|
Background on San Mateo Medical Center
| Location | County Population Demographics | County Population Connectivity | Patient Demographics |
| San Mateo County, CA | By July 2020, at least one in nine residents of San Mateo and nearby Santa Clara counties had insufficient food.
More than 14 percent of households are extremely low income, making less than 30 percent of the area median family income. More than 20 percent of the population is Hispanic/Latinx and over 30 percent is Asian. 43 percent of the population has limited English proficiency. |
Majority of area surrounding SMMC has broadband services.
Pockets of locations have slow or no broadband internet service. |
SMMC serves 55,000 patients annually in a Medicaid Managed Care plan
Prior to the pandemic, fewer than 100 out of SMMC’s 1,000+ weekly visits were conducted via telehealth. |
Telemedicine Platform Identification and Process Development

When selecting how best to provide telemedicine visits safely and securely, SMMC’s clinical team collaborated with the organization’s IT team to evaluate multiple telemedicine platforms, ultimately choosing Doxy.me. In the platform selection process, they prioritized ease of use, especially from the patient side – determining that even if other platforms offered more comprehensive services, the ability for patients to access the platform without having to download an app or sign up for a service was more important to meet their needs. In addition, based on SMMC’s large patient population with limited English proficiency, they knew they would need a platform with easy three-way video conferencing to allow interpreters to join telemedicine visits. The SMMC behavioral health team had also been looking into telemedicine platforms before the pandemic and had settled on Doxy.me, which helped speed up the platform selection process when the full system needed to pivot rapidly to telemedicine at the start of the pandemic.
Once settled on a platform, the team also relied on their patient service administrators (PSAs) to document verbal consent prior to the patient’s telemedicine appointment, with documentation available in English, Spanish, and Mandarin. This adaptation allowed for providers and patients to spend more time on medical concerns during the telemedicine visit, rather than on administrative tasks.
Surveying Providers and Patients to Identify Opportunities for Improvement
After the telemedicine program was first introduced, SMMC conducted a survey with patients and providers to identify challenges and opportunities for improvement. Providers said one major obstacle was the variation in telemedicine implementation and uptake across patients, clinics, and service lines, which made it difficult to achieve a uniform workflow and approach. For example, 80 percent of OB-GYN visits were conducted in-person, 50 percent of pediatric visits were in-person, while the majority of other adult patient visits were conducted through telemedicine with a mix of video and phone encounters. On the patients’ side, while they appreciated how telemedicine facilitated more immediate communication with their providers, patients reported receiving too many phone calls, or “touches,” by SMMC during the telemedicine visit process. Further, patients often blocked or did not answer SMMC’s phone calls because the calls weren’t easily identified as coming from the health system, making communication and scheduling difficult.
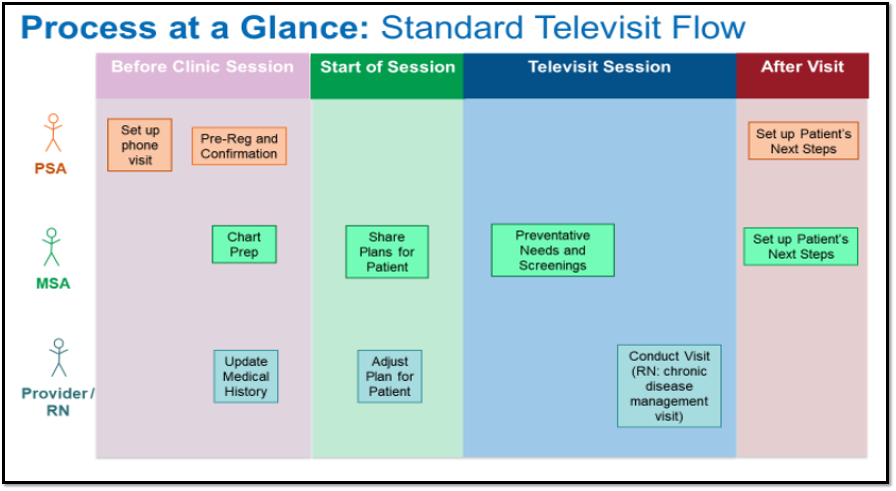
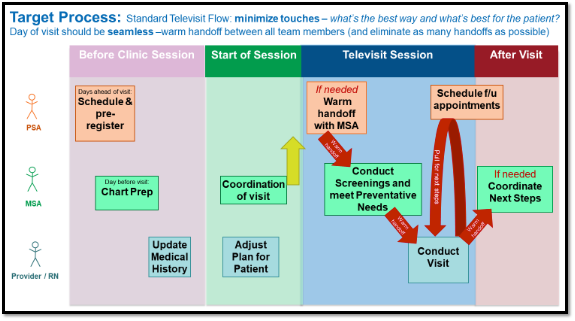
Refining Telemedicine Workflows
To better reach their patients, SMMC iterated on their initial workflow, with care team members from across all sites providing input. Clinic managers, physicians, nurses, and other clinical and administrative staff across primary care, OB-GYN, and specialty care came together to refine telemedicine processes for both audio-only and video visits. Responding to patients’ feedback about too many “touches,” SMMC incorporated “warm handoffs,” using shared virtual waiting rooms where the medical service administrators (MSAs) could prepare patients for their visits, conduct preventive health screenings, and schedule follow-up appointments. Using these shared virtual waiting rooms allowed for more efficient transitions between members of the care team without overwhelming the patients with many separate calls.
