When it comes to mental health, a cookie-cutter approach leaves a lot to be desired. So even before the pandemic hit, community behavioral health centers often struggled with how to help as many clients as possible while providing quality care.
The problem: The demand for services frequently outstrips the clinics’ capacity. There are long wait times – sometimes for weeks or even months -- for patients who seeking appointments with therapists and psychiatrists.
The Jefferson Center, a nonprofit, community-focused behavioral health care and substance use services provider in Denver, was among those wrestling with such concerns. Jefferson Center serves a wide geographic area—from the west Denver area to more rural and mountain communities. Jefferson’s client base is also diverse: it serves clients of all ages from many different settings, including schools, senior residential housing, and law enforcement facilities. The nonprofit wanted to improve its approach in a way that would benefit both clients and staff -- the latter suffering from burnout. The center decided to pilot a program in which clients could schedule time or drop-ins to meet with whichever provider or providers best met their needs—a peer, case manager, therapist, nurse, or psychiatrist—whether for a brief check-in or a typical consultation. The goal of the pilot, launched in the spring of 2021 with 10 clients with depression, was threefold: to see a faster improvement in clients’ mental health status, to ease staff feelings of sole responsibility for a client, and to use data-driven approaches to make these shifts. The project was designed to allow staff the time and space to do more direct clinical care, and, in doing so, to build better relationships with the people they serve. The center also wanted to use data and new operational practices to better manage client caseloads. The project called on key human-centered design principles to guide its progress: the team started small, “learned fast,” and shared its work early and often—allowing for adjustments along the way. “This is exactly what I have wanted for so long,” one client told Jefferson Center staff, after learning that her fourth therapist was leaving after a short period of time. “[The pilot program] sounds really cool. Like it might work for me.”A New Phase with a Tested Model
Early in 2021, Jefferson Center created a virtual clinic, dubbed Phase Forward, inspired by the phase-based care approach on which the program was modeled. Once a week for an hour, a Jefferson Center team would meet to plan for the upcoming clinic and review who was expected to come in and their self-identified needs. Then, for two hours of clinic time, patients join an open Zoom call from which they are triaged to specific providers. Jefferson wanted to try the program with its own clients. The center decided that regional Medicaid members with a diagnosis of depression would provide the best launching point for the program. This was based on a desire to improve regional Medicaid performance. Jefferson also partnered with the technology consulting company Auptimal, which has a background in working with community mental health organizations, to create a dashboard that could help staff facilitate the program. The tech company’s consultant sat in on weekly team meetings to hear firsthand how staff discuss operations and clients. Changes to the dashboard were made based on how the team best works and manages clients. For instance, rather than listing patients alphabetically, the dashboard shifted to listing clients with the most acute mental health needs first, according to Amelia Spiegel, innovation analyst for the Jefferson Center.Facing Challenges, Changing Course
[caption id="attachment_27794" align="alignleft" width="380"] Downtown Denver[/caption]
Jefferson Center met several hurdles during the course of the project. Initially the organization intended to develop a remote patient monitoring (RPM) system. A technology platform, RPM, regularly engages with clients in between visits to a care professional, providing triage information back to the care team. The idea behind using remote patient monitoring is to provide staff with a way to manage changing complexities and risk with caseloads, with the goal of leading to improved clinical outcomes and reduced staff burnout.
But a major obstacle loomed early on. While RPM programs are relatively well suited to support clients with physical health conditions, these programs are less widely used with clients seeking behavioral health supports. Working with two RPM vendors required substantial time and resources on Jefferson Center’s end to educate these organizations on the behavioral health needs of a community mental health population. Adapting screening tools and alerts to best fit behavioral health clients also proved problematic.
So did Jefferson’s key goal of monitoring clients at risk for suicide. Ultimately, one vendor’s review board deemed Jefferson’s desire to monitor this high-risk group too, well, too high risk for their tastes. Another startup was bought out by a larger company, which decided to focus on a different aspect of healthcare. That proved an important learning curve, says Spiegel. It’s critical to vet the level of experience a vendor has within the behavioral health field before undertaking such a partnership, she says.
Downtown Denver[/caption]
Jefferson Center met several hurdles during the course of the project. Initially the organization intended to develop a remote patient monitoring (RPM) system. A technology platform, RPM, regularly engages with clients in between visits to a care professional, providing triage information back to the care team. The idea behind using remote patient monitoring is to provide staff with a way to manage changing complexities and risk with caseloads, with the goal of leading to improved clinical outcomes and reduced staff burnout.
But a major obstacle loomed early on. While RPM programs are relatively well suited to support clients with physical health conditions, these programs are less widely used with clients seeking behavioral health supports. Working with two RPM vendors required substantial time and resources on Jefferson Center’s end to educate these organizations on the behavioral health needs of a community mental health population. Adapting screening tools and alerts to best fit behavioral health clients also proved problematic.
