Among the many provisions of the Affordable Care Act, one of the most intriguing – and confusing – is that health care providers should move toward providing “health homes” for their patients. What does that mean in practice?
It’s certainly not an image that immediately resonates with most consumers, particularly those who have traditionally sought care from the health care safety net. To gain insight into how patient-centered models of care are emerging in the safety net, we talked with more than 30 innovative providers and payers around the country. Here’s what we learned.
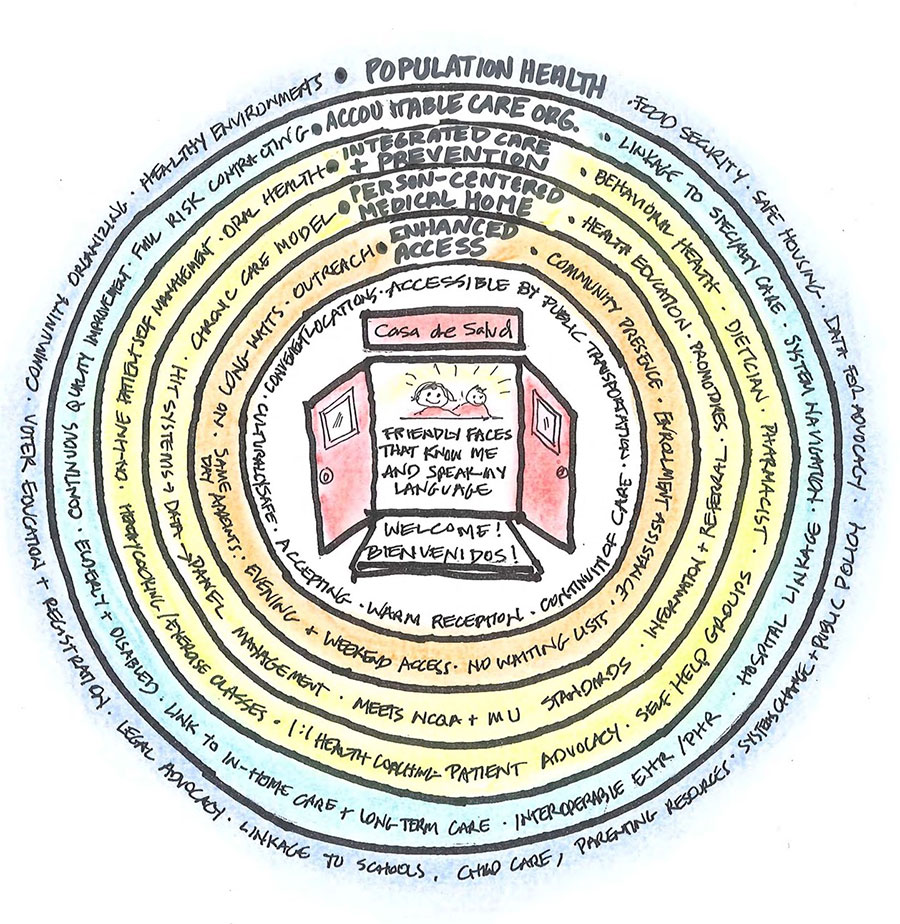
A variety of concepts have been proposed, ranging from “patient-centered medical homes” to “person-centered health homes” to “community-centered health homes,” to name but three. Although they all share many of the same qualities, for now we prefer the more generic image of a Health Home.

In our view, Health Home projects a more expansive view of health promotion and improvement than more physician-centric medical home concepts. It also acknowledges that medical care alone will be insufficient to ultimately achieve health equity for underserved populations. Patient and family engagement and self management are seen as essential complements to clinical interventions. A Health Home prioritizes the voice of the patient and sees culturally-proficient prevention and primary care as the cornerstone for an integrated system of care.
