With the rapid expansion of telemedicine in light of the COVID-19 pandemic, ensuring that remote care reaches diverse, low-income patients and promotes health equity, rather than exacerbating health disparities, is critical. Through a partnership between the Center for Care Innovations, UCSF’s Center for Vulnerable Populations (CVP), and the Commonwealth Fund, we have developed this toolkit to provide background information as well as concrete guidance relevant to safety-net healthcare systems looking to initiate, expand, or improve their telemedicine programs.
This toolkit focuses on telemedicine, which the Health Resources Services Administration defines as referring to remote clinical services such as phone and video visits, remote patient monitoring, patient portals, and mobile health.
The toolkit was originally published in October 2020 and was refreshed in June 2021. In the June 2021 refresh, we have added new evidence regarding equity in telemedicine uptake among diverse patient populations, as well as new resources regarding reimbursement. In addition, we have integrated “Tools from the Field” — scripts, workflows, and other concrete tools from safety-net healthcare sites participating in CCI’s Connected Care Accelerator. We hope that sharing these concrete tools will help to disseminate best practices and inspire continued testing and improvement of telemedicine programs as sites adapt these resources to meet their on-the-ground needs.
In addition to this more action-oriented toolkit, we have also expanded upon CCI’s COVID-19 Resource Wiki with information-oriented resources from our research.
If you find that we have missed a key resource on telemedicine implementation in safety-net healthcare settings, please let us know by sending an email to [email protected].
Toolkit Chapters
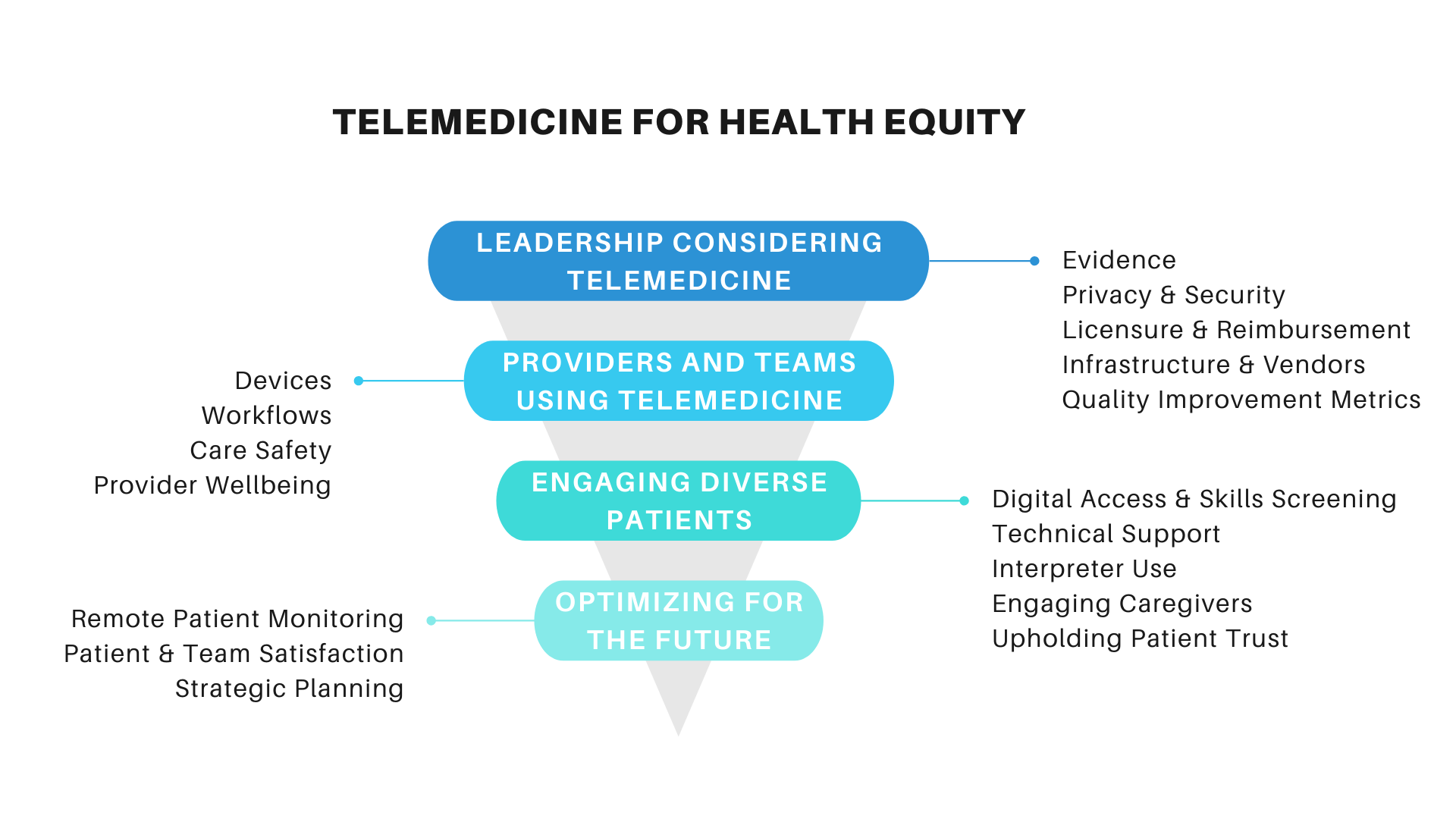
Considerations for Leadership Before Implementing TelemedicineWe summarize the basic components of telemedicine implementation for health care system leaders. These topics are important in safety-net settings that already face challenges related to limited resources and fragmented health information technology.
|
|
Considerations for Providers and Teams in Using TelemedicineOnce the decision to integrate telemedicine into routine care delivery is made, frontline care teams must begin to deliver telemedicine efficiently, safely, and equitably. We look at key considerations for frontline teams.
|
|
Considerations for Reaching and Engaging Diverse PatientsCentral to effective and equitable in telemedicine care is engaging a diverse patient population. We review some of the most pressing areas of consideration to ensure telemedicine does not worsen existing health disparities.
|
|
Optimizing Telemedicine for the FutureAs we continue to scale telemedicine approaches in the COVID-19 pandemic and beyond, there will be many advanced features that can be implemented and optimized for safety-net settings, including remote patient monitoring, assessing patient and team satisfaction, and population health management.
|
→ Want a more searchable and tagged version of this toolkit? Check out the Virtual Care Learning Hub!
Supported by The Commonwealth Fund, a national, private foundation based in New York City that supports independent research on health care issues and makes grants to improve health care practice and policy. The views presented here are those of the author and not necessarily those of The Commonwealth Fund, its directors, officers, or staff.