So did Jefferson’s key goal of monitoring clients at risk for suicide. Ultimately, one vendor’s review board deemed Jefferson’s desire to monitor this high-risk group too, well, too high risk for their tastes. Another startup was bought out by a larger company, which decided to focus on a different aspect of healthcare. That proved an important learning curve, says Spiegel. It’s critical to vet the level of experience a vendor has within the behavioral health field before undertaking such a partnership, she says.
Solutions & Success
[caption id="attachment_27795" align="alignright" width="371"] Downtown Denver seen from City Park[/caption]
Despite these and other obstacles, Jefferson Center is buoyed by early results from the program. It expanded the clinic to include both new and existing patients, clients with primary diagnoses of primary depression or anxiety, and patients who qualified for care under any state funding. “So far the pilot is absolutely a success and we have more to do,” says Spiegel, who notes that clients scores for both primary depression and primary anxiety have improved in all but one person in the program. “For the client whose scores aren’t improving, that data is sparking conversations among a care team which otherwise would not have had the chance to work together to provide care to a client.”
In the past, another problem impacting all three key stakeholders (clients, staff, and the organization) is that care team members are siloed from each other. Typically in clinic settings, staff have a direct relationship with a client and do not communicate with other members of the patient’s care team. But this common concern if remedied, might be at the heart of solving problems faced by all three stakeholders—hence the Phase Forward approach. By creating a data-driven team-based approach, maybe caseloads could be better managed, and the feeling of sole responsibility for a client’s well-being diffused among staff members, explains Spiegel. “As far as staff satisfaction goes, through our interviews we learned that we are making improvements related to burnout,” she says.
In addition to how caseload assignments are made, historically there haven’t been clear guidelines and procedures for moving a client through levels of care, according to Spiegel. That’s especially true when a client is doing well, and would seemingly benefit from being seen less frequently, she explains. Phase Forward is designed to help both staff and clients move more efficiently through different level of care, using clinical observations, data-informed decision making, and client input.
The model, which focuses on a team approach, is designed around the concept that if a client has multiple people to potentially connect with who were informed about their mental health history—versus the standard one-on-one therapy model—perhaps the patient might be more likely to actively engage with and benefit from care.
In the future the center wants to focus on qualitative input from clients as well as improving the dashboard to inform strategic decision making and expansion. The idea is to roll out the clinic concept to existing clients and among other specialty groups, such as clients in family services or intensive services, and those who have experienced trauma or post-traumatic stress disorder.
Overall, Phase Forward is working, and there is good reason to be hopeful for the future of this program, says Spiegel, who notes at least one client who moved from the so-called acute phase of care to continuation after four weeks and is rapidly approaching a maintenance level of care.
“We are definitely trending up. It’s really nice to have multiple people bringing referrals and expertise,” says one Jefferson Center therapist. “I really appreciate that we have a peer specialist" on the team, she adds, noting that the person in this role frequently brings a lot of valuable information on a client to clinic meetings and helps inform treatment. “We are meant to meet a client where they are at.”
Sharing the client caseload among other team members has other benefits for staff in terms of avoiding burnout, including knowing there’s client coverage if a staff member is out for a day or unable to see a client at a specific time for whatever reason. “With a model like Phase Forward, where you are not the only person responsible for seeing a client, it makes it a lot easier,” she concluded.
Downtown Denver seen from City Park[/caption]
Despite these and other obstacles, Jefferson Center is buoyed by early results from the program. It expanded the clinic to include both new and existing patients, clients with primary diagnoses of primary depression or anxiety, and patients who qualified for care under any state funding. “So far the pilot is absolutely a success and we have more to do,” says Spiegel, who notes that clients scores for both primary depression and primary anxiety have improved in all but one person in the program. “For the client whose scores aren’t improving, that data is sparking conversations among a care team which otherwise would not have had the chance to work together to provide care to a client.”
In the past, another problem impacting all three key stakeholders (clients, staff, and the organization) is that care team members are siloed from each other. Typically in clinic settings, staff have a direct relationship with a client and do not communicate with other members of the patient’s care team. But this common concern if remedied, might be at the heart of solving problems faced by all three stakeholders—hence the Phase Forward approach. By creating a data-driven team-based approach, maybe caseloads could be better managed, and the feeling of sole responsibility for a client’s well-being diffused among staff members, explains Spiegel. “As far as staff satisfaction goes, through our interviews we learned that we are making improvements related to burnout,” she says.