How do we get there from here? Fortunately, there is much experience and wisdom around the country to draw on. Excellent assessment tools and resource guides have already been developed to aid practice transformation through the efforts of The Commonwealth Fund’s Safety Net Medical Home Initiative. Many valuable lessons have been learned about the complex challenges of implementing Electronic Health Records and reconfiguring practice teams and workflow. There’s no need to reinvent those wheels!
But we’ve been struck by how often the discussion among professionals jumps over the question of what “person-centeredness” might look like from a consumer perspective to detailed prescriptions for redesigning practice from a provider perspective. The focus also tends to be on primary care rather than on connecting different providers and resources into an easy-to-navigate system of care. Prevention and social determinants of health are also rarely part of the conversation.
To try and integrate all these potential pieces into a single image of a Health Home, we developed this diagram. Part of the problem in talking about Health Homes is that we believe all these concepts are often floating around the conversation –acknowledged or unacknowledged — at least among professionals. But when most consumers think about what they’d want in a Health Home, we suspect that the innermost circle (or two) is often what they’re talking about.

The center of the diagram portrays the doorway to the Health Home from a consumer perspective. What are they looking for? They would likely prioritize the following: respect in all interactions; friendly faces who know me and speak my language; convenient, attractive locations and hours; and a personal relationship with a provider they trust. The next circle out (Enhanced Access) is often thought of as a “higher order” change by providers, but is very salient for consumers. Just like privately-insured patients, they want same-day appointments, after-hours access to urgent care and an advice line or online connection, and no long waits when they come in for care.
The next circle out (Person-Centered Medical Home) is where most of the energy of providers is going in innovative practices. It builds on the principles of teaming, panel management and patient self care inherent in the Chronic Care model, informed by appropriate HIT systems such as Electronic Health Records.
The fourth circle, “Integrated Care and Prevention,” takes the basic PCMH model to a higher level of integration, incorporating behavioral health, oral health, and other special resources such a dietician and pharmacist in the primary care setting. It also promotes wellness and patient self care via support groups, one-on-one coaching and exercise and cooking classes. Significant effort is devoted to health education, including the use of innovative technologies to facilitate patient self management at home or at work.
We have appropriated the “Accountable Care Organization” label for the fifth circle, to signify the importance of connecting primary care settings to specialty care, hospitals and other elements of the health care system in as seamless a fashion as possible. This has long been a gaping hole in most communities’ Safety Net. Just exchanging data among clinics and hospitals has been impossible most places. From a consumer perspective, ease of navigation of these elements of the system is key… and highly problematic at present. The interoperability, shared risk and accompanying financial incentives integral to the ACO concept will need to be put in place on a regional level if the Health Home concept is to be financially sustainable.
 Finally, medical care and patient self management alone will not be sufficient to advance health. It will take a shared commitment to primary prevention, including healthy environments, access to healthy food and safe housing as well as advocacy to address other social determinants of health and wellness to achieve the ultimate goal of providing a true Health Home.
Finally, medical care and patient self management alone will not be sufficient to advance health. It will take a shared commitment to primary prevention, including healthy environments, access to healthy food and safe housing as well as advocacy to address other social determinants of health and wellness to achieve the ultimate goal of providing a true Health Home.
We have used this diagram as the starting point for a two-year grantmaking program we are calling the Health Home Innovation Fund. With funding from The California Endowment, we are supporting ten partnerships around California to build Health Homes for their local safety net populations.
We recognize that the fully-developed Health Home we have just described remains an aspirational goal at present. But regardless of the eventual fate of the ACA, the stage has been set for fundamental change in the way American health care is organized and financed. As a wise person observed at one of our recent meetings, “everyone’s business model is up for grabs.” Just as market forces are driving consolidation across the for-profit landscape, we believe it’s essential that the organizations comprising the health care Safety Net seize this opportunity for experimentation and innovation. If we are to ever achieve the goal of health equity and also bend the cost curve, the time has come to connect its disparate elements into a truly integrated system of care.