It’s a crisis on top of a crisis. The COVID-19 pandemic has collided with the country’s opioid epidemic, shrinking access to life-saving treatments and recovery support services while compounding stress, isolation, and economic dislocation. By July of last year, deaths from drug overdose climbed by an average of 13 percent. In some states, deaths increased by 30 percent.* Meanwhile, high-cost emergency care for drug overdoses further crippled health care systems already flooded by COVID-19 cases.
Yet, despite the ravages of the pandemic, CCI’s Addiction Treatment Starts Here programs continue to transform treatment in California through an evidence-based approach to curbing opioid overdose and death. Through this programming, we’re increasing access to medications for addiction treatment (MAT) to help patients manage their opioid use disorder (OUD). What this means, as ATSH clinical director Brian Hurley has noted, is that primary care providers “can offer treatment that has a huge impact on the opioid epidemic in a way that wouldn’t have been possible before.”
This holistic approach incorporates behavioral therapy and support with FDA-approved medications — methadone, buprenorphine, or naltrexone. Buprenorphine — the newest medication in this group and the first to be dispensed in primary care settings — satiates the opioid receptors that cause cravings and can be dissolved under the tongue. Called by Health Affairs “a potentially transformative tool in health care practitioners’ fight to reduce deaths from opioid overdose,” buprenorphine is shown to significantly reduce drug use.
“The goal is to identify and connect patients to therapy and life-saving medications whether they intersect with clinics and hospitals or law enforcement, nonprofits and other touch points in the community and our health care system,” says Tammy Fisher, MPH, vice-president of the Center for Care Innovations. “This ‘no wrong door’ approach creates critical pathways to treatment and builds greater awareness of addiction as a treatable disease. The stigma and shame associated with addiction are significant barriers to care. Patients are less likely to access treatment, and there may also be a reticence to provide care. Our work supports health centers in reducing the shame often associated with addiction so that more people access life-saving treatment.”
Many patients interviewed at participating health centers were passionate about the MAT approach. At Marin City Health and Wellness, a young patient named Quincy said he no longer had to worry about relapse, since the medication he takes curbed his cravings. “It’s frustrating for me to hear stereotypes about [addiction] because most of us are just good people who have a sickness, who need help,” he said. Another patient named Morgan agreed. “I feel released; I feel like I’m like myself again, and then some,” she said. “I feel so much gratitude, more than I’ve ever felt before… for the chance to be the person I knew I wanted to be.”
Transforming treatment for a deadly epidemic
Opioid addiction is the country’s deadliest drug epidemic, killing more than 450,000 people since the 1990s — more than died in battle in World War II. Over the last five years, CCI has led medications for addiction treatment programs to improve treatment for people with opioid use disorder (OUD), helping more than 80 primary care health centers in California design or expand MAT programs.
“Evidence supporting the use of MAT shows mortality among patients with opioid use disorder can be reduced by more than half,” says Fisher of CCI. “Despite overwhelming evidence that prescribing medications is considered the gold standard of treatment, only 10 percent of people across the country receive it.”
Addiction Treatment Starts Here’s programs increased access to MAT by supporting more care teams to actively prescribe OUD medications. In fact, among the health centers that participated, the number of active MAT prescribers in California increased by 150 providers — equivalent to more than two active prescribers per participating clinic. CCI programs also helped clinics design effective programs, including identifying patients in need of care. The result? An increase of more than 2,000 patients receiving medications for addiction treatment. Many health centers doubled or tripled the number of patients accessing MAT for opioid use disorder. Central to these successes was CCI’s creation of learning communities, which offered a structured forum to learn new skills, share best practices, and crowd-source solutions to tough problems.
Through regular gatherings, site visits, webinars, and collaboration with peers, experts, and coaches, teams reported, they were able to develop new pathways for healing. As one participant in the primary care program wrote, “The coaching calls were extremely beneficial for problem-solving, brainstorming, and learning we weren’t alone in some of our challenges.”
Ironically, the onset of the COVID-19 crisis last March encouraged such innovation because federal agencies relaxed regulations on opioid use disorder treatment and providing virtual care for the duration of the pandemic.
