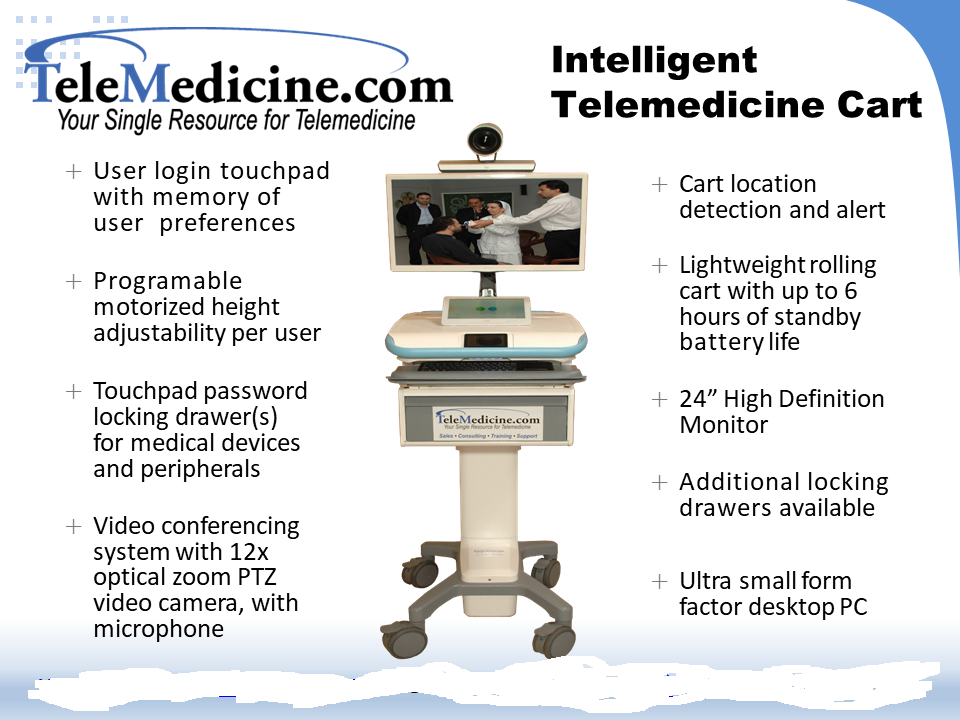
10. Buy the equipment that best suits your (and your patients’) needs.
Cloud services may be a better choice for distant sites depending upon your location; for leased lines or emergency use, point to point video conferencing via Cisco, Polycom and others is a better choice. For multiple specialties, a Custom Telemedicine Cart (#9) may work best, and it can be used with cloud-based services like Zoom. If you’re using a PTZ camera and speakerphone, a laptop or desktop should be fine for behavioral health visits.
Also, a word to the wise: When considering Internet broadband, Kurywchak says, don’t be fooled by confusing claims about Internet speed: The broadband speed you purchase is only between your location and your Internet Service Provider’s (ISP) central office, not the speed across the Internet. Kurywchak cautions: “Be aware that a virtual private network (VPN) encrypts your data – it does not improve your speed on the Internet.” Keep your speeds down between 768 Kbps and 512 Kbps; 384 Kbps is the lowest you can go without getting into lip-synch problems. If everything looks good, you can experiment with a higher bandwidth.
11. Make sure your medical peripherals (devices) are compatible with your platform.
This could be a matter of life and death in the field. Kurywchak has worked on telehealth with tribal leaders and physicians in African, set up a telemedicine operation for a tiny clinic on an island deep in the Amazon – the only clinic for 100,000 indigenous residents – and another in Lebanon to help treat life-threatening injuries from an estimated 100,000 unexploded bomblets from cluster bombs dropped on the country in a 2006 conflict. He has rolled out telemedicine on a South Korean ship, in a 200-bed hospital serving 4.5 million people in Nigeria, and in a remote rural hospital in California. “It was a lifesaver,” he says. “In one especially difficult birth at the hospital in California, the baby was born with the umbilical cord wrapped around its neck, but through telemedicine the doctor was able to locate someone at the nearest pediatric intensive care unit to walk him through the process of reviving the baby” and saving its life.
Simply put, a peripheral is a device that sends input into or gets output of a computer. Medical peripherals — including general examination cameras, stethoscopes, otoscopes, retinal cameras, fetal dopplers, and ultrasound are used in telemedicine to transmit data to a remote location where specialists can aid in stabilization, diagnosis, and treatment. However, most of these medical peripherals can only transmit data to a wired system and are not compatible with wireless. As Kurywchak recalls, “One place ordered 1,000 iPads for its doctors to do ENT (ear, nose and throat) exams, and their wired ENT scopes don’t work with wireless!”
To connect medical peripherals to devices that don’t have the same connector type, you’ll need to use adapters or transcoders that allow you to connect in and “output” to the kind of plug you need. The price ranges from $50 to $2,000. “You definitely get what you pay for,” says Kurywchak.
12. Think of your long-term goals.
It’s exciting to empower patients to take charge of their health with tools like blood pressure cuffs and glucometers and hold virtual check-ins. But could your health system go a step further? Home health telemedicine could transmit those readings directly to a physician from the patient’s home and send an alarm if variables go above or below designated ranges. “An extremely low-cost pharmacy device will not connect to a computer or transmit,” Kurywchak says. “But I’ve ad some good results in the $200 to $300 range.”
It’s less expensive – and possibly a great advantage during COVID — to distribute glucometers and blood pressure cuffs quickly so patients can do their own readings and give them to you or a medical assistant over the phone. “However, be aware that in some cases, patients will tell you what you want to hear,” says Kurywchak. In addition, if you’re collecting data for quality improvement programs, HEDIS will not accept diabetes measurements that are self-reported by patients. However, there are software platforms that don’t allow patients to edit the output, he says, so these are worth looking into.
Also, as you staff up to do telemedicine, Kurywchak says, remember that it’s crucial to hire tech employees with people skills. “You can have brilliant techies with no people skills working in the back room, but telemedicine tech employees have to interact with doctors in front of patients. You don’t want someone saying, ‘Oh my god, doctor, move over so I can fix this.’ When I’m hiring for telemedicine, I always ask applicants to tell me, in detail, how to use a pencil sharpener. The way they answer that question tells me a lot about their people skills and how patient and methodical they are (or aren’t).”
Enormous changes at the last minute

During our talk, Kurywchak mused over the enormous changes in electronics that have occurred since his early days as a computer operator on large mainframe computers at UC Davis or working for Shugart Technology (Alan Shugart invented the floppy disk), which shipped the floppy and then-revolutionary disk drives to Apple.
Kurywchak remembers that when he first gave lectures about telemedicine at UC Davis a few decades ago, doctors in the audience would get angry with him. “Physicians would get up in the lecture hall and say, ‘This ‘telemedicine’ will never replace me!’ But now doctors know it’s just another tool in their black bag.”
As for himself, Kurywchak feels lucky to be in a profession in which he learns something new every day. “That’s what I love about telemedicine,” Kurywchak says. “I’ve been doing this for 22 years, and there’s always more to learn. It’s like being a musician and playing for a living. You’ll never learn it all – never.”




