Top Takeaways
|

There’s an ancient belief that good things come in threes, and a trio of safety net health clinics in California seem bent on proving that. During the pandemic, the three clinics explored three different options to support telehealth visits with their patients, with all eventually finding success.
One clinic tried an offsite, centralized telehealth hub, which ultimately didn’t hold up as a workable solution, so it moved on fast and found a better fix. Another created telemedicine-designated exam rooms that proved popular with providers and patients alike. And a third built telehealth pods within the clinic walls that continue to work well for care teams and clients.
These clinics — Neighborhood Health Care, Monterey County Health Department/Clinic Services Bureau, and Sac Health Systems — found creative ways to deliver quality, compassionate virtual care accessible to all as part of CCI’s Connected Care Accelerator. Here’s a look at their challenges and successes along the way.
Monterey County Health: ‘Providers appreciated the opportunity to give feedback’
Monterey County Health is a key service for both rural and town communities. It serves over 44,000 patients a year at 10 clinic locations in the small Northern California towns of Marina, Salinas, and Seaside. Approximately 80% of the organization’s patients are underserved and receive Medi-Cal and Medicare. Its clinics provide pediatric, primary care, internal medicine, obstetrics, behavioral health, and geriatric care.
Like all medical centers, Monterey County Health Department/Clinical Services Bureau made a quick shift to telehealth in the Spring of 2020. And like many other health organizations, Monterey County Health quickly discovered its setup for remote exams was less than ideal. Clinicians complained that background noise made it difficult to hear their patients and share information. Patients surveyed about the situation confirmed the sensory overload, which made it hard to focus. It was distracting and detrimental to optimal care.
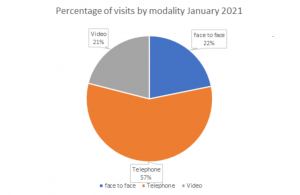
Video visits triped from 7% in Aug. ’20 to 21% in Jan. ’21. Credit: Monterey Health
The organization knew it needed to address the problem fast. So Monterey County Health decided to establish two designated telemedicine rooms at its Alisal Health Center location in Salinas: exam rooms that are used solely to provide telemedicine services. The organization also invested in equipment: It purchased noise reduction headphones and updated computer monitors from single to dual screens. Staff now have the tablets, cell phones, and laptops they need to do their job remotely. They also identified telemedicine software that suited both care teams and patients.
But the organization went beyond space configuration and tech support — it created an environment that felt calm and tranquil. Staff labeled the telemedicine doors and hallway areas as quiet zones. Acting on feedback from physicians, they introduced cubbies for each provider in the telemedicine room, so their specific equipment could be quickly accessed on their assigned telemedicine day. As a finishing touch, they hung soothing artwork in the exam rooms.
The innovation was embraced with open arms, according to Adriana Velez, outpatient services manager at the Alisal Health Center. Monterey County Health wants to expand the program to other clinic locations and is exploring creating a standalone telemedicine clinic site.
Clinic staff were surprised to have such positive engagement from the providers, notes Velez, who adds that physicians appreciated that the staff had solicited their suggestions and concerns. “I appreciate being given the opportunity to provide feedback. I feel my concerns and ideas were validated,” says Alisal Health Center physician Sara Lyon. “It was challenging to provide privacy during my video calls in a shared space. Now that we have dedicated rooms, I feel comfortable and safe providing telemedicine for my patients.”
Already, two exam rooms are proving insufficient, based on demand, so Alisal hopes to expand the program at its center, too. Clinic staff are also working on issues such as provider tools, including the need for ergonomic equipment.
In addition, the clinic found that it was important to create guidance on what types of visits would work well for telemedicine and which ones would not. For instance, “sick visits” (versus acute condition appointments) such as fever, cough, runny nose, sore throat, headache, diarrhea, rashes, bumps, and minor pain can often be addressed remotely. In contrast, well child visits, obstetrics and gynecology matters, newborn care, and acute concerns are best handled by face-to-face visits. The staff also learned that one solution doesn’t work for all and that they sometimes needed to tinker with adjustments for individual providers.
Sac Health System: Making Telehealth Pods Pleasant and Accessible
Sac Health System wanted to find ways to improve and sustain its virtual care model, too. The nonprofit community organization has nine clinics and two mobile units that provide affordable healthcare services, primarily to uninsured patients and their families in the Inland Empire of San Bernardino and Riverside counties in Southern California.
 The health center’s goal was to increase the volume of its virtual care visits and decrease its telephone-only appointments. Its first step was to establish a telehealth taskforce to address this and other virtual care concerns. Its members then scouted the sites to identify physical space for virtual care visits. Then, the question was, how should they configure the space to best serve providers? They settled on telehealth pods: private, designated booths in which providers could conduct video visits.