Safety concerns during the COVID-19 pandemic, for example, led federal agencies to reduce barriers to prescribing MAT and expand access to remote care. Among other things, MAT prescribers could use telemedicine to prescribe medication for opioid use disorder and do so without requiring a prior in-person visit. Many providers also extended prescriptions for buprenorphine and other MAT medications up to 90 days, so patients would not have to get refills at a pharmacy or clinic as often. During the pandemic, federal agencies also permitted providers to allow home delivery for MAT drugs such as buprenorphine.
“The pandemic changed everything about how health centers provided MAT care,” noted ATSH evaluator Mark McGovern, PhD, a professor in the Department of Psychiatry & Behavioral Sciences at Stanford. “Most clinics adapted medication visits and counseling visits, redesigned workflows to accommodate more virtual care, and had to ramp up outreach to patients who might need addiction care, while simultaneously reducing barriers to access this care.”
Partnering with California to curb the opioid epidemic

CCI’s addiction treatment programming is part of California’s larger effort to curb the opioid epidemic across the state. Thanks to funding from the California Department of Health Care Services and Cedars Sinai, the Addiction Treatment Starts Here program was born. The state funds were part of a State Opioid Response Grant funded by the Substance Abuse and Mental Health Services Administration, which has documented that 2.1 million Americans over age 12 suffer from opioid use disorder.
To date, CCI has run four programs in this space:
- Treating Addiction in Primary Care Safety Net, funded by the California Health Care Foundation;
- Addiction Treatment Starts Here: Primary Care (two cohorts),
- Addiction Treatment Starts Here: Behavioral Health, and
- Addiction Treatment Starts Here: Community Partnerships.
The program is now on the third wave for primary care.
Primary Care

This initiative, which supported dozens of primary care health centers in California with designing new or expanding existing MAT programs, saw many gains, including a 64 percent increase in the number of patients receiving MAT, according to an evaluation of its first two cohorts. Dr. McGovern observed that “health centers were creative in developing strategies to identify and engage patients in care. Many clinics focused on implementing low-barrier approaches to MAT. Supporting patients to get initial care, and then stay in treatment, is a team effort. ATSH teams put in the time to design solutions to persistent challenges.”
Participating health centers were especially enthusiastic about the coaching and learning sessions. “Our staff benefited significantly from the in-person learning sessions,” said one participant pre-pandemic. “Having time to brainstorm and develop a game plan as a team was priceless given that we would rarely have the opportunity to do this while on site at the clinic.” Another commented that “we did not know how much work we needed to do until I saw what other clinics were doing. Very humbling. Very inspirational.”
Among other things, the sessions discussed the intersection of childhood trauma and addiction. In one session, for example, ATSH coach Katie Bell talked with participants about why screening for Adverse Childhood Experiences, or ACEs, is important during the MAT intake process.
“A full-agonist opioid, such as oxycodone or heroin, is often the drug of choice for our patients with undiagnosed and untreated trauma because it numbs physical pain, emotional distress and mental anguish,” Bell told CCI. “This numbing of feelings can relieve the symptoms of post-traumatic stress disorder, such as anxiety, avoidance behaviors, intrusive disturbing memories or flooding of traumatic memories.” What’s crucial for MAT team members to understand, she says, is that buprenorphine (Suboxone) “allows for the return of the felt experience of sensations and emotions…Patients will find it helpful to understand that recovery includes healing uncomfortable and distressing feelings. And that part of their MAT care will be support, therapy and basic coping tools specific to the feelings associated with childhood trauma.”
A recent evaluation report touched on some of best practices the clinics developed, including:
- Moving from a doctor-centric to a team-based approach to care. By including a multidisciplinary team that included a prescriber, nurse, medical assistant, behavioral health clinician, addiction counselor, and care coordinator/case manager, clinic staff were able to develop close, supportive relationships. As one said, “You need to rely on and trust the people around you — this is not a one-person job.”
