Here, you’ll find the big-picture overview of the program. For more information about Resilient Beginnings, please visit the program page.
Navigation: Program Overview | Evaluation Overview

Here, you’ll find the big-picture overview of the program. For more information about Resilient Beginnings, please visit the program page.
Navigation: Program Overview | Evaluation Overview
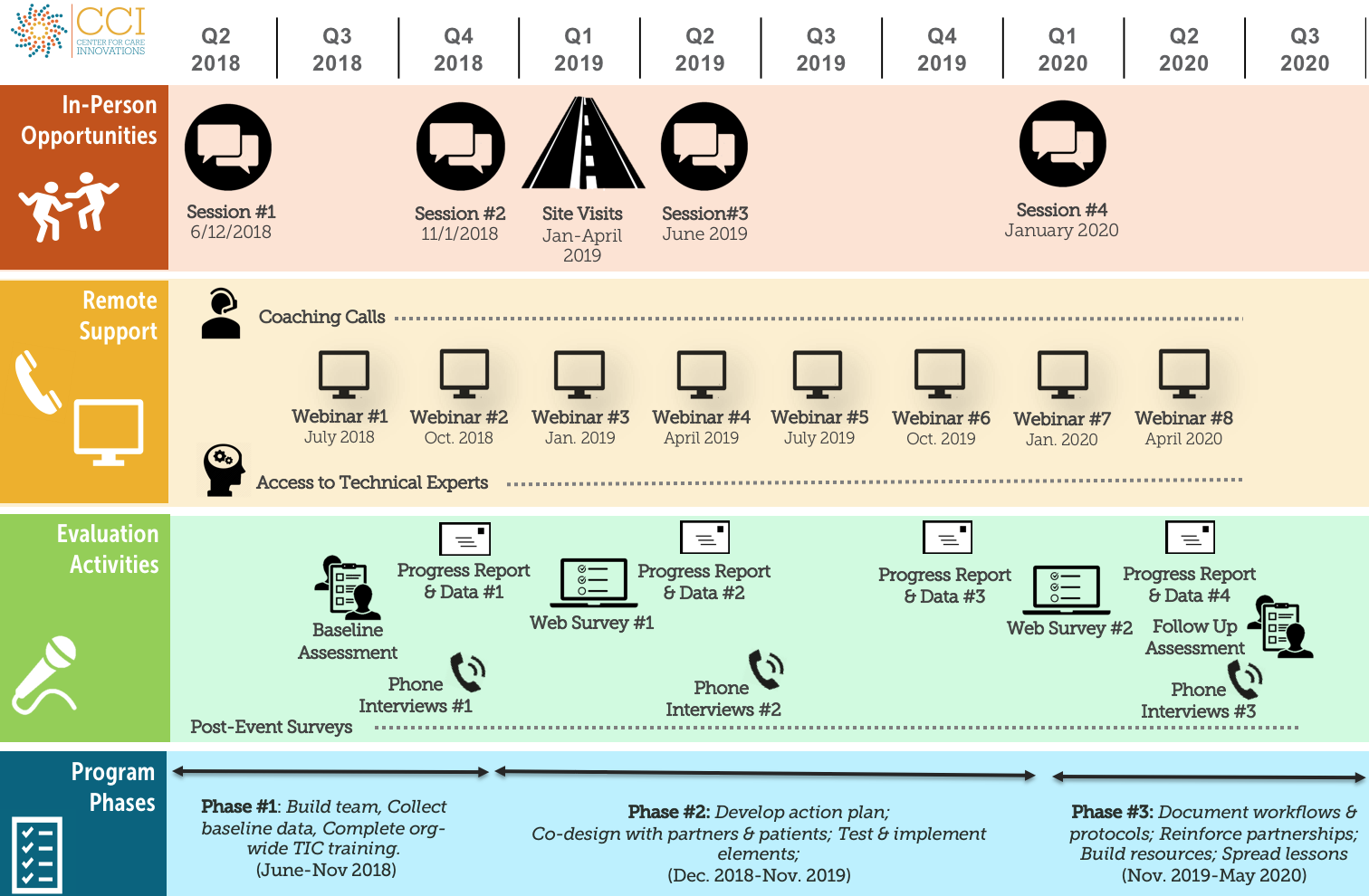
| Program Kickoff: | June 12, 2018 |
| Trauma-Informed Care Training: Updates, Answers, Inspiration | July 25, 2018 |
| Webinars: | Continuing through 2018 |
| Completion of Org-Wide TIC Training: | November 30, 2018 |
| In-Person Session 2: | November 1, 2018 |
| The Children’s Clinic Site Visit | March 18, 2019 |
| In Person Session 3 | May 15, 2019 |
| Montefiore Site Visit | June 13, 2019 |
Resources and reference material from CCHE, your evaluation team, will be posted here.
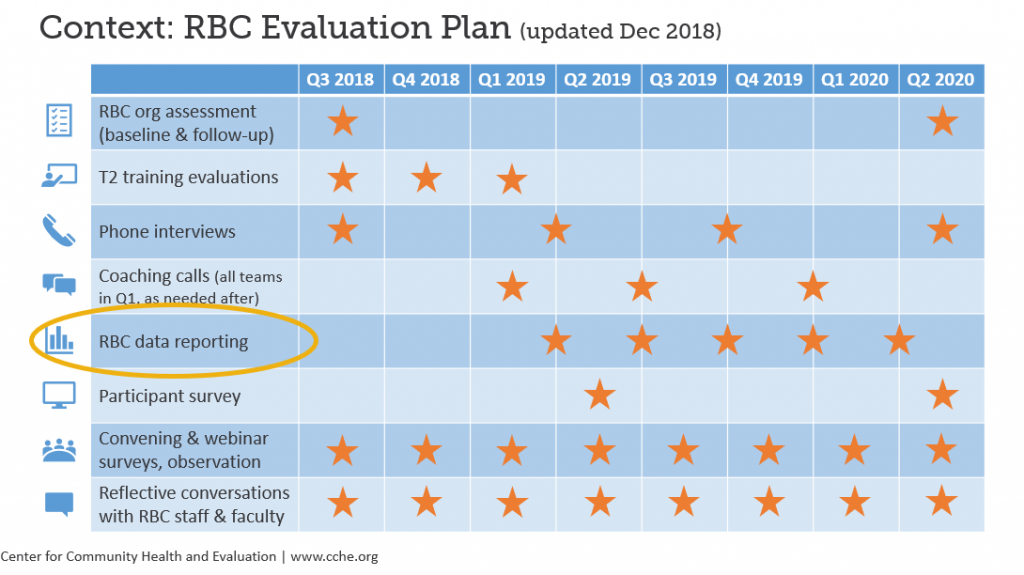
January 2019
CCHE provides an update on the evaluation plan and approach based on the baseline assessment and initial interviews.
August 2018
In this webinar, CCHE provided an introduction and explanation of the baseline assessment, explained the administration process, and built the case for why it’s important. CCHE also hosted a Q&A.