Incorporating Social Determinants of Health Screening into Telemedicine Visits
The team at SMMC also prioritized addressing social determinants of health during the development of their telemedicine workflows. Prior to the pandemic, MSAs would screen for food insecurity annually at patients’ in-person visits using a two-question scale. In developing their telemedicine workflows, SMMC made sure to retain MSA’s food insecurity screening as part of the virtual rooming process. Recognizing that rates of food insecurity were rapidly rising during the pandemic, they went further, incorporating screening for food insecurity into the standard telemedicine workflow at every visit, allowing for follow-up with a call or text to connect patients with a food bank.
At times, MSAs and providers noticed that some patients were hesitant to answer these sensitive questions, particularly if they had never met the care team in-person before and their first visit was via telemedicine. SMMC care teams developed specific phrasing to help make patients feel comfortable sharing these difficult experiences with their healthcare providers, such as prefacing the food insecurity questions with language like, “Given the pandemic and the especially challenging times right now, many people are experiencing food insecurity.” SMMC also offered connections to essential community services by connecting patients to 2-1-1 via phone, which provides support with housing, rent and utility assistance, and elder caregiving in both English and Spanish. Further, providers across SMMC were also recently trained to screen for adverse childhood experiences (ACEs) to better assess and meet the needs of their more vulnerable patients.
Food Security ScreeningENGLISH: For each statement, please tell me whether the statement was “often true, sometimes true, or never true” for your household. (Any patient answering with a 1 or 2 response is considered food insecure) Within the past 12 months we worried whether our food would run out before we got money to buy more. Within the past 12 months the food we bought just didn’t last and we didn’t have money to get more. Cuestionario para el Control de Seguridad AlimentariaESPANOL: Para cada pregunta, favor de contestar si en su hogar pasa lo siguiente: “a menudo,” “a veces” o “nunca.” (Si el paciente responde con 1 o 2 se considera en inseguridad alimentaria) En los últimos 12 meses nos preocupo que nuestra comida se acabara antes de que tuviéramos dinero para comprar más. En los últimos 12 meses la comida que compramos, se acaba rápidamente y no hay dinero para comprar más. |
Lessons Learned
The efforts at SMMC highlight the need to evaluate the patient experience early and incorporate the voices of all team members. Listening to feedback from patients and the entire care team allowed SMMC to:
- Make their workflows more patient-centered,
- Improve consistency and efficiency across different service lines,
- Connect patients with the appropriate supports,
- And develop a more holistic telemedicine program.
These changes helped SMMC create consistency in their process, reduce unnecessary handoffs, and improve the quality of care delivered. By providing opportunities for health promotion and case management, SMMC has been able to create a smoother transition for their patients while care is being delivered through telemedicine.
→ Get inspired by more examples and how-tos in our Telemedicine for Health Equity Toolkit
Find this useful or interesting? We’re constantly sharing stuff like this. Sign up to receive our newsletter to stay in the loop.