- Changing hearts and minds through patients’ stories. “An evidence-based approach to demystifying and debunking stereotypes is exposure to a person with lived experience,” the report noted. As one rural clinic employee recalled, “We made a point of telling stories of our patients whose lives were transformed because of MAT. These were the sort of patients who were known to the clinic…and who were often seen as ‘drug seeking’ or ‘sociopathic’. So, when these patients became better moms, workers and simply looked happy and healthy — with the patients’ permission — we made sure people knew about it.”
- Embracing addiction as chronic disease management. Teams worked hard at their clinics to promote the understanding of addiction as a chronic disease. As one participant commented, “You wouldn’t threaten to discharge a patient with diabetes whose A1C was 10, but you seem inclined to give up on someone [taking medication for OUD] who relapses after a few months of stability. Instead, why wouldn’t you consider what the issues are and how you might adjust the treatment plan?”
- Partnering with community groups to address urgent social needs. Wendy Vierra, director of operations at Neighborhood Healthcare’s behavioral services, noted that her health center had joined forces with Interfaith Community Services to better serve the homeless population. “Relationships — building a credible, reliable safety net that wraps around our patients and is non-judgmental — is essential,” she told CCI. “Our vision is to give people the resources they need to live their best lives. We understand we cannot do that alone. We need the expertise of our community-based partners to provide whole person care and provide a solid foundation for wellness.”

Valley Health Association and two other substance use disorder treatment centers participated in the Boys and Girls Youth Summit (above) in Salinas, California.
- Expanding telehealth in addiction management. A necessity in the pandemic, telehealth will continue to play a strong role in many clinics after the program ends. Among other things, it has increased participation in support groups and allowed for faster communication. As one participant said about patient readiness for change, “Being able to have a phone visit with a patient the same day of their expressing interest has allowed us to ‘strike while the iron is hot’ in terms of [treatment].”
- Being aware that some patients need both MAT and treatment for chronic pain. “The most significant challenge is building an alliance with patients such that they trust you to not abandon them and their quest for pain control,” said Dr. Kenneth Petterson of the Olive View–UCLA Medical Center. “At the same time, we try to ‘do no harm’ and avoid therapies that provide more than just short-term relief…At our MAT clinic, we are realizing that more patients who come to us using heroin initially started with taking prescription opioids. This helps us to remember to make sure we’re addressing not only the addiction but to identify and treat their longstanding chronic pain, which can be an important trigger for disease relapse.”
- Practicing self-care. Addiction treatment is hard work, especially during a pandemic, and the program included webinars on staff self-care and wellness. Clinics shared their strategies for resilience, including storytelling, group hikes, opening all-staff meetings with meditation, celebrating successes, and incorporating more moments of joy and/or relaxation into the workplace through quick, informal huddles, buddy systems, and dance (including, at one clinic, salsa lessons). One team also recommended checking in prior to case review to ensure team members and their families had enough support.
Find out more about the primary care program’s accomplishments in the final evaluation of its first two cohorts (below). This spring CCI seeks to build on this success through its third cohort.
Behavioral Health

Addiction Treatment Starts Here: Behavioral Health also saw impressive gains. With more relaxed federal regulations during the pandemic, many program participants were able to make buprenorphine, methadone, and naltrexone more easily available to patients who needed them. The addiction treatment program’s behavioral initiative reported a 383 percent increase in patients receiving MAT for opioid use disorder, according to a CCI-Tides Foundation quarterly report.
“The addition of MAT has been transformative as it gives us a powerful tool to curb cravings in the critical stage when a client has decided to move toward doing something about addiction,” said Ellen Ahn, executive director of KCS Health Center. “Although early, we predict that our success rate for treatment with MAT will be much, much higher than behavioral health treatment alone.”
“The behavioral health project was designed like a learning lab,” said Sandra Newman, Addiction Treatment Starts Here co-director and consultant. She explained that the program brought together different behavioral health organizations – clinics providing substance use disorder care or treating serious mental health conditions, in addition to integrated sites providing both primary care and behavioral health. “Participants had an ‘all teach, all learn’ philosophy,” she said. “So even though we had many different types of organizations, there was so much we could glean from everybody’s experience in connecting patients to needed care.”
