Central to effective and equitable implementation of telemedicine care is engaging a diverse patient population. This is one of the most pressing areas of consideration to ensure telemedicine does not worsen existing health disparities.
Building Trust During the Encounter. Considerations for patient trust must be woven into all efforts to support telemedicine. Previous research has clearly documented patients’ desires to maintain in-person relationships with providers and continued patient concerns about privacy and security related to telemedicine. Developing communication around how telemedicine will be used in conjunction with in-person care and as a way to increase support and connection for patients — as opposed to substitute or replace routine care — will be critical to any program. This is particularly important when caring for patient populations who experience justified mistrust of medical institutions and fears of surveillance because of historical and present abuses.
- Advisory Board: Tips to Improve Your “Webside Manner” — This website has an infographic on how to ensure telemedicine care remains patient-centered. Tips include ensuring a clear, well-lit screen view and presenting in the professional attire that works best for you. A visual ID badge may be reassuring especially for a new patient visit. Just as in in-person visits, refrain from eating or multitasking and maintain eye contact.
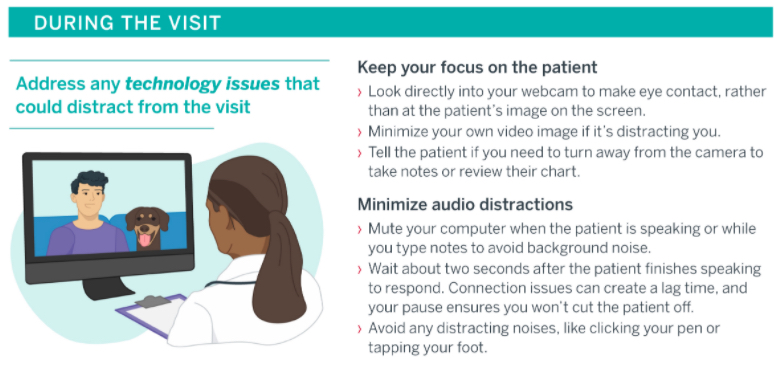
Advisory Board
- Center for Care Innovations: Empathetic Communication in Phone and Video Visits — This webinar by an expert motivational interviewing trainer reviews best practices in empathy-based communication for virtual health care settings. Links to additional PDF resources with tips for empathetic communication when providing care by phone and video can be found online here.
- Cleveland Clinic: COVID-19 Response Digital Health Playbook — This PDF provides guidance from the Cleveland Clinic on the expansion of telemedicine and digital health platforms. It includes a section on “Empathy in Virtual Visits” on pages 43-47 with helpful tips on establishing patient relationships, expressing empathy, and conveying value and respect during virtual visits.
- UCLA Pediatric Psychology Consultation Liaison Service: COVID-19 Tips—Building Rapport with Youth and Adults via Telehealth – These two PDF resources provide tips on setting the scene, introducing telehealth to patients, building rapport, and keeping adult and youth patients engaged in telemedicine visits. While some information is specific to mental health, most is broadly applicable to telemedicine care. The PDF focused on adults also includes a section focused on group telemedicine sessions.
Communicating Changing Models of Care. Special attention should be paid to communications regarding changes to protocols and models of care due to the COVID-19 pandemic. Clarity regarding office open hours, in-person availability, safety protocols, and new telemedicine offerings will be crucial to maintaining patient trust.
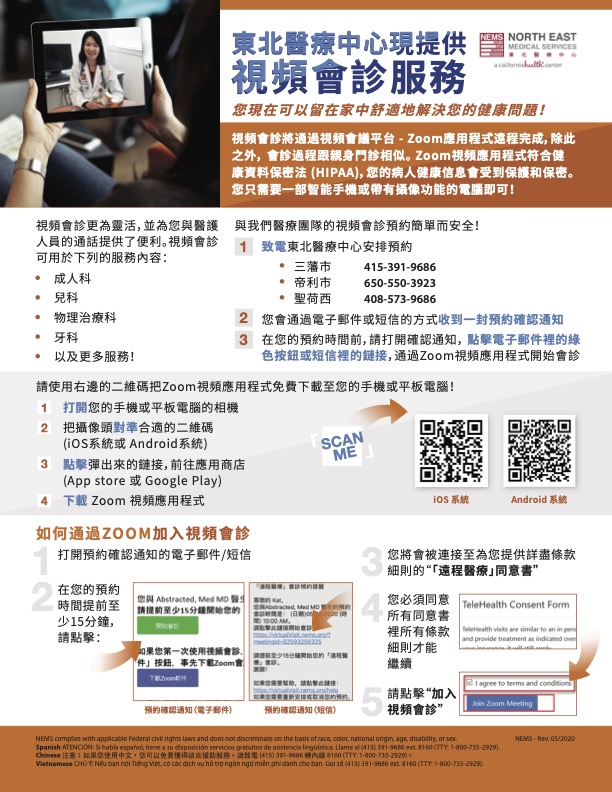
- North East Medical Services: Video Visit Flyer and Instructional Videos —These flyers were designed to promote the availability of video visits in English, Chinese, and Vietnamese. The flyer also includes instructions on how to download and use Zoom for the video visit. In addition, these short instructional videos in English, Cantonese, and Mandarin help patients navigate using Zoom. These tools were created by North East Medical Services (NEMS) — a community health center serving the medically-underserved populations of the San Francisco Bay Area, California and one of the largest community health centers serving Asians in the United States — as part of their work through CCI’s Connected Care Accelerator.
- Neighborhood Healthcare: Demonstrating a Video Visit Workflow — This video walks through the entire video visit process using eClinicalWorks and Doxy.me, from when a patient calls for an appointment to the visit itself to the post-visit follow-up. The goal is to help demystify the telemedicine process for patients who may be unsure about what a video visit entails. This tool was created by Neighborhood Healthcare — a Federally Qualified Health Center with sites throughout San Diego and Riverside counties in California that provide medical, dental, and behavioral health services to every member of their community, regardless of situation or circumstance — as part of their work through CCI’s Connected Care Accelerator.
- Northeast Valley Health Corporation: Patient Video Visit Tutorial (Spanish) — This video provides a Spanish-language overview of the video visit process using Otto Health. It outlines what a video visit is, what the visit confirmation texts and emails will look like, tips for logging on with a compatible web browser and checking connection quality, displaying the video visit portal instructions in Spanish, giving access to the device’s camera and microphone, the virtual check-in and waiting room processes, how to use the chat function, and how to add an additional person to the visit. This tool was created by Northeast Valley Health Corporation — a Federally Qualified Health Center with 14 sites in the San Fernando and Santa Clarita valleys in Los Angeles County, California providing medical, dental, and behavioral healthcare for uninsured and medically underserved patients with limited financial resources — as part of their work through CCI’s Connected Care Accelerator
- California Medical Association (CMA): Reopening a Medical Practice: Communicating with Your Patients and Others — This PDF is about communicating with patients and others about re-opening a medical practice during the COVID-19 pandemic. This guide has recommendations and templates to help health systems communicate with patients and other health care organizations about changes via email, social media, and signage. These templates can be modified to suit the needs of your practice.