|
Background on White Memorial Community Health Center
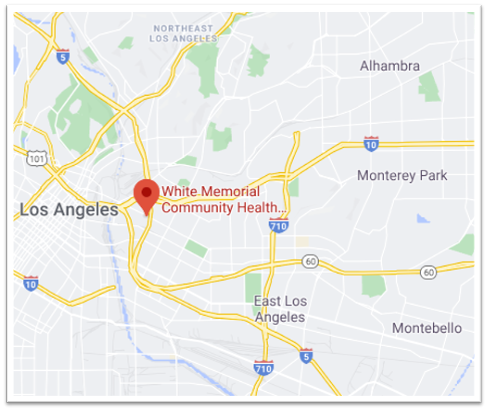
| Location | Population Demographics | Population Digital Connectivity | Patient Demographics |
| Boyle Heights, Los Angeles, CA | Nearly 40 percent of children live in households with income below federal poverty level.
95 percent of the population is Hispanic/Latino. |
18+ percent of households lack access to computer.
30+ percent of households lack broadband internet access. |
15,000+ unique patients served in 2019.
98 percent of 2019 visits were with Medicaid beneficiaries. 85 percent of patient population are pediatric patients. 40 percent of patient population is best served in a language other than English. |
Prioritizing Video Visits
Boyle Heights was among the hardest hit areas affected by the COVID-19 pandemic, with a cumulative case rate of over 20,000 cases per 100,000 people in March 2021 (compared to about 9,000 cases per 100,000 people in California as a whole). Prior to February 2020, White Memorial did not conduct any phone or video visits with patients, and like many practices nationwide, White Memorial rapidly shifted towards telemedicine at the start of the pandemic.
From the start, clinical leaders at White Memorial chose to prioritize video over audio visits and invested in resources to support them. These leaders emphasized video because:
- White Memorial has a primarily pediatric patient population, and they had found that audio-only telemedicine visits were challenging for kids and their families.
- They anticipated that future reimbursement for telemedicine would be tied to video visits.
At the same time, White Memorial’s leadership team also recognized that they would never be able to conduct all their telemedicine visits through video given the broadband access and affordability challenges faced by many of their patients. With that understanding, they continued to support audio-only telemedicine visits for patients who had connectivity and digital literacy challenges.
Improving Video Visit Access
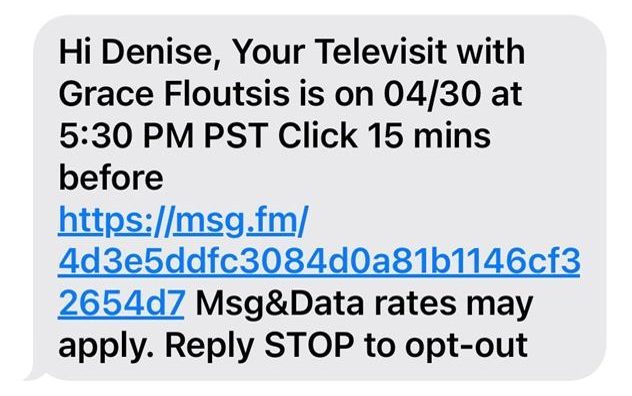
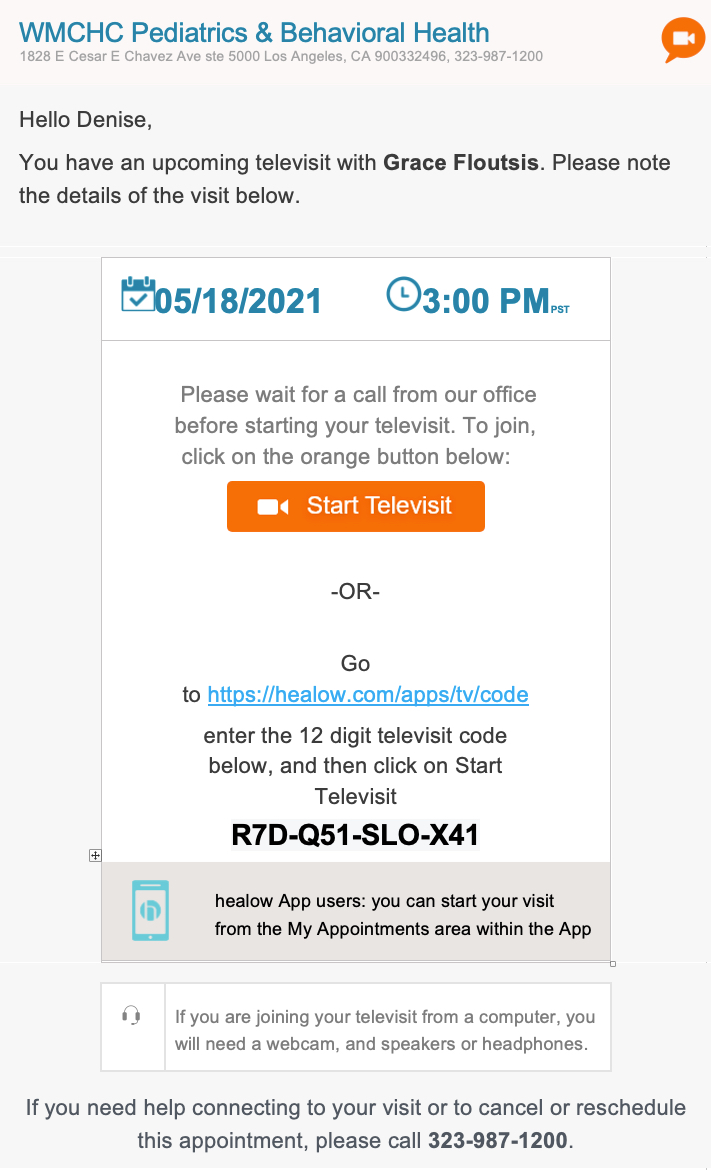
White Memorial chose to use their electronic health record platform — eClinicalWorks, which they had used since 2017 — to deliver telemedicine care. In the initial rollout stage, patients had to download and navigate through a mobile application in order to participate in a video visit. White Memorial staff quickly recognized that this process was too labor intensive and complicated, creating barriers for many patients. To improve video visit access, White Memorial zeroed in on streamlining this workflow. Patients now receive a link sent through email or text which they can use to directly launch their video visit via their web browser. Further, White Memorial discovered that there were certain areas in the clinic where the Wi-Fi connection with a laptop was too slow for video visits. To overcome this challenge, they purchased small cameras to place on top of in-clinic desktop computers, which had a wired internet connection and gave them five times better speeds and better resolution for conducting video visits. With this fix in place, most medical providers conducted video visits from on-site, though behavioral health providers worked both from home and in the clinic providing video visits.
→ Read more about this televisit workflow and others in our Telemedicine for Health Equity Toolkit
Adjusting Scheduling to Accommodate Video Visits