The health center’s goal was to increase the volume of its virtual care visits and decrease its telephone-only appointments. Its first step was to establish a telehealth taskforce to address this and other virtual care concerns. Its members then scouted the sites to identify physical space for virtual care visits. Then, the question was, how should they configure the space to best serve providers? They settled on telehealth pods: private, designated booths in which providers could conduct video visits.
The IT team tested multiple hardware solutions. Although providers in in-person exam rooms work from a single monitor, for example, they found providers preferred dual monitors for virtual visits inside the telehealth pod. Says one clinician: “Telehealth pods are pleasant to use, and all my tools are accessible in order to perform video visits.”
However, the team also realized that telehealth pods could be a problem if they were poorly ventilated or had lighting issues. Among other things, they recommend that clinics:
- Place telehealth pods in a location that has access to good light and good ventilation. Sac Health booths have built-in recessed lighting, windows, and fan ventilation.
- Confirm with the vendor in advance that the parts to assemble telehealth pods will fit through clinic doors.
Neighborhood Health Care: Flexible Space and Rolling Workstations
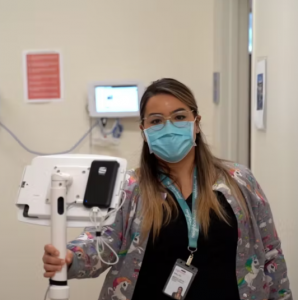
Ready to roll: Neighborhood’s portable workstations
Early on in the COVID-19 crisis, Neighborhood Health Care decided it needed to create a centralized, dedicated telehealth hub offsite that would offer care teams and providers a quiet and confidential environment in which to conduct telehealth visits. Just as with in-person visits, when a patient may be in a gown and need to disrobe for an exam, patients at home need the same level of privacy while meeting with their health team in front of a camera, explains Jeff Glenn, chief operating officer for Neighborhood Health Care. Makeshift setups—where administrative staff might walk past an open “exam room”— weren’t going to cut it for patient care.
Neighborhood Health Care — a federally qualified health center based in Escondido in Southern California with 19 mostly urban clinic locations serving 75,000 patients across San Diego and Riverside counties — had the resources for a telehealth hub. But as Neighborhood tried to sort out a solution for virtual visits, it became apparent within six month of the pandemic that patients wanted to return to in-person visits. Plans for a telehealth hub were scrapped.
Instead, the organization realized it needed a different physical configuration that took into consideration providers’ requests to see patients both in-person and remotely during morning and afternoon clinic sessions in their regular care team space. Providers, the organization learned, weren’t happy with only offering telehealth appointments; they wanted at least some in-person engagement during their work day.
In other words, providers needed a flexible model in which to care for their patients. Given that, Neighborhood Health Care switched up their thinking on telehealth hubs and opted to design a flexible space to meet the need. One solution that proved a winner: allowing providers to seamlessly transition from video to in-person visits by using mobile workstations. (See our story Rolling Exams: Workstations on Wheels Make Hybrid Consultations Easy).
Clinic patients also learned to get comfortable with virtual visits. “One patient was weirded out at first because she had never done a video visit,” says physician Heather Washington, Neighbor’s PACE medical director. “But [she] thought it was quite easy and a good idea to have this option.” Among other lessons learned:
- Adapt and pivot but stay flexible and responsive. Be prepared to put a potential solution on hold or discontinue it if it’s not working.
- Pleasing all providers with a single solution is tough to do.
- Expect the unexpected. Demand for in-person visits—even among high-risk patients—can happen more quickly than originally anticipated.
- Upfront planning is key to the success of effective video visits.
- Engage everyone on the team; brilliant ideas can come from unlikely quarters.
|
The COVID-19 pandemic upended the way California delivers health care. Health care systems completely restructured their services to keep both their patients and employees safe. Federal policymakers acted quickly to expand coverage and payment for virtual care. The California Department of Health Care Services also dismantled previous barriers to telehealth and began requiring Medi-Cal managed care plans to pay providers for telephone and video visits at the same rate as in-person visits. As a result, many California health care providers rapidly pivoted from in-person visits to virtual patient visits. For these organizations, this shift has been transformational, as they’ve adopted new technology, overhauled workflows, and redefined team member roles. The Connected Care Accelerator — a partnership between CCI and the California Health Care Foundation, with additional funding from the Blue Shield of California Foundation — selected 40 safety net healthcare centers in California to participate in a 12-month program that provided funding, methods, tools and hands-on technical assistance to enhance virtual care initiatives. In a series of case studies, CCI showcases the most sustainable and impactful solutions and shares advice for fellow safety net clinics who want to integrate similar virtual care strategies. |
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.