In addition to how caseload assignments are made, historically there haven’t been clear guidelines and procedures for moving a client through levels of care, according to Spiegel. That’s especially true when a client is doing well, and would seemingly benefit from being seen less frequently, she explains. Phase Forward is designed to help both staff and clients move more efficiently through different level of care, using clinical observations, data-informed decision making, and client input.
The model, which focuses on a team approach, is designed around the concept that if a client has multiple people to potentially connect with who were informed about their mental health history—versus the standard one-on-one therapy model—perhaps the patient might be more likely to actively engage with and benefit from care.
In the future the center wants to focus on qualitative input from clients as well as improving the dashboard to inform strategic decision making and expansion. The idea is to roll out the clinic concept to existing clients and among other specialty groups, such as clients in family services or intensive services, and those who have experienced trauma or post-traumatic stress disorder.
Overall, Phase Forward is working, and there is good reason to be hopeful for the future of this program, says Spiegel, who notes at least one client who moved from the so-called acute phase of care to continuation after four weeks and is rapidly approaching a maintenance level of care.
“We are definitely trending up. It’s really nice to have multiple people bringing referrals and expertise,” says one Jefferson Center therapist. “I really appreciate that we have a peer specialist" on the team, she adds, noting that the person in this role frequently brings a lot of valuable information on a client to clinic meetings and helps inform treatment. “We are meant to meet a client where they are at.”
Sharing the client caseload among other team members has other benefits for staff in terms of avoiding burnout, including knowing there’s client coverage if a staff member is out for a day or unable to see a client at a specific time for whatever reason. “With a model like Phase Forward, where you are not the only person responsible for seeing a client, it makes it a lot easier,” she concluded.
Lessons Learned
Take the time to define roles, responsibilities, and expectations.
Roles, responsibilities, and expectations are especially critical for productive working relationships within the project team and with supervisors of clinic staff. If the center had given more time and attention to this, project leaders believe they may have avoided the small amount of clinic staff turnover it did experience.Involve frontline staff from the get-go.
Frontline staff have excellent ideas and are resilient – involve them sooner rather than later in the process. This can make for smoother transitions regarding responsibilities and help a clinic meet stated principles, such as challenging the status quo and organizational hierarchy. Involving clinic staff early in the process can also help to empower them to make their own decisions within an operational framework.Keep the focus on the problem, not the solution.
Clearly identify the problem—in this case overwhelming caseloads and clients stuck waiting for treatment—to help generate possible solutions and prototypes to solve a complex problem.Identify appropriate technology partners to help achieve goals.
Buyer beware: Startup companies are inherently volatile. In Jefferson’s case, the tech entity that helped on the design phase with screening tools and alert systems was acquired by a larger company that was not interested in pursuing clients in the mental health market. Choose to work with such companies with caution, and perhaps outside the constraints of funded grants.Next Steps
- Define and refine clinic staff roles and responsibilities.
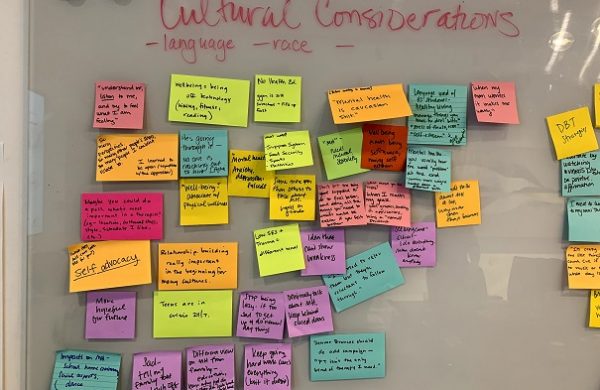
- Hold a whiteboarding brainstorm session with clinic staff with the goal to build trust, generate ideas, and plan for the future.
- Expand clinical team to combat turnover.
- Experiment with ways to introduce patients to members of the care team to develop and strengthen relationships.
- Refine task board and dashboard for maximum efficiency.
- Create formal triage and handoff procedures.
- Focus more on patient experience and satisfaction. ______________________________________________________________________________ The Jefferson Center for Mental Health is part of a CCI collaborative designed to support innovation to better address the health of historically underserved Coloradan communities. The Colorado Health Innovation Community (CHIC) helps health care safety net organizations identify, test, and evaluate new approaches with the potential to improve care experiences for low-income Coloradans. The program draws on human-centered design and sustainable solutions for patients and staff alike, with an emphasis on technological innovation that can help strengthen health and health care. JCMH is one of seven clinics in the cohort, including Clinica Family Health, Every Child Pediatrics, Jefferson Center for Mental Health, Mental Health Center of Denver, Melissa Memorial Hospital, Solvista Health, and STRIDE Community Health Center. Partners on the project include Colorado Health Foundation, The Colorado Health Access Fund of the Denver Foundation, Rose Community Foundation, Community First Foundation, and Colorado Access.