Community Partnerships
Addiction Treatment Starts Here: Community Partners included developing new initiatives for impact, with the challenge of COVID-19 and trying to build relationships in a virtual world.
Despite the barriers posed by the pandemic, Community Partnerships has been remarkably successful in bringing together unlikely allies in multiple sectors — “some of which historically have not ‘played nicely’ in the sandbox,” as one leader explained — to find common ground in the fight against the opioid epidemic. One of the program’s most powerful findings was that new tools from the learning collaborative were critical in building connection and trust with groups like law enforcement officials, some of whom committed to change their policies if that helped provide lifesaving treatments for addiction.
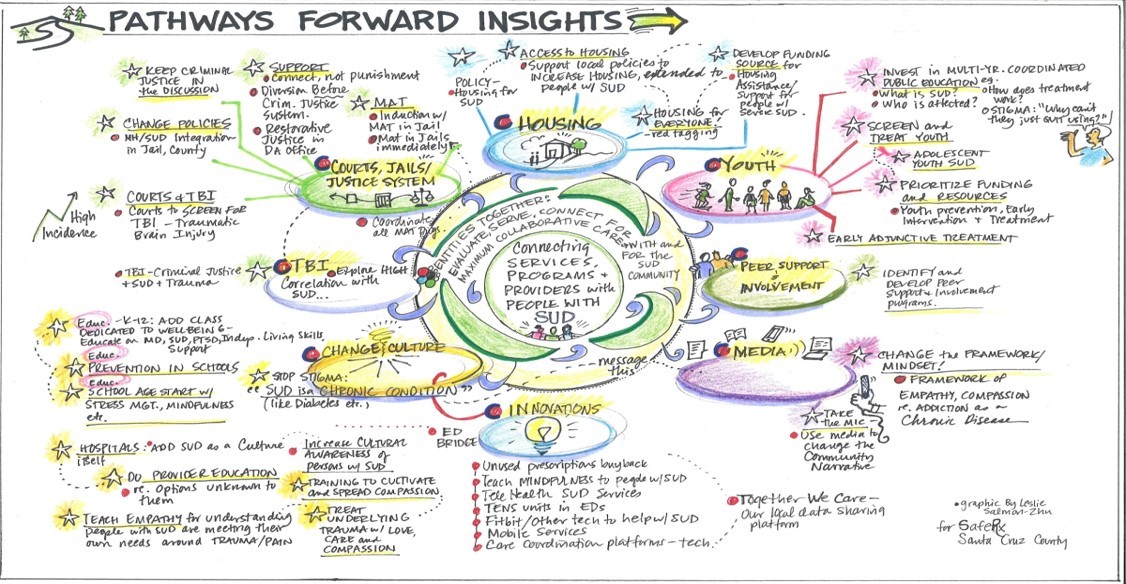
A SafeRx Santa Cruz County, for example, found “systems mapping” – a problem-solving tool that CCI is testing in the program– extraordinarily useful in building bridges and connecting with the local sheriff to support MAT. As one said, systems thinking “honors the gray areas and makes it easier to find the ‘we’ – even if the ‘we’ is complicated.”
Another coalition, Rx Safe Del Norte, placed indigenous approaches to healing and people with lived experience with addiction at the center of its work. Consider that in 2017, the county had a population of 27,470. The same year, there were 33, 932 opioid prescriptions — more prescriptions for opioids than people living in the county. The death rate attributed to opioids there is more than double the state rate.
The small rural community is home to a significant Native American population, which has been disproportionately hit by the opioid impact. Health care groups serving the local tribes joined family and community services to create the addiction treatment coalition and participated in CCI’s 16-month learning collaborative. Besides doing systems mapping, the coalition found partnerships with indigenous groups and healers key to its success. “There is a lot of indigenous knowledge around wellness and pain management that needs to be respected by the community and medical providers,” said coalition facilitator Jermaine Brubaker. “And that wellness may look different to indigenous communities.”