The White Memorial providers also found that scheduling their telemedicine visits back-to-back created more pressure than back-to-back in-person visits, given the need to manage patients waiting online and often time-consuming technical troubleshooting. Many White Memorial patients struggle with internet connectivity and have phones that run on 3G or have limited bandwidth for video visits. White Memorial revised their scheduling process by lengthening pediatric follow-up visits first to 20 minutes, then to 15 minutes (compared to 10 minutes pre-pandemic). Further, White Memorial recognized that overbooking to account for no-shows caused many problems when providing virtual care, for if two patients logged on for a video visit at the same time, White Memorial was unable to accommodate them as easily as when two patients arrive in the clinic in-person at the same time. With this in mind, White Memorial developed a policy in family medicine not to overbook appointments, even though they kept the 20-minute visit length the same as it had been pre-pandemic. While this did reduce productivity when patients missed appointments, it eliminated the risk of having to manage multiple patients logging on for a video visit at the same time. In addition, now that some preventive care visits are again being conducted in-person, White Memorial is spreading video visits out over the course of the clinic day to avoid back-to-back video visits.
Piloting a Patient Satisfaction Survey
Finally, White Memorial developed a post-visit survey to assess patients’ satisfaction with their telemedicine experience and disseminated the survey by text in both English and Spanish. After pilot testing their survey in a few primary care clinics, White Memorial sent their survey to more than 3,500 English-speaking patients and more than 1,000 Spanish-speaking patients. They have received over 300 completed English surveys and nearly 75 completed Spanish surveys. Of these, more than 80 percent of English-speaking patients and more than 75 percent of Spanish-speaking patients reported that they were always satisfied with the treatment they received through their video appointment. More than 80 percent of English-speaking patients and 80 percent of Spanish-speaking patients said they would recommend video appointments to their family and friends.
Lessons Learned
Following these changes in telemedicine processes at White Memorial, by February 2021, about 30 percent of their primary care visits overall (including in-person, phone, and video) and half of their behavioral health visits were video visits. Of all their primary care telemedicine visits (including video and phone) nearly 70 percent were video visits. The organization’s ability to dramatically increase the percent of visits done by video – compared to phone – is attributable to their efforts to:
- Streamline telemedicine workflows,
- Improve access by texting and emailing direct appointment links to patients,
- Build more time into appointment scheduling to allow for troubleshooting technological difficulties, and
- Use desktop computers with hardwired broadband connections.
White Memorial assessed the difficulty with streaming video visits given their patients had limited access to technology, broadband, or were still learning how to interact in the digital world. Their investment in assessing patient satisfaction will be critical in informing their continued refinements of their telemedicine practice. Now that more patients and community members have received COVID-19 vaccinations, more in-person visits are being scheduled. But White Memorial plans to continue offering telemedicine particularly for certain visit types well-suited to virtual care, such as hospital and emergency department follow-ups, as well as to meet patients’ modality preferences, as many White Memorial patients are still requesting video visits and they anticipate it will continue to be a desired service.