CCI had to cancel its in-person sessions for the program during the pandemic and figure out how to recreate its “secret sauce” for online collaboration. “There is real and pervasive Zoom fatigue,” according to a CCI’s quarterly report last fall. “People are looking for authentic connection, which can be hard to establish virtually. Complicating matters, some team members don’t have a quiet place where they can listen and actively participate in webinars.” Strategies to overcome these barriers included making learning sessions more interactive and redesigning Zoom breakout sessions to include a team lead to start each session’s discussion. Also, CCI kept the same people in the breakout rooms across all the sessions, which made it easier for people to get to know each other and build stronger relationships online.
Tracking changes in addiction treatment during the pandemic
Many providers expressed hope that relaxed regulations for MAT treatment and virtual care would continue after the pandemic. Stanford University and CCI researchers examined this trend early on in the pandemic, publishing their findings in an article for the Journal of General Internal Medicine this February. In a survey of 338 clinicians from 57 primary care clinics located in California, they found that:
- Most primary care clinics (52 out of 57) reported changing their practices in treating people with opioid use disorder in response to COVID-19 regulatory changes.
- Many clinics reported that both medical (40.4 percent) and behavioral health visits (53.8 percent) were now exclusively virtual.
- Two-thirds of clinics reported increased duration of buprenorphine prescriptions and reduced urine drug screenings.
- The majority of clinics experienced an increase in patient demand for behavioral health services.
- Over half of clinics described having an easier or unchanged experience retaining patients in care. One MAT program manager said, “Our group participation has gone way up to the point we are thinking of keeping it on Zoom.”
Battling stigma, embracing empathy

Despite national campaigns to reduce prejudice, people with opioid use disorder still encounter widespread stigma. CCI’s addiction programming and the MAT approach seek to dismantle stereotypes of substance users and to provide care with dignity, support, and mutual respect.
That approach is evident at Bay Area Community Health, an Addiction Treatment Starts Here participant that started a Zoom-based relapse prevention group during the pandemic — an innovation that proved highly successful. Lee Bradshaw, who oversees the health center’s substance use disorder program, noted the pandemic had increased patients’ isolation and anxiety: “We work with intelligent, sensitive people who do not do well in early recovery by themselves.”
“Taking this into account, we were concerned for our patient’s welfare without regular human interaction and support from like-minded people,” Bradshaw continued. “We started out with grief. It is our belief that substances are best friends for most of our patients, and there is a grieving period that goes along with having to quit.” After some weeks, she said, “We switched to discussing anxiety, and this seems to be appropriate given what is going on in the world right now.”
Surveying our participating health centers before and during the pandemic, we also found that:
- The most consistent barrier was stigma, both at the staff and patient level. Ellen Ahn, executive director of KCS Health Center, said that her organization’s stigma training addresses the biological and medical findings that de-stigmatize addiction. “It was well received and well worth the investment in bringing our team the expertise in addiction medicine,” she says. “The only recommendation we would make is that it takes commitment in resources and time to address stigma. And without the institutional investment, reversing the culture of stigma is difficult.”
- Multidisciplinary teams and staff buy-in were key to success, as was an approach that took cultural humility into account. “Families are a big part of people’s recovery,” said Brubaker of Rx Safe Del Norte, which includes members from neighboring Native American tribes. “Historical trauma adds another layer to this work we need to consider and address…We will continue to build empathy, break down stigma, increase access to resource, and reduce the barriers to treatment and recovery.”
- Flexibility, adaptability, patience, and compassion enabled teams to pivot during the pandemic. Building relationships is key, says Eric Schluederberg, DO, a family physician at the Kheir Clinic in Los Angeles. “It will take time. Be patient. You will often feel like you’re at a standstill, but a new program like this takes time to perfect. Don’t feel discouraged.”
Writer Sarah Henry and CCI program coordinator Briana Harris-Mills contributed additional reporting and writing to this story.
* Technically, our headline should say: “Tackling America’s Deadliest Ilicit Drug Epidemic,” because other drugs kill more people than opioids. As Dr. Brian Hurley has pointed out, alcohol is the number one drug people use and is responsible for 85,000 deaths per year. But the drug that is the biggest killer is tobacco products, including cigarettes. The cancers, heart attacks, emphysema, and chronic obstructive pulmonary disease linked to tobacco use “make it the number one killer,” Hurley says.
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.